Causes of cerebral circulatory disorders
The brain is the main organ of the central nervous system; it consists of neurons united by synaptic connections. By interacting with each other, neurons form chains of electrical impulses that regulate the activity of the body1.
The functioning of the brain requires large amounts of energy, which it receives through the bloodstream. Blood enters the brain through four arteries - two carotid and two vertebral, and outflow - through two jugular veins. With an average weight of 2% of the total body weight, the brain at rest consumes 15% of all blood circulating in the body, 20-25% of the oxygen received during respiration, and up to 50% of all glucose reserves entering the blood from the liver2.
Blood supply to the brain and blood circulation within the organ play a crucial role in its functioning, since without the provision and distribution of energy, oxygen, vitamins and amino acids entering the bloodstream, neurons cannot grow and divide. 85% of all pathologies associated with brain function are due to circulatory disorders3. Improving blood circulation in the brain is necessary for any pathologies and conditions that can lead to vasoconstriction or impaired blood circulation within the organ.
Pathological causes of vasoconstriction and their consequences:
- Arterial hypertension. In response to increased blood pressure, the walls of blood vessels spasm, and additional layers grow on the inside of the vessels. Thickening impairs blood flow4,5,6.
– Hypercholesterolemia. Violation of lipid metabolism in the direction of increasing low-density lipoproteins (“bad cholesterol”) leads to the formation of atherosclerotic plaques on the walls of blood vessels. Plaques completely or partially block a vessel, disrupting blood circulation, including in the brain7.
– Thrombosis. The formation of a thrombus (a clot of coagulated blood) can have various origins, as a rule, these are damage and cracks in the walls of blood vessels. Blood clots lead to blockage of blood vessels and increase blood viscosity, impairing blood circulation to the brain8,9.
- Diabetes. With increased levels of glucose in the blood, thickening of the vascular walls is stimulated, which leads to disruption of the natural flow of blood, and blood supply to the brain is disrupted10,11.
– Osteochondrosis of intervertebral discs. The vertebral artery is one of the main vessels through which blood flows to the brain. With pathology of cartilage tissue, intervertebral discs compress this artery, disrupting the blood supply to the brain12,13.
- Cardiopsychoneurosis. This is a complex of disorders of the cardiovascular system that can lead to disturbances in blood supply and circulation in various organs, including the brain14,15.
Impaired blood circulation in the brain can result from traumatic brain injuries, including concussions and bruises, as well as traumatic injuries to the spine, accompanied by impaired blood flow.
Neurocirculatory dystonia in the context of cerebral circulatory disorders is considered separately. The difficulty is that this disease often does not have an acute phase, and its main symptoms without targeted diagnosis can be explained by a number of typical pathologies such as chronic fatigue syndrome16. In other words, many simply do not know that they have this disease (sometimes called a syndrome in the medical literature).
Symptoms of neurocirculatory dystonia are nervousness, increased fatigue, sleep disturbances, weakness, impaired cognitive function, and subsequently palpitations, cardialgia, shortness of breath, and blood pressure disorders. In the future, it leads to arrhythmia, tachycardia, and chronic vascular insufficiency. All these symptoms are explained, among other things, by impaired blood circulation in the brain17.
Reasons for the development of neurocirculatory dystonia18:
– genetic predisposition;
– psycho-emotional stress;
– lack of sleep (inconsistency with circadian rhythms);
– lack of physical activity;
– unbalanced diet, obesity;
– alcohol abuse, smoking.
That is, lifestyle directly affects the development of neurocirculatory dystonia, which leads to chronic cerebral circulatory disorders. Under conditions of lack of oxygen and nutrients, the rate of formation of neurons decreases, connections between control departments, as well as the transmission and inhibition of nerve impulses within the central nervous system are disrupted.
As a result, memory, concentration, reaction and coordination of movements deteriorate, constant fatigue and drowsiness are observed, and performance drops to 50%19. This condition can lead to massive death of brain cells and the appearance of local foci of necrosis. That’s why improving blood circulation in the brain is vitally important; let’s look at how to do it point by point.
Treatment
If there are diseases such as hypertension, diabetes mellitus or other diseases, then, first of all, it is necessary to compensate for the underlying disease.
To treat chronic cerebrovascular accidents, various medications are used - vascular drugs (Trental, Cavinton, Sermion, etc.), nootropics, metabolic drugs, antioxidants. To prevent the formation of blood clots, antiplatelet agents such as aspirin, dipyridamole are prescribed. For high cholesterol levels in the blood Statins may be used.
Sometimes surgical treatment is required to eliminate the blood flow disorder - for example, carotid endarterectomy. Treatment methods such as carotid angioplasty and stenting are also used.
We improve blood circulation in the brain - sufficient and complete sleep
According to research, the duration of proper sleep is 7-8 hours per day20. Sleep should be regular - that is, it is recommended to fall asleep and wake up at approximately the same time. It is necessary to sleep in absolute darkness and silence, so the brain can fully analyze and systematize the information received during the day, as well as update the neurochemical mechanisms responsible for long-term memory21.
Research shows that adequate sleep normalizes blood circulation in the brain, ensuring adequate daily intake of oxygen and nutrients by brain cells. Lack of sleep, on the contrary, impairs blood supply to the brain and blood circulation, leads to the death of neurons and extensive damage to the central nervous system (including disruption of the function of the blood-brain barrier, which protects the brain from infections and toxins that can enter it through the blood)22,23. Therefore, in order to improve blood circulation in the brain, you must first normalize sleep; without this measure, other methods will be less effective.
Symptoms
Symptoms of a cerebrovascular accident depend on the degree of damage to brain cells and the location of the area of the brain with impaired blood flow. In acute cerebrovascular accidents (hemorrhagic or ischemic stroke), movement disorders such as hemiplegia or hemiparesis develop.
In chronic cerebral circulatory disorders (also called discirculatory encephalopathy), symptoms develop gradually and are manifested by symptoms such as memory impairment, dizziness, headaches. At first, the patient does not have any impairment of intellectual abilities. But as there is a chronic lack of oxygen in the brain tissue, memory impairment begins to progress, personality disorders arise, and intelligence decreases significantly. Subsequently, the patient develops severe intellectual-mnestic and cognitive impairments and dementia develops; extrapyramidal disorders and cerebellar ataxia may also develop.
Improving blood circulation in the brain - diet and drinking regimen
A diet to improve blood circulation in the brain is selected based on the metabolic characteristics and condition of a particular person. Before adjusting the diet, it is recommended to conduct the following studies: daily blood pressure monitoring, blood tests for glucose and cholesterol, and a coagulogram. Based on research results, it is necessary to adjust the amount of salt, sugar, animal fat and other products in the diet24,25,26.
Diet recommendations to improve blood circulation in the brain:
– The consumption of salted, smoked and canned foods is usually limited in the presence of arterial hypertension, based on the recommendation - no more than 4.5 grams of salt per day.
– Restrictions on the amount of animal fat (fatty meat, lard, milk, butter) are determined by the presence of hypercholesterolemia, which sets the upper limit - 1 gram of fat per 1 kg of weight.
– The amount of monosaccharides and disaccharides (glucose, sucrose and foods high in them) is limited when blood glucose is high. In this case, preference is given to polysaccharides, which are found, for example, in durum cereals and pasta.
– Since vitamin K actively stimulates blood clotting, if this indicator increases, it is recommended to limit all foods high in vitamin K (white cabbage, broccoli, spinach, lettuce, soy, eggs, dairy products, green tea).
Research shows27 that foods high in sodium reduce central perfusion pressure, which measures the level of blood flow to the brain. In this regard, outside of pathologies, it is recommended to avoid excessive consumption of foods high in sodium - salt, herring, caviar, almost all cheeses, beef kidneys, feta cheese, dry cream, powdered eggs.
Chronic cerebrovascular insufficiency
Etiology and pathogenesis
Chronic cerebrovascular insufficiency (CVI) is the most common variant of vascular-cerebral pathology (in foreign literature there is an illogical term “cerebrovascular diseases”, which can be used in cases where the brain is primarily affected and the innervation of the vascular system is secondarily disrupted with clinical disorders, for example, the neurogenic stage of hypertension, vegetative-vascular dystonia, etc.). The most common etiological factors of vascular damage are atherosclerosis, hypertension and their combination, diabetes mellitus, vegetative-vascular dystonia, vasculitis in systemic connective tissue diseases (lupus erythematosus, etc.), syphilis, tuberculosis, blood diseases with an increase in its viscosity (erythremia , macroglobulinemia, etc.).
The following stages of chronic cerebrovascular insufficiency are distinguished: initial manifestations of cerebral circulatory failure and dyscirculatory encephalopathy.
Initial manifestations of cerebrovascular insufficiency (CBF)
develop when the cerebral blood flow rate decreases from 55 ml/100 g/min (normal) to 45-30 ml/100 g/min. Clinical symptoms (complaints) are short-term dizziness and feelings of instability when walking or sudden changes in body position, a transient feeling of heaviness in the head, increased fatigue, decreased speed of thinking and memory, and sleep disorders. From time to time headaches and noise in the head appear. Such symptoms first occur after physical or emotional stress, alcohol consumption, hunger, or changes in meteorological factors.
When examining the neurological status, signs of focal damage to the nervous system are not detected. Neuropsychological examination reveals a slowdown in thinking when solving intellectual problems, and mild impairment of cognitive functions.
Encephalopathy
is a multifocal brain lesion due to a decrease in blood flow to the brain ranging from 35 to 20 ml/100 g/min. Typically, discirculatory encephalopathy (DE) develops against the background of general vascular pathology. The following forms are distinguished: atherosclerotic, hypertensive, venous and mixed.
Based on the severity of neurological disorders, 3 stages of dyscirculatory encephalopathy are distinguished.
Stage I is characterized by a decrease in attention, memory (primarily for current events - memorization of new information is impaired), increased fatigue, and decreased ability to work. new information), increased fatigue, decreased ability to work. It is difficult for the patient to concentrate and switch from one activity to another. There is a dull headache, which intensifies with prolonged mental stress and excitement. Sleep is disturbed. Periodically, dizziness and staggering occur when walking. Emotional lability and decreased mood are observed.
When examining the neurological status, revival of reflexes of oral automatism, anisoreflexia of deep reflexes in the arms and legs are revealed against the background of their moderate increase without a decrease in muscle strength, moderate impairments of attention and memory. Working capacity has been preserved.
In stage II , personal changes appear in the form of viscosity of thinking, getting stuck on trifles, selfishness, touchiness, irritability, narrowing the range of interests and needs; Memory disorders increase, the ability to generalize and abstract, and associative thinking decreases. It is difficult to fall asleep, sleep is short and intermittent. Patients often complain of a dull headache, darkening of the eyes with a sudden change in the position of the body and head, dizziness, and instability.
In the neurological status, along with pseudobulbar signs and anisoreflexia, akinetic-rigid syndrome and vestibulo-cerebellar disorders are detected. Working capacity and social adaptation decrease.
Stage III is characterized by worsening symptoms and signs of the previous stage. Signs of pseudobulbar paresis, pyramidal insufficiency with decreased muscle strength, extrapyramidal and cerebellar dysfunction are increasing. Criticism towards one's own state decreases, weakness of spirit (tearfulness) is noted. Control of the sphincters of the pelvic organs is impaired. Cognitive disorders become severe to the point of dementia, and the development of apato-abulic syndrome and epileptic seizures is possible. There is severe drowsiness after eating (pollakihypnia; from the Greek pollakis - often, hupnos - sleep). Headache, dizziness and memory disorders are often combined (Windscheid's triad). The patients are incapacitated and have signs of severe disability (group I).
Diagnostics
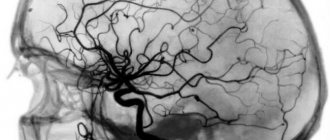
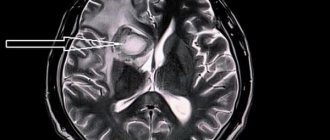
chronic cerebrovascular insufficiency is based on clinical data and additional studies of the vascular system and brain. In the fundus, vascular atherosclerosis and pallor of the optic disc are detected. The tortuous and compacted temporal arteries, compacted common, external and internal carotid arteries at the level of the neck are palpated. Rheoencephalography with functional tests (with nitroglycerin, hyperventilation for 3 minutes, turning and tilting the head, etc.), Doppler ultrasound with its variants (extracranial, transcranial, duplex scanning, ultrasound angiography, etc.), magnetic resonance imaging of the brain is performed. and the vessels supplying it (extra- and intracranial), carotid, vertebral or panangiography, X-ray examination of the aorta and large vessels. Useful information can be obtained from a biomicroscopic examination of the vessels of the conjunctiva, a biochemical study of lipid metabolism, as well as from an electroencephalogram and electrocardiogram. Often atherosclerosis of cerebral vessels is combined with atherosclerosis of the coronary arteries and vessels of the lower extremities.
Differential diagnosis
carried out in order to exclude brain pathologies of other origins and diseases of internal organs in which the function of the nervous system is secondarily affected (diabetes mellitus, damage to the liver, kidneys, lungs, gastrointestinal tract, etc.).
Treatment and prevention
When the first signs of chronic cerebrovascular insufficiency appear, periodic courses of treatment should begin to prevent progression of the disease. At the same time, primary prevention of atherosclerosis and vascular diseases of the nervous system should be organized by general practitioners (local therapists, family doctors, in large enterprises - workshop therapists), who explain the rules of a healthy lifestyle, including diet, self-regulation of work, rest and sleep patterns , adequacy of physical activity, skills and methods of relieving psycho-emotional stress, etc. Drug therapy for initial manifestations of insufficiency of cerebral blood supply is prescribed together with a therapist, taking into account the entire somatic status. Prescribed courses of vasoactive drugs (Cavinton, vinpocetine, cinnarizine, etc.), antisclerotic agents that improve blood rheology, and antiplatelet agents (acetylsalicylic acid and its derivatives, Wessel Due F, chimes, etc.), nootropic and neuroprotective drugs, including those containing amino acid complexes (actovegin, cortexin, glycine, etc.), antihypoxants, tranquilizers, vitamins B, E, etc.
Patients often have a fairly pronounced pathology of the cardiovascular system (hypertension, atherosclerosis), with coronary insufficiency, diabetes mellitus, obesity, I tereotoxicosis, etc., which requires the selection of additional combinations of drugs. In this regard, the doctor must remember and explain to patients: it is better to carry out the planned treatment with one drug for the full course of taking it, then after a short break (7-10 days) start taking another drug - and so on consistently for an unlimited time. If on the same day there is a need to take other drugs to correct the impaired function of internal organs, then taking the drugs should be separated by at least 30 minutes. It is strictly inadvisable to swallow 2 or more medications at the same time, since their interaction in the stomach is unpredictable, and this often leads to a decrease in the therapeutic effectiveness of each of the drugs taken and allergic reactions to medications.
If signs of cerebrovascular insufficiency appear, you should refrain from overheating (in the sun, in a sauna), climbing mountains more than 1000 m above sea level, consuming tobacco, alcohol (more than 30 ml of alcohol), strong tea and coffee (more than 2 portions per day), physical overload, prolonged exposure to TV, personal computer (no more than 45 minutes).
Measures to prevent cerebrovascular insufficiency should be carried out from adolescence (primary prevention) and be aimed at correcting risk factors: obesity (overeating, large meals in the evening), physical inactivity, smoking, abuse of alcohol and other drugs, stress, etc., and also to prevent exacerbations of the disease, repeated acute cerebrovascular accidents (secondary prevention).
Products to improve blood circulation in the brain:
– amino acids of animal and plant origin (meat, legumes);
– seafood (mussels, shrimp) and sea fish (mackerel);
– vegetables and fruits high in vitamin C and group B;
– cereals, nuts, berries and citrus fruits (rich in bioflavonoids).
Drinking regime
– a separate item in the program for improving blood circulation in the brain. Research shows that sufficient water consumption (2.5 liters per day in the absence of additional instructions due to pathologies) is the prevention of blood clots. However, in case of pathologies, it is still necessary to use antiplatelet agents or anticoagulants prescribed by a doctor.
Thirst quenching is also necessary for the development of neural populations28,29. The latest research shows that molecular hydrogen in drinking water protects the brain from neurodegenerative changes of various origins, including those caused by traumatic brain injury30. Therefore, to improve blood supply to the brain, it is necessary to drink enough water, and the drinking regime should be regular - the recommended 2.5 liters must be evenly distributed throughout the entire waking period.
Please note that 2.5 liters is an average. According to research, women on average need to drink less water than men (2.2 liters and 3 liters per day, respectively)31. Also, the recommended daily amount of water is determined by weight, age and lifestyle32. Below is a table of recommended daily water intake.
V.V. Zakharov Department of Nervous Diseases MMA named after. THEM. Sechenov, Moscow
One of the most common pathological conditions in neurological practice is brain damage of vascular etiology, which includes stroke and chronic insufficiency of blood supply to the brain. According to the World Federation of Neurological Societies, at least 15 million strokes are registered annually in the world. It is also assumed that a significant number of acute cerebrovascular accidents remain unaccounted for. Stroke is in third place among the causes of mortality and in first place among the causes of disability, which emphasizes the high relevance of this problem both for medical workers and for society as a whole [10]. The existence of chronic cerebral ischemia has long been disputed in foreign literature. Leading world angioneurologists, such as V. Khachinsky and others, in 1970-1980. postulated that there cannot be structural damage to the brain without stroke [15]. However, the development of modern neuroimaging methods has shown that long-term uncontrolled arterial hypertension can lead to diffuse changes in the deep parts of the white matter of the brain (the so-called leukoaraiosis), which is currently considered as a neuroimaging correlate of chronic cerebral ischemia [7, 20]. Stroke and chronic cerebral ischemia are caused by common causes, the most common of which are cerebral artery atherosclerosis and arterial hypertension. Due to the etiological commonality, both pathological processes are usually present simultaneously: patients with chronic insufficiency of blood supply to the brain have anamnestic or neuroimaging signs of strokes, and patients with stroke have signs of chronic cerebral ischemia. Assessing the contribution of each pathogenetic mechanism separately to the formation of clinical symptoms seems very difficult, and from a practical point of view, impractical. Therefore, at present, discirculatory encephalopathy (DE) is generally understood as a clinical syndrome of brain damage of vascular etiology, which can be based on both repeated strokes and chronic insufficiency of blood supply to the brain or a combination of both [3, 5]. Some other terms are also proposed to denote this clinical condition, such as chronic cerebral ischemia, cerebrovascular disease, ischemic cerebral disease, etc. However, from our point of view, the term “dyscirculatory” encephalopathy is the most appropriate, since it reflects the localization of the lesion, its nature and at the same time is not strictly connected with a specific pathogenetic mechanism: only with acute or only with chronic cerebral ischemia.
Clinical manifestations of discirculatory encephalopathy Clinical manifestations of DE can be very diverse. As mentioned above, most patients with chronic vascular diseases of the brain have a history of strokes, often more than once. The localization of strokes undoubtedly largely determines the characteristics of the clinic. However, in most cases of cerebrovascular pathology, along with the consequences of strokes, there are also neurological, emotional and cognitive symptoms of dysfunction of the frontal lobes of the brain. This symptomatology develops as a result of disruption of connections between the frontal cortex and the subcortical basal ganglia (the “disconnection” phenomenon). The cause of “disconnection” is diffuse changes in the white matter of the brain, which, as mentioned above, are a consequence of arterial hypertension [3, 17]. Depending on the severity of the disorders, it is customary to distinguish three stages of DE. At stage I, symptoms are predominantly subjective. Patients complain of headache, unsystematic dizziness, tinnitus or heaviness in the head, sleep disturbance, increased fatigue during physical and mental stress, forgetfulness, and difficulty concentrating. Obviously, the above symptoms are nonspecific. It is assumed that they are based on a slight or moderate decrease in mood. Emotional disorders in chronic insufficiency of blood supply to the brain are of an organic nature and are the result of secondary dysfunction of the frontal lobes of the brain due to disruption of frontostriatal connections [3]. Along with emotional disorders, at stage I of DE, impairments of cognitive functions can also be detected, most often in the form of slowness of higher nervous activity, a decrease in the volume of RAM, and inertia of intellectual processes. These neuropsychological symptoms reflect involvement of the deep parts of the brain with secondary dysfunction of the frontal lobes. As a rule, at stage I DE, cognitive impairment does not form a clinically defined syndrome and is therefore classified as mild [3, 8, 9]. In the neurological status, there may be an increase in tendon reflexes, often asymmetrical, uncertainty when performing coordination tests, and slight changes in gait. Like emotional and cognitive disorders, changes in the neurological status at this stage of DE are nonspecific, therefore, instrumental research methods confirming the vascular nature of brain damage are of fundamental importance for diagnosing cerebrovascular insufficiency at stage I DE [3, 5]. Stage II of discirculatory encephalopathy is spoken of in cases where neurological or mental disorders form a clinically defined syndrome. For example, we may be talking about mild cognitive impairment syndrome. Such a diagnosis is legitimate in cases where impairments in memory and other cognitive functions clearly go beyond the age norm, but do not reach the severity of dementia [8, 19, 21]. At the same time, in the structure of cognitive disorders, neuropsychological symptoms of frontal-subcortical dysfunction usually retain their dominant position. At stage II of DE, pseudobulbar syndrome, extrapyramidal disorders in the form of hypokinesia, mild or moderate increase in muscle tone of the plastic type, ataxic syndrome and other objective neurological disorders can also develop. On the other hand, subjective neurological disorders characteristic of stage I DE usually become less pronounced or less relevant for patients [3, 5]. At stage III of dyscirculatory encephalopathy, there is a combination of several neurological syndromes and, as a rule, vascular dementia is present - impairments of memory and other cognitive functions of vascular etiology, which lead to maladjustment of the patient in everyday life. Vascular dementia is one of the most severe complications of cerebrovascular insufficiency. According to statistics, vascular dementia is the second most common cause of dementia in old age after Alzheimer's disease and is responsible for at least 10-15% of dementias. As a rule, vascular dementia is accompanied by severe gait disturbances, in the pathogenesis of which dysfunction of the frontal regions of the brain also plays a role. Pseudobulbar syndrome, pelvic disorders, etc. are also very characteristic [4]. Vascular dementia, like DE in general, is a pathogenetically heterogeneous condition. Vascular dementia can occur as a result of a single stroke in a strategic area of the brain for cognitive activity or as a result of repeated strokes in combination with chronic cerebral ischemia. In addition, in addition to cerebral ischemia and hypoxia, secondary neurodegenerative changes play an important role in the pathogenesis of dementia in cerebrovascular insufficiency, at least in some patients with DE. Modern research convincingly shows that insufficient blood supply to the brain is a significant risk factor for the development of degenerative diseases of the central nervous system, in particular Alzheimer's disease (AD). The addition of secondary neurodegenerative changes undoubtedly aggravates and modifies cognitive disorders in cerebrovascular insufficiency. At the same time, memory impairments become more pronounced, which initially extend to current events, and as the disease progresses, to more distant life events. In such cases, the diagnosis of mixed (vascular-degenerative) dementia is legitimate [4].
Diagnosis of DE To diagnose dyscirculatory encephalopathy syndrome, a thorough study of the disease history, assessment of the neurological status, and the use of neuropsychological and instrumental research methods are necessary. It is important to emphasize that the presence of cardiovascular diseases in an elderly person does not in itself prove the vascular nature of the detected neurological disorders. Evidence is needed of a cause-and-effect relationship between the symptoms observed in the clinical picture and vascular damage to the brain, which is reflected in the diagnostic criteria of DE accepted today: (according to Yakhno N.N., Damulin I.V., 2001): • presence of signs (clinical , anamnestic, instrumental) brain damage; • presence of signs of acute or chronic cerebral dyscirculation (clinical, anamnestic, instrumental); • the presence of a cause-and-effect relationship between hemodynamic disorders and the development of clinical, neuropsychological, and psychiatric symptoms; • clinical and paraclinical signs of progression of cerebrovascular insufficiency. Arguments in favor of such a connection may be the presence of focal neurological symptoms, a history of stroke, characteristic changes in neuroimaging, such as post-ischemic cysts or pronounced changes in white matter, the specific nature of cognitive impairment in the form of a predominance of symptoms of frontal-subcortical dysfunction over memory impairment.
Treatment of DE Cerebrovascular insufficiency is a complication of various cardiovascular diseases, therefore etiotropic and pathogenetic therapy of DE should be primarily aimed at the underlying pathological processes of chronic cerebral vascular insufficiency, such as arterial hypertension, atherosclerosis of the main arteries of the head, heart disease and etc. Adequate antihypertensive therapy is one of the most important measures in the management of patients with cerebrovascular insufficiency. Arterial hypertension is one of the most powerful and independent risk factors for acute cerebrovascular accidents. Long-term uncontrolled arterial hypertension leads to secondary changes in the vascular wall of small-caliber arteries (arteriolosclerosis), which underlies chronic ischemia of the deep parts of the brain. In addition, it has now been proven that arterial hypertension is also a risk factor for the neurodegenerative process, which often complicates the course of vascular dementia. Therefore, adequate antihypertensive therapy is an essential factor in the secondary prevention of the increase in mental and motor symptoms of DE. One should strive for complete normalization of blood pressure (target figures are no more than 140/80 mm Hg), which, according to international studies, significantly reduces the risk of both acute cerebrovascular accidents and vascular and primary degenerative dementia. However, normalization of blood pressure should be done slowly, over several months. A rapid decrease in blood pressure can lead to worsening cerebral perfusion due to improper reactivity of arterioles altered by lipohyalinosis [13, 16, 23]. The presence of atherosclerotic stenosis of the main arteries of the head requires the prescription of antiplatelet agents in cases where the stenosis exceeds 70% of the vessel lumen or the integrity of the vascular wall is compromised. Drugs with proven antiplatelet activity include acetylsalicylic acid in doses of 50-100 mg per day and clopidogrel (Plavix) in a dose of 75 mg per day. Studies have shown that the use of these drugs reduces the risk of ischemic events (myocardial infarction, ischemic stroke, peripheral thrombosis) by 20-25%. However, it should be kept in mind that there are individual differences in response to antiplatelet agents. In some cases, the effectiveness of these drugs is insufficient, and in some patients a paradoxical proaggregant effect is observed. Therefore, after prescribing acetylsalicylic acid or clopidogrel, a laboratory study of the aggregation of blood cells is necessary [2]. In order to enhance the antiplatelet effect of acetylsalicylic acid, it may be advisable to simultaneously administer dipyridamole at a dose of 25 mg three times a day. Monotherapy with this drug did not show any preventive effect against cerebral or other ischemia, however, when used in combination, dipyridamole significantly increases the preventive effect of acetylsalicylic acid [2]. In addition to prescribing antiplatelet agents, the presence of atherosclerotic stenosis of the main arteries of the head requires consultation of the patient with vascular surgeons to decide on the advisability of surgical intervention. Currently, the positive preventive effect of surgery in patients with a history of transient ischemic attacks or small strokes has been proven. The benefits of surgery for asymptomatic stenosis are less convincing [2]. If there is a high risk of cerebral thromboembolism, for example with atrial fibrillation and valvular disease, antiplatelet agents may be ineffective. The listed conditions are an indication for the prescription of indirect anticoagulants; the drug of choice is warfarin. Therapy with indirect anticoagulants should be carried out under strict monitoring of coagulation parameters, and the international normalized ratio (INR) should be examined every two weeks [2]. The presence of hyperlipidemia that cannot be corrected by diet requires the prescription of lipid-lowering drugs. The most promising in this case are statins (Zocor, Simvor, Simgal, Rovacor, Medostatin, Mevacor, etc.). Currently, the prescription of these drugs is considered justified not only for hyperlipidemia, but also for normal cholesterol levels in patients with coronary heart disease or diabetes mellitus. The advisability of prescribing these drugs to prevent the development of cognitive impairment and dementia is also discussed, which, however, requires further research [6, 11, 18]. An important pathogenetic event is also the impact on other known risk factors for cerebral ischemia, which include smoking, diabetes mellitus, obesity, physical inactivity, etc. [4, 11, 18]. In the presence of cerebrovascular insufficiency, it is pathogenetically justified to prescribe drugs that act primarily on the microvasculature, such as: • phosphodiesterase inhibitors: aminophylline, pentoxifylline, vinpocetine, tanakan, etc. The vasodilating effect of these drugs is associated with an increase in the content of cAMP in the smooth muscle cells of the vascular wall, which leads to to their relaxation and increase in the lumen of blood vessels [5, 6]; • calcium channel blockers: cinnarizine, flunarizine, nimodipine. They have a vasodilating effect due to a decrease in the intracellular calcium content in the smooth muscle cells of the vascular wall. Clinical experience suggests that calcium channel blockers, such as cinnarizine and flunarizine, may be more effective for circulatory failure in the vertebrobasilar system [1, 5, 6]; • a2-adrenergic receptor blockers: nicergoline. This drug eliminates the vasoconstrictor effect of the mediators of the sympathetic nervous system: adrenaline and norepinephrine [5, 6]. In neurological practice, vasoactive drugs are most often prescribed. In addition to their vasodilatory effects, many of them also have positive metabolic effects, which allows them to also be used as symptomatic nootropic therapy. In domestic neurological practice, vasoactive drugs are usually prescribed in courses of two to three months, once or twice a year [5, 6]. Metabolic therapy is widely used for cerebrovascular insufficiency, the purpose of which is to increase the compensatory capabilities of the brain associated with the phenomenon of neuronal plasticity. Neuronal plasticity is understood as the ability of neurons to change their functional properties during life, namely to increase the number of dendrites, form new synapses, and change membrane potential. It is likely that neuronal plasticity underlies the process of restoration of lost functions that is observed after a mild stroke or other brain damage. Metabolic drugs include pyrrodoline derivatives (piracetam, pramiracetam, phenotropil), which have a stimulating effect on metabolic processes in neurons. The experiment found that the use of piracetam increases intracellular protein synthesis and utilization of glucose and oxygen. With the use of this drug, there is also an increase in blood supply to the brain, which is likely secondary to an increase in metabolic processes. In clinical practice, the positive effect of piracetam has been shown in patients with mild cognitive impairment of an age-related nature, in the recovery period of ischemic stroke, especially in cortical lesions with clinical aphasia, as well as in mental retardation in childhood [5, 6]. Another strategy for influencing cerebral metabolism is the use of peptidergic and amino acid drugs. These include Cerebrolysin, Actovegin, glycine and some others. They contain biologically active compounds that have multimodal beneficial effects on neurons. Clinical and experimental studies of peptidergic drugs indicate an increase in the survival of neurons in various pathological conditions, improvement of cognitive functions, and regression of other neurological disorders [5, 6]. Like vasoactive drugs, metabolic therapy is traditionally given in courses once or twice a year. Pathogenetically justified and appropriate is the combined implementation of vasoactive and metabolic therapy. Currently, the doctor has several combined dosage forms at his disposal, which include active substances with vasoactive and metabolic effects. These drugs include instenon, vinpotropil, Phezam and some others. Phezam is a combined vascular-metabolic drug that contains 25 mg of cinnarizine and 400 mg of piracetam. As mentioned above, cinnarizine is a calcium channel blocker, which has the greatest effect on microcirculation in the vertebrobasilar region. Therefore, the use of Phezam has the most beneficial effect on symptoms of vertebrobasilar insufficiency, such as vestibular disorders, dizziness and unsteadiness when walking. It should be noted that in addition to vasoactive properties, cinnarizine also has a symptomatic effect against systemic dizziness, so Phezam can be used not only for cerebrovascular insufficiency, but also for symptomatic purposes in peripheral vestibulopathy. Piracetam, which is part of the drug, effectively promotes the normalization of cognitive functions and memory, the reduction of residual effects of a neurological defect, psychopathological and depressive symptoms, the elimination of disorders of autonomic regulation, asthenia, insomnia, and the improvement of general well-being and performance. Fezam is prescribed one or two capsules three times a day for two to three months. Contraindications to the use of Phezam are severe impairment of liver and/or kidney function, parkinsonism, pregnancy and lactation, and children under five years of age. The development of vascular dementia syndrome requires more intensive nootropic therapy. Of the modern nootropic drugs, acetylcholinesterase inhibitors and memantine have the most powerful clinical effect on cognitive functions. These drugs were initially used to treat mild to moderate dementia due to Alzheimer's disease. However, today their clinical effectiveness has also been proven in vascular and mixed dementia [11, 12, 14, 18, 22]. In conclusion, it should be emphasized that a comprehensive assessment of the state of the cardiovascular system of patients with cerebrovascular insufficiency, the impact on both the cause of the disorders and the main symptoms of DE, undoubtedly helps improve the quality of life of patients and prevent severe complications of cerebrovascular insufficiency, such as vascular dementia and movement disorders.
Literature 1. Andreev N.A., Moiseev V.S. Calcium antagonists in clinical medicine. M.: RC "Pharmedinfo", 1995. 161 p. 2. Warlow C.P., Dennis M.S., J. van Geyn et al. Stroke. Practical guide for the management of patients / trans. from English St. Petersburg, 1998. P. 629. 3. Damulin I.V. Dyscirculatory encephalopathy in the elderly and senile age / Abstract of thesis... Dr. med. M., 1997. 32 p. 4. Damulin I.V. Alzheimer's disease and vascular dementia / ed. N.N. Yakhno. M., 2002. P. 85. 5. Damulin I.V., Parfenov V.A., Skoromets A.A., Yakhno N.N. Circulatory disorders in the brain and spinal cord // Diseases of the nervous system. Guide for doctors / ed. N.N. Yakhno, D.R. Shtulman. M., 2003. pp. 231-302. 6. Zakharov V.V., Yakhno N.N. Memory impairment. M.: GeotarMed, 2003. P. 150. 7. Martynov A.I., Shmyrev V.I., Ostroumova O.D. et al. Features of damage to the white matter of the brain in elderly patients with arterial hypertension // Clinical Medicine. 2000. No. 6. P. 11-15. 8. Yakhno N.N., Zakharov V.V., Lokshina A.B. Syndrome of moderate cognitive impairment in dyscirculatory encephalopathy // Journal of Neurology and Psychiatry named after. S.S. Korsakov. 2005. T. 105. No. 2. P. 13-17. 9. Yakhno N.N., Lokshina A.B., Zakharov V.V. Mild and moderate cognitive impairment in dyscirculatory encephalopathy // Clinical gerontology. 2005. T. 11. No. 9. P. 38-39. 10. Bogousslavsky J. The global stroke initiative, setting the context with the International Stroke Society // J Neurol Sciences. 2005. V. 238. Supp l.1. IS. 166. 11. Erkinjuntti T., Roman G., Gauthier S. et al. Emerging therapies for vascular dementia and vascular cognitive impairment // Stroke. 2004. Vol. 35. P. 1010-1017. 12. Erkinjuntti T., Roman G., Gauthier S. Treatment of vascular dementia-evidence from clinical trials with cholinesterase inhibitors // J Neurol Sci. 2004. Vol. 226. P. 63-66. 13. Forrete F., Seux M., Staessen J. et al. Prevention of dementia in randomized double blind placebo controlled Systolic hypertension in Europe (Syst-Eur trial) // Lancet. 1998. V. 352. P. 1347-1351. 14. Kumor V., M. Calach. Treatment of Alzheimer's disease with cholinergic drugs // Int J Clin Pharm Ther Toxicol. 1991. V. 29. No. 1. P. 23-37. 15. Hachinski VC, Lassen NA, Marshall Y. Multi-infarct dementia: a cause of mental deterioration in the elderly // Lancet. 1974. V. 2. P. 207. 16. Hansson L., Lithell H., Scoog I. et al. Study on cognition and prognosis in the elderly (SCOPE) // Blood Pressure. 1999. V. 8. P. 177-183. 17. Hershey LA, Olszewski WA Ischemic vascular dementia // Handbook of Demented Illnesses. Ed. by JCMorris. New York etc.: Marcel Dekker, Inc. 1994. P. 335-351. 18. Lovenstone S., Gauthier S. Management of dementia. London: Martin Dunitz, 2001. 19. Golomb J., Kluger A., Garrard P., Ferris S. Clinician's manual on mild cognitive impairment // London: Science Press, 2001. 20. Pantoni L., Garcia J. Pathogenesis of leukoaraiosis // Stroke. 1997. V. 28. P. 652-659. 21. Petersen RS Current concepts in mild cognitive impairment // Arch. Neurol. 2001. Vol. 58. P. 1985-1992. 22. Sahin K., Stoeffler A., Fortuna P. Et al. Dementia severity and the magnitude of cognitive benefit by memantine treatment. A subgroup analysis of two placebo-controlled clinical trials in vascular dementia // Neurobiol.Aging. 2000. Vol. 21.P. S27. 23. Tzourio C., Andersen C., Chapman N. et al. Effects of blood pressure lowering with perindopril and indapamide therapy on dementia and cognitive decline in patients with cerebrovascular disease // Arch Inern Med. 2003. V. 163. N. 9. P. 1069-1075.
Improving blood circulation in the brain - physical activity and exercise
Physical inactivity (lack of physical activity) can be caused by many factors - from sedentary work to basic laziness. It has a number of negative consequences, including problems with the cardiovascular and respiratory systems, bones33,34.
In the context of cerebral circulation, lack of physical activity is associated with an increased risk of blood clots35 and deterioration of the conductive capacity of gray matter (a major component of the central nervous system)36. Therefore, anyone who leads a sedentary lifestyle is recommended to take regular walks, run every night, practice Nordic walking, or workout in the gym.
Research shows that regular physical exercise has a beneficial effect on blood flow throughout the body, including the brain37,38. There are special sets of exercises to improve blood circulation in the brain, and there are also specialized programs implemented in the presence of certain pathologies.
A set of exercises to improve blood circulation in the brain:
– Take a sitting position, looking straight ahead, turn your head 45 degrees to one side, then to the other.
– Slowly rotate your head in a circle, first to the right, then to the left.
– Tilt your head up so that your chin points to the ceiling. Then lower your head to your chest and touch your chin to your chest.
– Bend to the right and left towards your shoulders so that your ear touches your shoulder. The shoulders are motionless.
– Looking straight ahead, stretch your head forward as much as possible, return it to its original position and pull it back as far as possible.
The entire complex is performed as slowly and carefully as possible. The purpose of exercises to improve blood circulation in the brain is to relax the muscles that compress the blood vessels and normalize blood flow. Each movement is performed 10-15 times; for sedentary work, it is recommended to perform the complex 2-3 times during the day at approximately equal intervals.
Exercises to improve blood circulation in the brain with cervical osteochondrosis include neck rotations, lateral flexions, rotation, retractions, and stretching of the trapezius muscle. The figure below shows an example of such a complex.
There are many specialized complexes of medical gymnastics to improve blood circulation in the brain in case of osteochondrosis of various joints39,40. It is unacceptable to perform these exercises on your own; they are performed only under the supervision of a specialist, or as directed and after consulting a doctor.
Treatment and prevention of cerebrovascular accidents
Stroke is one of the leading causes of death and the most common cause of disability.
Stroke prevention includes:
- Timely diagnosis and treatment of diabetes.
- Treatment of arterial hypertension: sodium restriction, regular use of medications to lower blood pressure.
- Controlling blood cholesterol levels: proper nutrition, weight loss, use of statins.
- Diagnosis and identification of the causes of transient ischemic attacks (TIA).
- Avoiding stress and psycho-emotional overload.
- Timely diagnosis and treatment of vascular atherosclerosis.
- Maintaining a sleep schedule and physical activity.
- Diet selection.
- Strengthening the walls of blood vessels, both with medications and preventive measures - hardening, gymnastics, taking antioxidants and vitamins.
- Quitting smoking.
Adequate treatment of cerebral circulatory disorders begins with examination and establishment of the exact cause of the pathology. You cannot self-medicate and haphazardly reduce blood pressure - this disrupts the coordinated work of the cardiovascular system, increases the load on the walls of blood vessels, which leads to the formation of aneurysms, stenoses and, as a result, impaired renal filtration, thereby aggravating the course of hypertension, increasing the risk of strokes and heart attacks . When antihypertensive drugs are taken irregularly and incorrectly, cerebral perfusion pressure drops, which causes blockage of blood vessels and brain hypoxia. The presence of the slightest symptoms of MV disturbance is a reason to immediately consult a doctor.
Unfortunately, against the background of constant stress, poor nutrition, untimely examination, uncontrolled use of medications, cerebrovascular accidents began to affect young people. Sometimes, frequent headaches may indicate the onset of changes in the blood vessels of the brain, and therefore taking painkillers can complicate timely diagnosis and lead to complications.
The initial examination of the cerebral blood supply should include:
- Clinical blood test
- General urine analysis
- Biochemical blood test, in particular lipid profile with determination of the atherogenic index, determination of blood glucose
- Coagulogram
- Ultrasound of brachycephalic and transcranial vessels of the neck and brain
- Ultrasound of the heart (ECHO-CG)
- Ultrasound of the kidneys and adrenal glands
- Measuring anthropometric data and calculating body mass index
- Consultation with an ophthalmologist, with mandatory examination of the fundus vessels
- Consultation with a cardiologist
- Neurologist consultation
This is a mandatory list for a basic study to determine the risks or degree of cerebrovascular accident, but the doctor, based on the examination data, anamnesis and research results, can recommend more in-depth examinations, including CT and MRI, to establish the severity of the condition, establish the correct diagnosis and select therapeutic and preventive measures.
For more detailed consultation, examination and examinations, please contact medical specialists.
Improving blood circulation in the brain - bioactive supplements
Most dietary supplements for improving brain circulation are nootropics, the mechanism of action of which is related to stimulating blood flow. One of the popular nootropics with this mechanism of action is glycine. This is an aliphatic amino acid that functions as a neurotransmitter and has an “inhibitory” effect on neurons, which gives a mild sedative effect.
Glycine reduces the release of GABA and glutamic acid and stimulates blood circulation in the brain. Target effects – relieves irritability and aggressiveness, eliminates chronic fatigue syndrome, improves brain function, stimulating cognitive functions (memory, reaction, attention).
Among nootropics there are not only amino acids, but also extracts, for example, ginkgo biloba extract. It contains 24% flavonoids, vitamins, minerals and other bioactive substances. It has a vasodilating effect, improves blood flow to the brain and blood flow inside the organ. It also stabilizes blood pressure and cholesterol levels, improves microcirculation. Helps eliminate neurocirculatory dystonia and chronic fatigue syndrome caused by psycho-emotional stress.
Complex supplements, such as “Healthy Sleep,” will help improve blood circulation in the brain, eliminate anxiety and normalize sleep. This supplement includes glycine, gamma-aminobutyric acid, tryptophan, melatonin and 4 extracts - lemon balm, passionflower, valerian and chamomile. The benefit of the supplement is that it not only stimulates blood circulation in the brain and improves cognitive function, but also stabilizes the sleep/wake cycle, helping to get enough sleep.
Cerebrovascular diseases: retribution for carelessness or an inevitable reality?
Russia - half a million strokes per year
Cerebrovascular diseases (CVDs) are the most important medical and social problem of modern neurology, as they give the highest rates of morbidity, mortality and disability.
CVD is divided into acute (stroke and transient cerebrovascular accidents - transient ischemic attacks), as well as chronic forms (chronic cerebral ischemia - “dyscirculatory encephalopathy”, vascular dementia). This division is conditional, since stroke, as a rule, develops against the background of chronic cerebral ischemia, being a certain stage of cerebrovascular disease.
Within the framework of the ICD X, the classification of CVD is carried out in connection with the predominant lesion of the vascular system of the brain, which is reflected in the corresponding headings: I 65—“Occlusion and stenosis of the precerebral arteries, not leading to cerebral infarction”, I 66—“Occlusion and stenosis of the cerebral arteries, not leading to cerebral infarction"; and also depending on the leading clinical syndrome in headings I 67—“Other cerebrovascular diseases”: I 67.2—cerebral atherosclerosis, I 67.3—progressive vascular leukoencephalopathy, Binswanger’s disease; I 67.4—hypertensive encephalopathy, “other specified cerebral vascular lesions: acute cerebrovascular insufficiency, chronic cerebral ischemia” (I 67.8).
Vascular dementia is also distinguished - heading F 01 (F 01.0 - vascular dementia with acute onset, F - 01.1 multi-infarct dementia, F 01.2 - subcortical vascular dementia, F 01.3 - mixed cortical and subcortical dementia), as well as a number of neurological syndromes considered as consequences of previous cerebrovascular diseases (section I 69). In ICD-10, the term “dyscirculatory encephalopathy” is absent. However, in our country it is the most commonly used.
The etiology of CVD is extremely complex and involves complex interactions between numerous factors. According to WHO, there are over 300 risk factors associated with stroke, which are grouped into four categories:
- main modifiable risk factors (high blood pressure, atherosclerosis, smoking, physical inactivity, obesity, unhealthy diet, diabetes);
- other modifiable factors (social status, mental disorders, emotional stress, alcohol abuse, certain medications);
- non-modifiable risk factors (age, heredity, nationality, gender);
- “new” risk factors (hyperhomocysteinemia, inflammation, abnormal blood clotting).
“Axis of evil” of cerebrovascular pathology
The main “axis of evil” in the pathophysiology of CVD is endothelial dysfunction and changes in the rheological properties of blood, which underlie the increase in its coagulation activity.
However, despite the presence of universal patterns, the process of cerebral ischemia is individual. The features of its course are determined by the compensatory capabilities of cerebral blood flow, the background state of brain metabolism and the reactivity of the neuroimmunoendocrine system.
On average, about 400-500 thousand strokes (80-85% ischemic) are registered annually in Russia, of which up to 200 thousand are fatal, and of the surviving patients, at least 80% remain disabled. There is also a tendency towards an increase in the incidence of stroke in young people.
Therefore, modern neurology is dominated by the doctrine of the dynamic nature and potential reversibility of cerebral ischemia and the need for urgent measures to restore cerebral blood flow. Moreover, the stages of the pathophysiological cascade of the acute period of acute ischemic disturbance of cerebral hemodynamics have been revealed and it has been shown that the leading links of the pathological cascade are glutamate “excitotoxicity” with the activation of intracellular enzymes and the accumulation of intracellular Ca2+, increased synthesis of nitric oxide and the formation of oxidative stress, the development of a local inflammatory reaction, damage to the blood-brain barrier and microcirculatory disorders.
Genetic factors (latent and lifelong risk factors) are among the main non-modifiable risk factors and are receiving increasing attention in clinical trials of vascular diseases.
However, association studies between specific genotypes and diseases are often difficult to replicate. The extreme complexity of the physiological mechanisms mediating the influence of molecular genes on human physiology suggests that genotype-phenotype association studies will have one of the lowest signal-to-noise ratios of any type of epidemiological case-control study. In fact, the influence of many genetic factors appears only under certain environmental influences (smoking, taking certain medications, alcohol). For example, the presence of the Leiden variant increases the risk of thrombotic events by 2.6 times. When patients with this nucleotide variant of the F5 gene (or other genetic defects affecting blood clotting) also take oral contraceptives, the risk of sinus thrombosis increases almost 30 times, thus making sinus thrombosis almost inevitable. All external factors, such as diet and lifestyle, can theoretically be properly adjusted to minimize the risk of vascular disease. Genetic factors thus provide a unique opportunity for long-term prevention of cerebrovascular diseases in accordance with the individual genetic characteristics of patients.
Taking into account the above, the following pathogenetic forms of chronic CVD are distinguished:
- Atherosclerotic - characterized by damage to large main and intracranial vessels by the type of stenosis with the development and preservation of collateral circulatory pathways.
- Hypertensive - the pathological process develops in smaller branches of the vascular system of the brain (subcortical arteriosclerotic encephalopathy, Binswanger encephalopathy - the development of lacunar zones of ischemia and severe neuropsychological disorders with epileptic syndrome). In this variant, multi-infarct encephalopathy often develops - multiple, predominantly lacunar, small infarcts that occur against the background of arterial hypertension, with minor cardiogenic embolisms, angiopathy and coagulopathies.
Three stages of cerebrovascular insufficiency
The initial manifestations of CVD are cerebrovascular disease (weakness, increased fatigue, decreased mental performance), mild cognitive impairment. As the disease progresses, movement disorders, a sharp decrease in memory, and transient cerebral vascular crises occur. In the future, the development of vascular dementia, impaired control over the function of the pelvic organs, extrapyramidal syndrome and other various neurological complications is possible.
The most common type of chronic cerebral failure is its vertebrobasilar form, the causes of which can be not only atherosclerotic stenosis of the vertebral arteries, but also their deformation, congenital hypoplasia, compression caused by pathology of the cervical spine, etc.
This clinical form of CVD is characterized by: frequent attacks of dizziness, accompanied by nausea and sometimes vomiting; unsteadiness of gait; occipital headaches; hearing loss, tinnitus; memory loss; attacks of “blurred” vision, the appearance of “fly spots” in the field of vision; attacks of sudden falling, usually without loss of consciousness.
Pseudobulbar syndrome is characterized by disorders such as dysarthria, dysphagia, dysphonia (the voice becomes quiet, monotonous), drooling, decreased control over the functions of the pelvic organs and cognitive disorders.
Emotional and affective disorders (psychopathological syndrome) are observed at all stages of CVD. The early stages are characterized by neurosis-like, asthenic and asthenodepressive disorders, then they are joined by dysmnestic and intellectual disorders. Moreover, depression is observed in 25% of patients with vascular dementia.
In the domestic literature, there are three stages of chronic cerebrovascular insufficiency:
- Stage I is characterized by asthenoneurotic disorders, anisoreflexia, discoordination phenomena, mild oculomotor disorders, and symptoms of oral automatism.
- Stage II is characterized by a deepening of memory and attention impairments, an increase in intellectual and emotional disorders, a significant decrease in performance, mild subcortical disorders and gait disturbances, more distinct focal symptoms in the form of revitalized reflexes of oral automatism.
- At stage III, clearly defined discoordination, amyostatic, psychoorganic, pseudobulbar or pyramidal syndromes arise, and paroxysmal disorders are observed. At this stage of the disease, patients are sometimes completely capable.
Vascular dementia is a difficult diagnosis
The diagnosis of CVD is based on identifying, using clinical and instrumental methods, a cause-and-effect relationship between impaired cerebral blood supply and brain damage. It is important to note that the line between acute and chronic forms of cerebrovascular accident is very arbitrary. The cause of discirculatory encephalopathy and vascular dementia can be ischemic strokes caused by stenosis of large cerebral vessels and cardiogenic embolisms. Vascular dementia in this case occurs either due to several foci, often in both hemispheres of the brain, or due to a single ischemic focus.
The presence of an elderly patient with neuropsychological changes in a history of stroke is a compelling argument for diagnosing vascular dementia. Relative signs confirming the diagnosis of CVD can be considered: vascular risk factors, especially arterial hypertension, a history of transient ischemic attacks, the appearance of pelvic disorders or difficulty walking in the early stages of the disease, local changes in the electroencephalogram.
The compensatory mechanisms of the brain are so powerful that at any given time they can provide adequate needs of the nervous system and maintain clinical well-being. But when these mechanisms become depleted due to either a sudden decrease in the lumen of the vessel or damage to the vascular wall, a stroke occurs.
With computed tomography or magnetic resonance imaging, multiple ischemic foci are visualized in such patients. The location and size of the infarction and the total number of foci are important. At the same time, it is worth remembering that the differential diagnosis between degenerative forms of age-related dementia and CVD is not always simple, especially since almost 20% of cases of elderly dementia are mixed dementia.
Even at the morphological level there is no complete clarity. In Alzheimer's disease, in most cases, signs of previous strokes are found, and in cases of seemingly definite vascular dementia, histological signs of specific degenerative changes are found. At least half or more of all dementia cases have morphological features of both types of lesions.
The most characteristic sign confirming the vascular nature of dementia is the presence of multiple ischemic foci. In general, due to the vagueness of diagnostic criteria, the category of patients with “cerebrovascular pathology” is constantly expanding, incorporating patients with arterial hypertension, various chronic psychosomatic disorders, etc., since doctors purely subjectively and speculatively formulate a clinical diagnosis based on “cerebral” complaints.
On the other hand, the problem of so-called silent strokes, traces of which are detected by neuroimaging both in patients with a newly diagnosed acute clinical episode and in people without a history of stroke, has attracted much attention. Such instrumental findings confirm the idea of the cerebrovascular pathological process as a continuum: brain damage does not occur just like that, without an already established morphological background, in particular, changes in the vascular wall.
Restore hemodynamics and metabolism
Treatment of CVD should include interventions aimed at the underlying disease that initiated the damage to brain tissue, correction of the main syndromes, effects on cerebral hemodynamics and metabolism. Prevention of progression of CVD is carried out taking into account their heterogeneity.
In case of subcortical arteriosclerotic encephalopathy and multi-infarction condition against the background of arterial hypertension, the basis is normalization of blood pressure with correction of the perverted circadian rhythm of blood pressure. In case of a multi-infarction condition against the background of multiple cardioembolism, angio- and coagulopathies, the use of antiplatelet agents (acetylsalicylic acid at the rate of 1 mg per 1 kg of body weight per day, or clopidogrel, or dipyridamole 150-200 mg/day) and anticoagulants (for cardiac arrhythmias) is indicated warfarin is absolutely indicated).
Preventive treatment includes, as necessary, vasoactive drugs: pentoxifylline, vinpocetine, etc. Treatment of the main syndromes includes the use of nootropics, amino acid drugs and neurotransmitters (glycine, neuromidin, choline alfo-scerate), in case of impaired cognitive functions - ginkgo biloba preparations, anticholinesterase drugs. For dizziness and tinnitus, it is advisable to prescribe betahistine 16 mg 3 times a day.
Nootropics have an effective effect on cerebral hemodynamics and metabolism due to the implementation of multilateral (membrane stabilizing, antioxidant, neuroplastic, antihypoxic, neurotransmitter) neuroprotective effects. Particular attention has recently been paid to combination drugs that simultaneously improve cerebral perfusion and metabolism, such as the drug piracetam + cinnarizine. Moreover, primary neuroprotective therapy should begin within the “therapeutic window”, since its implementation during this period reduces the likelihood of severe strokes, extends the safe period for thrombolic therapy and in some cases has a protective effect against excessive reperfusion syndrome.
Since strokes are considered the most serious and obvious sign of progression of CVD, the main direction in the management of such patients is the organization of effective measures for primary and secondary prevention of acute cerebrovascular accidents (ACVA).
Primary prevention of stroke means preventing stroke in healthy individuals, patients with initial forms of CVD and in high-risk groups. Secondary prevention aims to prevent recurrent strokes.
Rehabilitation of patients and prevention of stroke are carried out according to a step-by-step program:
- stage 1 - establishment of a rehabilitation diagnosis, reflecting the clinical form, stage of the disease, the presence of concomitant pathology, psycho-emotional disorders;
- stage 2 - development of an individual rehabilitation program taking into account the biopsychosocial model of the disease (with the active participation of the patient) based on complex treatment;
- stage 3 - monitoring of effectiveness according to clinical neurological examination and neuropsychological testing, followed by correction of the complex of rehabilitation measures;
- stage 4 - final - assessing the effectiveness of the rehabilitation and drawing up a plan for further management of the patient.
“Three pillars” of secondary prevention of CVD
Today these are considered antiplatelet agents, antihypertensive drugs and statins. The use of antiplatelet agents (aspirin in a daily dose of 50-325 mg, clopidogrel, dipyridamole), according to a meta-analysis of the results of 287 clinical trials, demonstrated a reduction in the risk of serious vascular events (non-fatal myocardial infarction, non-fatal stroke and death from vascular causes) by 25% in patients previously suffered an ischemic stroke. However, antiplatelet agents, in the absence of constant monitoring, can cause complications, in particular, exacerbation of gastritis or peptic ulcer, the development of a vascular event while taking an antiplatelet or anticoagulant, and hemorrhage.
Drug lowering of blood pressure leads to a significant proportional reduction in the risk of stroke (indapamide - by 29%, perindopril [4 mg] together with indapamide [2-2.5 mg] - by 43%). After a stroke, blood pressure (regardless of its level) is recommended to be reduced with diuretics and/or angiotensin-converting enzyme inhibitors, taking into account individual tolerance to such therapy (evidence level I). Most clinical studies do not support the benefits of one therapy or another, with the exception of data on the advantage of losartan over atenolol and chlorthalidone over amlodipine.
Neurological disorders in CVD are grouped into five main syndromes: vestibular-atactic, pyramidal, amyostatic, pseudobulbar, psychopathological.
The third component of effective secondary stroke prevention is considered to be lowering blood cholesterol levels (the use of statins reduces the risk of a recurrent cerebral event by an average of 24%). In patients with a history of ischemic stroke, the appropriateness of prescribing a statin (simvastatin) should be considered first (level of evidence I). Probably, the pleiotropic effect of statins is important - their anti-inflammatory effects, which are realized in the area of atherosclerotic plaques, leading to the stabilization of the latter. During this period, statin use appears to be quite adequate even without cholesterol control. Prescribing 20 mg/day of atorvastatin, simvastatin or rosuvastatin provides a targeted preventive effect of these drugs with mandatory monitoring of liver function during therapy.
Antioxidants in the fight for a healthy brain
Since free radical oxidation acts as a nonspecific pathogenetic link in CVD, the feasibility and necessity of using antioxidants in the complex treatment of such patients is obvious. Among various medicines, the Russian antioxidant-antihypoxant Mexidol® (2-ethyl-6-methyl-3-hydroxypyridine succinate), which has neuroprotective properties, stands out. In accordance with the instructions for use, Mexidol® inhibits the processes of lipid peroxidation (LPO), increases membrane fluidity, increases the activity of antioxidant enzymes, activates the energy-synthesizing functions of mitochondria and improves energy metabolism in cells, modulates receptor complexes of brain membranes, enhancing their ability to bind. Mexidol® increases the body's resistance to damaging factors and has a cerebroprotective effect.
Our clinic has accumulated significant experience in using the drug Mexidol® in the complex treatment of patients with acute and chronic cerebral circulatory failure and other CVD.
In the vast majority of cases, we used a standardized drug administration regimen:
- daily intravenous drip administration of the drug Mexidol® in a dose of 5 ml of a 5% solution (250 mg) per 200 ml of physiological solution for 5-10 days;
- Subsequently, the drug was administered orally in tablet form at a dose of 125 mg three times a day for 30 days.
All patients received complex therapy, including dehydration, cardiovascular (as indicated) drugs, drugs that selectively improve cerebral circulation, neuroprotective drugs, and anticholinesterase drugs.
In the process of summarizing clinical experience on the use of antioxidants, the following tasks were solved:
- conducting a detailed analysis of the dynamics of the symptom complex of the disease in persons receiving Mexidol® in complex treatment (including based on the results of scoring on scales in relation to different nosologies);
- comparison of the results of therapy in patients receiving Mexidol® with the results in individuals in the control group, in whom Mexidol® was not used in complex treatment.
As a result of the treatment, which included Mexidol®, all patients with CVD showed an improvement in their condition in the form of almost complete regression of the general cerebral syndrome, as well as partial regression of focal symptoms (for example, a decrease in motor deficit by 1-2.5 points, cerebellar insufficiency and sensory disorders ). A comparison of two groups of patients, one of which used Mexidol®, indicates the high effectiveness of the drug in patients with CVD.
A characteristic sign of vascular dementia is the presence of multiple ischemic foci. Due to the vagueness of diagnostic criteria, the category of patients with “cerebrovascular pathology” is constantly expanding, incorporating patients with hypertension and psychosomatic disorders, as doctors speculatively formulate a clinical diagnosis based on “cerebral” complaints.
It should be noted that the use of Mexidol® in patients where CVD was accompanied by epilepsy led to an increase in the threshold of convulsive readiness of the brain according to EEG data, which determines not only the possibility of adequate neuroprotective therapy, but also the possibility of reducing the dose of antiepileptic drugs. Another significant criterion for the effectiveness of the use of the drug Mexidol® in patients with CVD is its pronounced anxiolytic effect, verified according to the Hamilton Anxiety Scale (anxiety reduction by an average of 4.5 points) one month from the start of therapy. While using Mexidol®, patients noted a significant improvement in general well-being, an increase in vitality, which correlated with an increase in activity, assessed using the Barthel index (an average of 18 points).
The use of the drug Mexidol® in patients with CVD in all studies has proven not only its effectiveness, but also its safety. There were no significant side effects recorded, and in no case was it necessary to either discontinue the drug or reduce the course dose, which significantly distinguishes Mexidol® from other drugs, since the problem of their safety is currently very relevant and is often considered one one of the main factors in choosing treatment strategies and tactics.
Thus, the drug Mexidol® belongs to the group of highly effective drugs with a multimodal spectrum of action and undoubtedly deserves the attention of not only neurologists, but also doctors of other specialties (therapists, psychiatrists, neurosurgeons, resuscitators). By increasing the body's resistance to the effects of various stress factors (ischemia, inflammation, shock, intoxication), Mexidol® is effective for the prevention, first of all, of decompensation of cerebral blood flow in individuals at risk for cerebrovascular pathology. However, this drug should be prescribed in adequate dosages (and it is advisable to use it intravenously at the beginning of therapy, and then in tablet form) and for a certain time (at least 5 weeks), which will allow achieving a higher therapeutic effect when using it.
Sometimes an impossible task
Thus, the variety of etiological factors causing the development of CVD makes the task of differential diagnosis of their pathogenetic forms extremely complex and sometimes impossible. In this regard, the strategy and tactics for treating patients with this pathology fall into the field of entropy and are unlikely to become ideal in the coming years. Taking this into account, therapy for victims becomes long-term and multidisciplinary. This should be understood and accepted by both doctors of various specialties and patients, because the treatment of cardiovascular diseases (atherosclerosis, coronary heart disease, hypertension, thrombosis, congenital heart defects and rheumatic heart disease) should not take place in isolation, without taking into account concomitant CVD. Recently, priority has been given to outpatient preventive and rehabilitation measures for patients with CVD. First of all, this is due to the significantly lower cost and availability of treatment in outpatient settings compared to inpatient ones. But can the measure of the correctness of patient management be a “coin”, when the price of manipulation is human life?
Improving blood circulation in the brain - vitamins
Among the vitamins for improving blood circulation in the brain, one can highlight Vitamin B5 (pantothenic acid), which is necessary for the functioning of nerve fibers, the division of epithelial cells and the formation of the inner wall of blood vessels. Vitamin B6 (pyridoxine) is involved in the functioning of the nervous system, is necessary for the formation of a number of neurotransmitters, and reduces the level of lipids in the blood. Vitamin B8 (inositol) is part of the protective membrane of brain cells, stabilizes lipid metabolism, and normalizes mood.
Vitamin C (ascorbic acid) normalizes blood clotting, stabilizing blood flow, stabilizes capillary permeability, and is an antioxidant. Also, complexes with minerals - phosphorus, magnesium, selenium and zinc - are useful to improve blood circulation in the brain. All these minerals are necessary to maintain the functioning of brain cells. Examples of such complexes are Magnesium + Vitamin B6, Zinc + Vitamin B6, Multivitamin complex 360.
Diagnostics
The diagnosis of chronic cerebrovascular accident is made based on a combination of examination data, symptoms, neurological signs, results of brain neuroimaging (MRI, or MSCT), and angiography of cerebral vessels.
The doctor may detect the presence of certain neurological, motor, and sensory deficits, such as changes in vision or visual fields, abnormal reflexes, abnormal eye movements, muscle weakness, decreased sensation, and other changes. In addition, certain tests help determine the presence of intellectual-mnestic disorders.
Laboratory research methods are prescribed for the diagnosis of somatic diseases.
Wait. Add the book to the cart.
The problem of damage to the venous system of the brain is a real “Cinderella” of modern angioneurology. The attention of researchers and practitioners is primarily drawn to the pathology of the arterial bed of the brain. Meanwhile, the venous system is important for the blood supply to the brain.
Prevention and treatment of venous encephalopathy is, first of all, the prevention and treatment of diseases that can complicate the characteristics of manifestations and the course of the pathological process. If the cause of venous circulation disorders in the brain is established, then treatment is aimed at eliminating it. For example, in case of heart failure, cardiac drugs are the main ones; when veins are compressed by a tumor, scar after injury or inflammation, which impede the outflow of blood from the cranial cavity, the issue of surgical intervention is decided.
Glivenol reduces congestion in the veins - the average daily dose is 0.6–1.2 g; aescusan - 250 mg tablets or oral solution, active ingredient - zecin; Troxevosin, Detrolex - 500 mg tablets; diosmin - 450 mg; hesperidin - 50 mg; Take 2 tablets per day, day and evening with meals. Improves blood supply to the brain, lowers venous pressure and cerebrospinal fluid pressure, reduces cerebral edema euphilin orally 0.1-0.2 g 2-3 times a day, intravenously 5-10 ml of a 2.4% solution in 10-20 ml 40 % glucose, intramuscularly 1–2 ml of 2.4% solution. Diuretics have a decongestant effect: diacarb, furosimide, mannitol (200–400 ml of a 15% solution intravenously in a stream, slowly or drip, used only in a hospital). Magnesia sulfate is also used (25% solution is administered intramuscularly or intravenously, 5–20 ml). Orally or parenterally B1, B6, B12, PP, etc. According to indications, tranquilizers, hypnotics and anticonvulsants are prescribed.
For severe signs of venous stasis and cerebral edema, as well as for cardiovascular failure with severe shortness of breath and cyanosis, bloodletting (300–400 ml) is recommended, including with the help of leeches (hirudotherapy). Maintaining hygiene is of great importance.
The choice of forms of work and physical activity depends on the underlying disease. Professions that require heavy physical stress, which may increase venous stagnation (loader, digger, etc.), as well as those associated with prolonged bending of the head or incorrect posture, are contraindicated. Do not work at heights, underground, or in high, low, or extreme temperatures.
If you have venous pathology of the brain, you should also not perform sports exercises, for example, on rings and others associated with great physical stress.
An increase in venous pressure in the cranial cavity can be promoted by prolonged reading, writing, drawing, performing minor instrumental work, as well as frequent strain associated with holding the breath. You need to take short breaks while working, during which, with your hands behind your head, take a few deep breaths. When writing, you should use an inclined desk-lectern to avoid slouching or bending your head.
It is preferable to live in a temperate climate, since patients do not tolerate temperature fluctuations well. Venous pressure may increase at high altitudes.
The patient should stay in the fresh air as long as possible, work and rest in a well-ventilated area. You need to sleep with a high pillow under your head. Sleep should be long enough, but not excessive. Daytime rest or sleep for 1–2 hours is recommended. During the day you need to sit with your head thrown back several times (5-6 minutes each). You need to rest in a half-sitting position. At the same time, your well-being improves, headaches go away even with obvious signs of venous stagnation.
Impetuous movements and sudden bends are harmful. Patients should walk at a moderate pace, monitor their breathing, and short breaks from work should be used for warm-up and breathing exercises.
Clothing should be loose and not tight around the neck. A tight collar can cause headaches, which disappear if you release its pressure. Do not tighten the belt too tightly, which also increases venous and internal pressure.
If you are prone to constipation, you need to follow a diet: food with limited liquid (3–4 glasses per day), salt (up to 5 g per day), carbohydrates and fats is recommended; food rich in proteins, vitamins, fiber (brown bread, vegetables and fruits). To prevent constipation, it is recommended to take laxatives.
If there are venous circulation disorders in the brain, smoking is strictly not recommended. Everyone knows the expression “smoker's cough.” In this case, venous pressure increases and signs of bettolepsy may occur. Moderation in sexual activity should be observed. Pregnant women with signs of severe venous congestion in the brain, if it is impossible to eliminate its cause, are advised to terminate the pregnancy or deliver by caesarean section. Childbirth represents excessive stress for them with a life-threatening increase in venous and internal pressure. Venous pressure often increases with negative emotions. Therefore, patients need a calm, friendly environment both at home and at work.
For venous cerebral insufficiency, systematic light breathing exercises have a beneficial effect: intensive inhalation through the nose and slow exhalation through the mouth. It should be noted that a rise in venous pressure may occur during a conversation. Older speakers who engage in extreme exertion are at risk of experiencing severe headaches, dizziness, and other brain symptoms. To be convinced of the significant impact of speakers' overstrain on the vessels, it is enough to observe their neck: the play of tension and collapse of the jugular veins, caused by fluctuations in intrathoracic pressure, is noticeable. Interrupting speech with frequent breaths can eliminate the increase in venous pressure.
Venous pressure is significantly reduced under the influence of a course of physical therapy, head and neck massage using the stroking method. Systematic air baths after morning sleep are useful. The naked patient walks around the room at a temperature of 21–22 °C for 10–15 minutes, after which he wipes himself with warm water (38–39 °C). In summer, air baths are taken outdoors in the morning, in the warmth. Patients with venous pathology of the brain are prescribed galvanic collars, warm seats and foot baths. If the state of health allows, then foot baths are carried out with the addition of hot water. Narzan, carbon dioxide and hydrogen sulfide baths are shown.
One of the important methods of combating venous encephalopathy is oxygen therapy, which normalizes vascular tone, improves overall well-being, and reduces headaches.
Sanatorium-resort treatment is recommended mainly in the middle zone. Staying in southern resorts during the hot season is contraindicated.