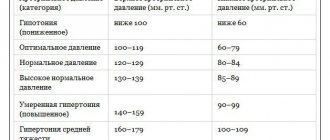
1. Diagnosis of high blood pressure
Diagnosis of high blood pressure, or hypertension, involves taking a medical history and directly examining the patient. Your doctor's specific questions and tests will depend on how high your blood pressure is and whether you have other risk factors for heart disease. Some patients may require more detailed diagnostic testing or even a comprehensive cardiac evaluation.
To diagnose hypertension, your doctor may:
- Ask about your family history of hypertension, assess risk factors for high blood pressure - for example, heredity or smoking.
- Measure your blood pressure two or more times. Measurements can be taken on the left or right arm, on the leg and, for example, in different positions - sitting, lying or standing. This will help you get a more accurate idea of your blood pressure.
- Measure your weight, height and waist circumference.
- Check the retina and the condition of the back of the eye.
- Check your heart function (at a minimum, listen to the rhythms).
- Examine the abdomen with a stethoscope. Listening to the vessels in the abdomen will help you hear abnormal sounds, which may be caused by obstruction of blood flow due to a narrowing of the artery in the abdomen.
- Examine the neck to detect an enlarged thyroid gland, distension of the jugular veins and carotid artery.
A must read! Help with treatment and hospitalization!
We get tested
General blood test (every three months) .
This is necessary to determine the level of hemoglobin and ESR. Damage to the renal vessels is accompanied by a decrease in hemoglobin levels, and any inflammation, including the vascular wall, is reflected by an increase in the erythrocyte sedimentation rate (ESR). It would also be useful to evaluate the number of leukocytes - markers of the inflammatory process during infections. The fact is that the presence of infection in the body may lead to the need to adjust the treatment of hypertension. Article on the topic Heart attack season.
How to support your heart Determination of cholesterol levels (every six months) .
High blood cholesterol levels are a risk factor for heart attacks and strokes. If the level of total cholesterol is elevated, you need to undergo a more in-depth analysis - for one of the fractions of cholesterol, low-density lipoproteins (LDL). After assessing cholesterol levels, the doctor decides whether to prescribe special cholesterol-lowering drugs - statins. Biochemical blood test (once a year) . It is needed to assess the level of creatinine, a special protein secreted by the kidneys. The fact is that the kidneys are one of the main organs that regulate blood pressure, and kidney diseases can cause severe hypertension. But the kidneys themselves are a target organ for high blood pressure. If the kidneys are not working well, the concentration of creatinine levels in the blood increases. In addition, it is necessary to evaluate the level of uric acid, which can be deposited in the kidneys and cause severe hypertension. Another important indicator is potassium level. High potassium may occur in patients with kidney failure; low potassium often indicates that the patient is not using diuretics correctly to lower blood pressure.
General urine test with determination of microalbuminuria (every three months) . Albumin is a protein whose presence in a urine test indicates serious kidney damage.
Determination of glucose (every six months) . This analysis will help you not to miss the development of diabetes. The fact is that hypertension often accompanies this disease.
Click to enlarge
4. Other examination results for arterial hypertension
During the appointment, the doctor can check whether high blood pressure has caused damage to other organs - blood vessels, heart or eyes. Unusual heart sounds when listening, swollen neck veins (this may indicate heart failure), swelling of the arms and legs, and vascular abnormalities in the back of the eye can indicate various health problems. This means that additional examinations may be necessary.
What should you think about?
The diagnosis of hypertension, or high blood pressure, is usually made based on the average of two or more readings obtained during two or more doctor visits. But in very severe cases, one visit is enough. Self-measurement of blood pressure can also help in diagnosis. Some people are nervous before visiting the doctor, and their blood pressure rises. This means that the picture may not be entirely objective. But if you measure your blood pressure at home and then report the data to your doctor, it can be very helpful in accurately diagnosing hypertension.
High blood pressure: examination algorithm
Arterial hypertension can be either an independent disease or a symptom of another pathology. To understand, it is necessary to correctly prescribe tests and instrumental research methods.
Examination of a patient who complains of increased blood pressure has two goals. The first, as mentioned above, is to determine what we are dealing with: hypertension or symptomatic hypertension. The second is to find out whether a person has target organ damage or whether hypertension is “without consequences.”
The main “sources” of symptomatic hypertension are the heart, kidneys, endocrine system, brain and large vessels. The list partially overlaps with the list of target organs: heart, kidneys, brain, eyes, blood vessels. The doctor will focus on the condition of these parts of the body.
Examination of the heart and great vessels
The basis of heart examination is ECG, and examination of hypertensive patients is no exception. Pressure can increase with various arrhythmias, the presence of which the patient is not always aware of, and a cardiogram or Holter is the best way to identify rhythm disturbances. In addition, the doctor will prescribe an ECHO-CG - patients usually call it “ultrasound of the heart.” This study shows both disturbances in the structure of the heart (various valve defects, etc.) and a decrease in its function, i.e., it helps to diagnose heart failure (HF).
Treatment and prevention of hypertension
Prevention of hypertension consists of lifestyle adjustments, preventive examinations to identify possible failures that are prerequisites for hypertension, and their surgical treatment.
Drug treatment includes taking several groups of medications. Can be assigned:
- ACE inhibitors;
- calcium antagonists;
- angiotensin 2 receptor antagonists;
- diuretics;
- beta-adrenergic antagonists;
- alpha-blockers;
- means of central action;
- combination drugs (combination of several substances in one drug).
At SM-Clinic you can undergo a preventive examination to timely identify possible problems with blood pressure and receive qualified treatment for any type of hypertension.
Other studies
ECG (every six months) . It is necessary to monitor the heart rate and rhythm, and assume an increase in the size of various parts of the heart. Due to increased blood pressure, the main chamber of the heart, the left ventricle, begins to thicken, this is called left ventricular hypertrophy. In a hypertrophied heart, rhythm disturbances are more likely to occur, and heart failure may occur due to heavy workload.
Ultrasound of the carotid arteries (once a year) . If the doctor sees thickening of the wall of the carotid artery, this indicates that the condition of the blood vessels is changing, an atherosclerotic plaque begins to form, which means the risk of stroke increases.
Examination by an ophthalmologist (once a year) . The eyes also suffer from high blood pressure. Severe hypertension can cause damage to the retina, optic nerve, and blood vessels in the eyes.
Where does the disease come from?
The cause of hypertension is still unknown. A number of people have a hereditary predisposition to hypertension.
In addition to unfavorable heredity, there are other factors for the development of arterial hypertension. These include excessive consumption of table salt, obesity, and stress.
The above factors contribute to a greater extent to the development of hypertension in persons with unfavorable heredity.
The main causes of secondary arterial hypertension are bilateral (less often unilateral) tissue damage. Diseases of a number of endocrine glands, such as the pituitary gland, adrenal glands and thyroid gland, can also lead to the development of secondary arterial hypertension.
Arterial hypertension is dangerous precisely because of its complications, which can often be fatal. If it did not cause such complications, then arterial hypertension itself would not arouse such interest. Indeed, of all the unpleasant sensations that are characteristic of high blood pressure, only a headache can be noted.
The presence of arterial hypertension causes the development of a number of changes in the body of its owner. As a rule, these changes develop gradually. In a stable course of arterial hypertension, the severity and reversibility of these changes are directly dependent on the duration of the disease, as well as on the level of persistent increase in blood pressure. First of all, long-term arterial hypertension (without appropriate treatment) leads to changes in the structure and properties of the arterial wall throughout the body.
As a result of a series of transformations, the vascular wall loses its inherent elasticity, becoming dense and brittle, facilitating hemorrhages. The arteries of the kidneys, brain, fundus and limbs suffer the most from a persistent increase in blood pressure. Arterial hypertension accelerates the processes of premature aging of the arterial wall (atherosclerosis) throughout the body, being a risk factor for the development and progression of coronary heart disease (CHD).
Thus, arterial hypertension is accompanied by various complications and concomitant diseases. Among them:
- Atherosclerosis
. Arterial hypertension can be a risk factor for atherosclerosis, a disease in which there is a high level of low- and very low-density lipoproteins (cholesterol) in the blood, as well as the formation of atheromatous plaques on the walls of blood vessels. And this, in turn, contributes to the further development of arterial hypertension. - Heart diseases
. Arterial hypertension increases the risk of myocardial infarction, as it is a risk factor for atherosclerosis, and also contributes to the narrowing of the coronary arteries that supply blood to the heart muscle. - Diseases of the central nervous system
. These include conditions such as stroke, chronic cerebrovascular accident, etc. - Kidney diseases
. Arterial hypertension is one of the main causes of kidney diseases, including renal failure, which is associated with impaired blood circulation in them. - Visual impairment.
Arterial hypertension is accompanied by impaired blood circulation in the retina, as well as the optic nerve (the nerve also receives nutrition from very small arterioles). - Diabetes.
Arterial hypertension is a risk factor for many complications of diabetes, for example, diabetic foot, retinopathy (retinal pathology), etc. - Preeclampsia
is a condition characteristic of pregnant women with symptoms of gestosis (toxicosis). Hypertension may be a sign of this serious complication. - Metabolic syndrome.
This is a group of conditions associated with obesity, increased blood pressure, increased blood sugar, and the risk of myocardial infarction and stroke. - Erectile disfunction.
The insidiousness of arterial hypertension (hypertension)
It also lies in the fact that it is often asymptomatic; even with high blood pressure (BP), the patient’s health can remain good. This is the reason for the negative attitude towards medical recommendations.
But feeling well with high levels of arterial hypertension (hypertension) does not protect the patient from the dangerous complications of this disease. Every patient suffering from arterial hypertension (hypertension) must understand that a long-term and sustainable decrease in blood pressure improves the quality of life and reduces the risk of developing vascular complications: by 45% - the number of strokes and by 38% - the number of myocardial infarctions.
Diagnostics that detect malfunctions in the cardiovascular system:
- Electrocardiogram (ECG);
- Angiography (detecting the presence of blood clots);
- Echocardiography (study of functional changes in the heart and its valve apparatus);
- Blood pressure monitoring (an effective method for diagnosing hypertension);
- Cardiorisk (determines the degree of development of heart disease);
Using the above diagnostic methods, diseases such as coronary heart disease, heart failure, congenital and acquired heart defects, various types of arrhythmia, inflammatory lesions on the heart muscle (carditis), thrombophlebitis and thrombosis, aortic aneurysms, angina pectoris, heart attacks and pre-infarction condition are detected.
If abnormalities in the functioning of the cardiovascular system are detected, you must consult a cardiologist, take the necessary tests and undergo a full diagnosis.