© Author: A. Olesya Valerievna, candidate of medical sciences, practicing physician, teacher at a medical university, especially for SosudInfo.ru (about the authors)
The umbilical cord is a special organ through which the developing embryo, and subsequently the fetus, is connected with the mother’s body. Normally, the vessels of the umbilical cord are represented by two arteries and a vein , through which blood and the oxygen and nutrients contained in it are exchanged.
Until recently, it was possible to find out how the umbilical cord is built, how many vessels are in it and whether there are other anomalies only after the birth of the baby through visual examination and histological examination. With the introduction and widespread use of ultrasound techniques and Doppler measurements, it became possible to “look” inside the uterus even before birth, to trace the nature of blood flow and the anatomical features of this organ.
To assess the state of blood circulation in the mother-fetus system, determining the number of umbilical cord vessels and the characteristics of blood flow through them is of great importance. Normally, the doctor diagnoses the presence of three vessels, but in rare cases he may miss one, and then the expectant mother begins to worry seriously. Let's try to figure out why the lack of one of the arteries is dangerous, how it will affect the baby, and what a woman who has this anomaly should do.
Formation and structure of the umbilical cord
The umbilical cord is a cord that connects the fetal surface of the placenta to the abdominal wall of the fetus. Its main components are blood vessels. On the outside, the umbilical cord is covered with a single layer of epithelial cells, and the vessels are surrounded by a jelly-like substance (Wharton's jelly), which plays a protective role, enveloping them on all sides.
By the end of pregnancy, the thickness of the umbilical cord reaches one and a half to two centimeters, the length is 50-70 cm, which allows the fetus to move freely in the uterine cavity even before birth, and the expectant mother feels peculiar tremors and movements. An excessively long or short umbilical cord is a sign of pathology.
As mentioned above, the umbilical cord must have two arteries and one vein. It is generally accepted that venous blood with carbon dioxide moves through the veins, and arterial blood rich in oxygen and nutritional components moves through the arteries. With the umbilical cord, the situation is somewhat different: the vein carries oxygenated blood to the tissues of the fetus, and the arteries carry venous blood away from the unborn baby.
The umbilical arteries exist only during fetal development. Departing from the internal iliacs, they pass along the inner surface of the abdominal wall, on the sides of the bladder in the form of a triangle, heading to the umbilical ring, where they are included in the umbilical cord. After birth, these vessels become empty, and only thin folds of peritoneum on the back of the abdominal wall remind of them.
There is only one umbilical vein, although initially there are two of them (the left one is reduced). Nature provides that only one vessel is sufficient to ensure adequate blood flow, so neither the fetus nor the mother experiences “inconvenience” due to an azygos vein. The umbilical vein delivers about 80% of the blood to the developing baby's inferior vena cava, and the remaining 20% is used for blood flow to the liver.
Uteroplacental blood flow system
The amount of blood that flows through the vessels of the umbilical cord during pregnancy is enormous. By the end of gestation, the fetus receives about 240 ml of arterial blood per minute through the vein, the same volume goes through the arteries to the placenta. About 5-20 minutes after the birth of a child, blood flow through the vessels of the umbilical cord remains, and at this time it can be taken for research and other purposes (preparation of medicines, for example), however, already during the birth process, under the influence of the release of the hormone oxytocin, the vessels of the umbilical cord begin to empty, and the organ quickly atrophies as unnecessary.
Video: series of lectures on fetal circulation
Diagnosis of the umbilical cord condition
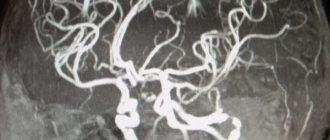
The most reliable information about the condition of the umbilical cord and its vessels can be obtained by ultrasound examination with color Doppler mapping. A transverse “section” of the umbilical cord shows the presence of a larger vessel – a vein, and a smaller diameter – an artery. The number of vessels is assessed from the longitudinal image. Data on the number of vessels can be obtained by the end of the first trimester, at about 12 weeks, when the woman is sent for the first screening test.
The accuracy of diagnosing the number of umbilical cord vessels can be influenced by various factors: the impossibility of good visualization of the organ too early or on the eve of birth, a small amount of amniotic fluid, more than one fetus in the uterus, excess weight in a pregnant woman. The qualifications of the doctor conducting the study also play a significant role.
Prenatal diagnosis of umbilical vein aneurysm: clinical observation with a favorable outcome
Ultrasound machine HM70A
Expert class at an affordable price.
Monocrystal sensors, full-screen display mode, elastography, 3D/4D in a laptop case. Flexible transformation into a stationary scanner with a cart.
Introduction
More than 40 years have passed since the first publication on ultrasound imaging of the umbilical cord [1], when Canadian specialists FR Morin and F. Winsberg described its echoanatomy. The B-stable gray scale scanning of the 70s of the last century with very modest resolution capabilities has been replaced by modern equipment with fantastic resolution capabilities that make it possible to identify the finest fetal and extraembryonic structures, the umbilical cord in particular, starting from the first weeks of gestation [2]. The number of publications devoted to this topic is infinitely large. Both the normal anatomy of the umbilical cord and its various anomalies are described: anomalies in size, and spatial arrangement of blood vessels, and the arrangement of umbilical cord fragments around each other and the fetus, and the pathology of Wharton's jelly, and the absence of the umbilical cord, and vascular anomalies, and neoplasia, etc. [3]. The frequency of their occurrence varies - from the “habitual” entanglement around the fetal body for obstetricians to rare forms, tumors and vascular aneurysms in particular. The impact of these conditions is ambiguous - from the absence of negative consequences, when the completion of pregnancy can be normal, to a fatal outcome.
The chapter “Anomalies of the umbilical cord that complicate the course of labor and worsen perinatal outcomes,” included in the National Guidelines for Obstetrics [4], mentions a rare vascular anomaly - an umbilical cord vein aneurysm (vein ectasia). The first case of prenatal diagnosis of umbilical vein aneurysm was described by F. Vesce et al. [5]. The anomaly described by the authors was complicated by the secondary formation of a hematoma. In their opinion, it is also possible to develop fetal anemia, non-immune hydrops and sudden intrauterine death. Most specialists who have studied the course of pregnancy and childbirth with aneurysmal changes in the umbilical cord vessels consider this pathology as potentially lethal [9–16]. In addition, according to a number of experts, venous ectasia of the umbilical cord has a significant correlation with chromosomal abnormalities of the fetus, trisomy 18 in particular [13, 17–19]. Due to its rarity, the population frequency of its detection is not indicated in any of the available literature sources.
Positive perinatal outcomes in this group of patients are much rarer [5–8]. In order to replenish the bank of favorable perinatal outcomes for such pathology, including those of domestic specialists [21, 22], we present our own observation of intrauterine ultrasound diagnosis of umbilical vein aneurysm.
Clinical observation
First pregnant K., 26 years old. Somatic and reproductive anamnesis are not burdened. During this pregnancy, the patient underwent screening ultrasound examinations at 12, 20 and 32 weeks using medium and expert class equipment.
Screening echography in the first and second trimesters did not reveal any anomalies in the development of the fetus or parafetal organs. During fetometry at 32 weeks of gestation, a discrepancy in the size of the trunk (abdomen) and the long tubular bones of the fetus was noted, which made it possible to formulate a conclusion about the asymmetrical form of fetal growth retardation. Doppler measurements did not reveal any disturbances in the uteroplacental-fetal blood flow. The amount of amniotic fluid corresponded to the norm. There were no specific localization features of the placenta. When assessing the condition of the umbilical cord, the following was revealed: there was its marginal attachment to the placenta; a round, thick-walled, hypoechoic formation with a diameter of 18 mm was visualized at the root of the umbilical cord (Fig. 1, 2).
Rice. 1.
Aneurysms of the vessel (vein) of the umbilical cord (sagittal scanning).
Rice. 2.
Aneurysms of the umbilical cord vessel (vein) (transverse scanning).
In the Color Doppler mode, scanty blood flow was recorded in this formation (Fig. 3); in the Power Doppler mode, a more intense blood flow was observed (Fig. 4, 5). Spectral Doppler measurements in the studied formation revealed medium-velocity arterial blood flow (18.5 cm/s) with episodes of venous contamination (Fig. 6). The number of vessels in the umbilical cord is normal.
Rice. 3.
Aneurysm of the umbilical cord vessel (vein), color flow mode.
Rice. 4.
Aneurysm of the umbilical cord vessel (vein), power Doppler mode (sagittal scanning).
Rice. 5.
Aneurysm of the umbilical cord vessel (vein), power Doppler mode (parasagittal scanning).
Rice. 6.
Arterial-venous spectrum of blood flow in an umbilical vein aneurysm.
The ultrasound report was formulated as follows: pregnancy 32 weeks. Asymmetrical form of fetal growth restriction without disruption of uteroplacental-fetal blood flow. Aneurysm of the umbilical cord vessel. Marginal attachment of the umbilical cord.
Dynamic echography in combination with Doppler and cardiotocography up to 37 weeks did not reveal any deterioration in the functional state of the fetus. There were no changes in the umbilical cord vascular formation detected at 32 weeks.
At 37 weeks 2 days, taking into account data on the centralization of fetal hemodynamics (decrease in the cerebroplacental ratio to 1.0), the pregnancy was completed by cesarean section. A live premature boy was born weighing 2400 g, length 52 cm, with an Apgar score of 6/6 points. Subsequently, the child in satisfactory condition was transferred to the second stage of neonatal care. Karyo type was determined: 46 XY.
When examining the placenta, the structural features discovered in utero were identified: at the root of the umbilical cord, attached to the edge of the placenta, there was a rounded formation measuring 2 x 2 cm (Fig. 7), on the section represented by an ectatic vein, surrounded by edematous Wharton's jelly (Fig. 8). Subsequent pathological examination of the umbilical cord confirmed the presence of an umbilical vein aneurysm with the presence of arteriovenous fistulas. This fact, from our point of view, explains the paradoxical nature of the blood flow we recorded in the pathologically altered umbilical cord vein: blood flow with the arterial spectrum with episodes of “venous spectrum contamination”. A similar spectrum of blood flow velocity curves in arteriovenous umbilical cord aneurysm was described by domestic specialists from Dagestan [21].
According to data conducted by N.P. Veropotvelyan et al. [16] analyzed 11 cases of prenatal diagnosis of umbilical cord aneurysm published before 2014; in 10 cases, the onset of pathology occurred in the third trimester (late manifestation). In observations, intrauterine fetal death occurred as a result of acute circulatory disorders in the umbilical cord vein due to compression by an aneurysm, while trisomy 18 was detected in 4 fetuses.
Rice. 7.
Aneurysm of the umbilical vein. Macropreparation (the wall of the aneurysm is not opened).
Rice. 8.
Aneurysm of the umbilical vein. Macropreparation (the wall of the aneurysm is opened).
The favorable outcome of the presented observation is probably due to the positive combination of the child’s normal karyotype and the small (2 cm) size of the umbilical cord venous aneurysm.
Literature
- Morin FR, Winsberg F. The ultrasonic appearance of the umbilical cord // J Clin. Ultrasound. 1978; 6 (5): 324–326.
- Abukhamad A.Z., Shaui R. Ultrasound diagnosis of fetal development anomalies in the first trimester of pregnancy: Trans. from English E.V. Yudina. M.: Vidar-M Publishing House, 2021. 384 p.
- Gagaev Ch.G. Pathology of the umbilical cord / Ed. V.E. Radzinsky. M.: GEOTAR-Media, 2011.
- Obstetrics: National Guide / Ed. E.K. Ailamazyan, V.I. Kulakova, V.E. Radzinsky, G.M. Savelyeva. M.: GEOTAR-Media, 2013: 427–435.
- Vesce F., Guerrini P., Perri G. et al. Ultrasonographic diagnosis of ectasia of the umbilical vein // J Clin Ultrasound. 1987; 15 (5): 346–349.
- Mysorekar V., Dandekar C., Sundari N. Umbilical Artery Aneurysm: Report of a rare case Singapore // J Obstet Gynaecol. 2002; 33(1):51–53.
- Hill A.J., Strong T.H., Elliott J.R., Perlow J.N. Umbilical artery aneurysm // Obstet Gynecol. 2010; 116(Suppl. 2): 559–562.
- Olog A., Thomas JT, Petersen S. et al. Large umbilical artery aneurysm with a live healthy baby delivered at 31 weeks // Fetal Diagn Ther. 2011; 29 (4): 331–333.
- Sherer DM, Anyaegbunam A. Prenatal ultrasonographic morphologic assessment of the umbilical cord: a review. Part II // Obstet Gynecol Surv. 1997; 52(8):515–523.
- Sentilhes L., Vivet-Lef-bure A., Patrier S. et al. Umbilical artery aneurysm in a severe growth-restricted fetus with normal karyotype // Prenat Diagn. 2007; 27 (11): 1059–1061.
- Shen O., Reinus C., Baranov A., Rabinowitz RR Prenatal diagnosis of umbilical artery aneurysm: a potentially lethal anomaly // J Ultrasound Med. 2007; 26 (2): 251–253.
- Siddiqi TA, Bendon R., Schultz DM, Miodovnik M. Umbilical artery aneurysm: prenatal diagnosis and management // Obstet Gynecol. 1992; 80(3, Pt 2): 530–533.
- Weber MA, Sau A, Maxwell DJ et al. Third trimester intrauterine fetal death caused by arterial aneurysm of the umbilical cord // Pediatr Dev Pathol. 2007; 10 (4): 305–308.
- Shen O., Reinus C., Baranov A., Rabinowitz RR Prenatal diagnosis of umbilical artery aneurysm: a potentially lethal anomaly // J Ultrasound Med. 2007; 26 (2): 251–253.
- Vandevijver N., Hermans RH, Schrander-Stumpel CC et al. Aneurysm of the umbilical vein: case report and review of literature // Eur J Obstet Gynecol Reprod Biol. 2000; 89(1):85–87.
- Veropotvelyan N.P., Gazarova L.V., Nikitina K.L., Podkosha S.G., Usenko T.V. Prenatal ultrasound diagnosis of umbilical cord vessel aneurysm // Prenatal diagnostics. 2014; 13 (2): 130–135.
- Berg C., Geipel A., Germer U., et al. Prenatal diagnosis of umbilical cord aneurysm in a fetus with trisomy 18 // Ultrasound Obstet Gynecol. 2001; 17(1):79–81.
- Sepulveda W., Corral E., Kottmann C. et al. Umbilical artery aneurysm: prenatal identification in three fetuses with trisomy 18 // Ultrasound Obstet Gynecol. 2003; 21(3):292–296.
- Heredia F., Jeanty Ph. Umbilical artery aneurysm is an extremely rare vascular anomaly. Umbilical cord anomalies. www.thefetus.net/ 2002-09-18-10
- Panda D., Stiller R., Iruretagoyena L., Levi A. Prenatal diagnosis of an umbilical vein aneurysm: a case report // Conn Med. 2009; 73(8):465–467.
- Esetov M.A., Esetov A.M. Prenatal ultrasound diagnosis of arterial-venous aneurysm of the umbilical cord: personal observation and review of the literature // Prenatal diagnostics. 2015; 14 (2): 137–142.
- Shatokha Yu.V. Prenatal ultrasound diagnosis of umbilical cord artery aneurysm with a favorable outcome // Prenatal diagnostics. 2018; 17 (2): 146–151.
Ultrasound machine HM70A
Expert class at an affordable price.
Monocrystal sensors, full-screen display mode, elastography, 3D/4D in a laptop case. Flexible transformation into a stationary scanner with a cart.
Where is the norm and where is the pathology?
Around the 21st week of gestation, all pregnant women are sent for a Doppler study, which allows one to evaluate not only the anatomical features of the fetus, placenta, and umbilical cord, but also the characteristics of blood flow (speed, number of vessels, anomalies). Often doctors do not bother to explain the results of the analysis to the patient, even briefly, so expectant mothers scour the literature and the Internet in search of answers.
Normally, at any stage of pregnancy, the umbilical cord has 3 vessels. Having received such a conclusion, the woman can calm down - the blood flow is fine (of course, if no other anomalies are found). In some cases, the ultrasound diagnostic doctor does not detect one artery in the umbilical cord, then the conclusion will indicate that there are only two vessels - one vein and one artery.
If there is an insufficient number of umbilical cord vessels, specialists will have to figure out whether the anomaly is isolated or combined with other defects, which is often found in this type of pathology. Some women note that the number of vessels during ultrasound differs at different times, and this creates even more questions, misunderstanding and unnecessary anxiety for the expectant mother.
Note that the number of vessels should not change throughout pregnancy, so there are two conclusions: either one of the arteries stopped functioning for some reason, or an error was made in one of the studies, and it is necessary to “recount” the vessels again, preferably – from a competent and experienced doctor who will dispel all doubts.
The umbilical cord has 3 vessels, what is it, what is the threat of 2 vessels?
Home / Articles / Pregnancy and childbirth / Pregnancy
June 5, 2015 |
How many vessels should the umbilical cord have - a “conductor” connecting the fetus with the mother during pregnancy, a supplier of nutrients and oxygen. Dopplerometry of the umbilical cord vessels is among the studies required for women who are preparing for motherhood. The procedure is carried out at 21 weeks, with its help the number of arteries is determined. The study allows you to timely identify abnormalities in the development of the embryo and take the necessary measures.
If, in the results of Dopplerometry, the expectant mother discovers that the umbilical cord has 3 vessels - what does this mean? If 2 vessels are diagnosed in the umbilical cord, what threat does this pose to the embryo?
The structure of the umbilical cord is normal
To understand why the umbilical cord has 3 vessels and what this means, you need to understand its structure. This is the name given to a kind of “rope” that ensures the connection between the embryo and the mother’s body and the interaction of the circulatory systems. The formation of the connecting element is completely completed by approximately 12 weeks. The length of the formation is 40-70 cm, “used” before the birth of the child. Normally, it is adjacent to the middle part of the placenta; there are exceptions (for example, membrane attachment).
How many vessels should there be in the umbilical cord? The norm is 2 arteries and one vein – 3 vessels. The vein serves as a conductor through which oxygenated blood penetrates the baby’s circulatory system from the woman’s body. Nutrients also leak into the vein through the vein. Arteries are used to remove waste products. 3 vessels in the umbilical cord during pregnancy indicate no cause for concern.
The structure of the umbilical cord - pathology
The norm that the umbilical cord must meet is 3 vessels, what this means can be read above. However, sometimes there is a deviation from this rule - two vessels in the umbilical cord. Expectant mothers are forced to face the medical verdict “EAP”, which stands for “single artery” of the umbilical cord, in about 0.5% of cases. The risk increases when it comes to multiple pregnancies, reaching 5%. The threat increases if a woman suffers from diabetes.
2 vessels in the umbilical cord - what does this mean, if there is a reason for concern? One of the arteries may be absent immediately, or its functionality may be impaired while waiting for the baby. EAP does not belong to the category of diagnoses that are fatal to the fetus, but requires additional research.
2 vessels in the umbilical cord - danger
So, the umbilical cord has 2 vessels - what does this mean for the baby? In approximately 90% of cases, EAP pathology is an isolated abnormality and does not turn into a threat to the fetus and mother. Despite the increasing load placed on the vessel, its functioning is not impaired. A small baby is born in about 13% of cases.
The umbilical cord vessels (2 or 3) are not of significant importance at the stage of childbirth. The main thing is that the specialist and junior medical staff attending the birth are aware of the presence of pathology. Labor management tactics, selected specifically for such a case, guarantee that there is no danger for the woman in labor and the fetus.
2 vessels in the umbilical cord - what are the dangers of deviation from the recognized norm during the birth process? If it is carried out incorrectly, hypoxia of the embryo is possible (lack of oxygen, complete interruption of its supply). To avoid danger, the doctor may choose a caesarean section. It is also necessary to cut the umbilical cord as carefully as possible - there is a risk of disrupting blood flow.
The umbilical cord has 2 vessels - what does this mean according to doctors? In such situations, obstetricians-gynecologists necessarily insist on additional examination, which is prescribed to the pregnant woman.
2 vessels in the umbilical cord - examination
It’s great if there are 3 vessels in the umbilical cord. However, timely diagnosis of deviations from this norm allows one to avoid risk even with one artery. The gynecologist must prescribe an additional examination to the woman to make sure that there are no other genetic pathologies that develop against the background of the disorder.
The number of vessels in the umbilical cord, normality or pathology - these questions can be clarified already by the 20th week, when the pregnant woman can undergo Dopplerometry. Most often, the umbilical cord has 3 vessels at 20 weeks. If, as a result of the study, it is determined that the number of arteries is not normal, Doppler testing is indicated for the expectant mother until birth. The procedure will provide control of blood flow in the vessels and will allow recording deviations.
Knowing how many vessels there should be in the umbilical cord, when diagnosing a disorder, it is worth consulting with a geneticist. An examination carried out by this specialist will help to reject the assumption of chromosomal abnormalities. A pregnant woman is advised to test blood obtained from the umbilical cord (cardocentesis). An ultrasound of the embryo's heart is required to exclude heart pathology - up to 22-24 weeks. Prevention tools - ultrasound of organs (each), cardiotocography (CTG).
2 vessels in the umbilical cord - is it necessary to terminate the pregnancy?
How many vessels are in the umbilical cord is a question, the answer to which is absolutely unimportant for the future life of the child. The diagnosis of EAP only indicates the need for additional examinations. A threat arises only when other chromosomal abnormalities that can harm the fetus are attached to a single artery.
Did you like the article? Share with friends:
to this entry
- Nnn May 20, 2021 at 6:29
My youngest son had two vessels instead of three... She carried it normally, although she often went for ultrasounds to monitor the baby’s development. Everything went well, she also gave birth without complications. The weight was 3.900. He grew and developed well... But! When he began to grow up, it was as if he had developmental delays. He only spoke when he was 4 years old. Now he is 7. He has bad memory. They tried to go to different clubs, he can’t do it, he can’t remember anything... He can’t even do simple poems, addition and subtraction don’t work either... He’s absent-minded, he always has to be reminded of everything, he even forgets his briefcase, he also constantly stumbles and falls... Not I know if this is somehow connected with his intrauterine development, but he’s the only one I have….
Answer
Oksana Mar 21, 2021 at 18:47
I was observed by a doctor throughout my pregnancy and gave birth on my own, quickly and without complications. Weight and height are good. The child is very active, has a good memory, at the age of 6 he reads, writes, and counts; his son’s development is simply excellent. She is ahead of her peers, which I am very happy about, because I read that children with two vessels, on the contrary, lag behind... but there is one thing... vision fails -5, -7 and a whole bunch of diseases associated with the eyes. We get treatment and go for procedures, but in general everything is fine with health, I rarely get sick.
Answer
Madina Oct 29, 2021 at 18:14
My daughter also had 2 vessels, she gave birth on her own, the birth went well, her height was normal, but her nails were too short, and today she is three years old and her nails still don’t grow, but only along with her fingers, we don’t cut them, on her toes nails are not beautiful, deformed((((
Answer
Anna Jun 25, 2021 at 3:57
My daughter had two vessels in her umbilical cord. She is already 8 years old, an excellent student, good memory, 100% vision, generally excellent health, tall, does not lag behind in anything, but on the contrary, at school she took part in all the clubs you can, and she entered art school. The doctors told me that 2 vessels do not affect what kind of child will be born, this is a variant of the norm!
Answer
Elena Oct 25, 2021 at 8:16
The number of vessels only affects the nutrition of the fetus. Vision, memory, and mental abilities do not depend on the number of vessels and arteries. I have a 5-year-old son, a completely healthy and active child, although there were 2 vessels. And this happens much more often than 0.5%, I only have 2 friends and everything is fine.
Answer
Leave your comment: Cancel
Two vessels in the umbilical cord: should I worry?
The mysterious abbreviation EAP in the doctor’s report means the presence of a single artery, that is, 2 vessels were found in the umbilical cord. This pathology occurs in approximately 0.5-1% of cases of normal pregnancies, and with multiple pregnancies the figure reaches 5%. About a third of fetuses with such a change in the umbilical cord, combined with other structural anomalies, are more likely to have severe chromosomal pathology, so the woman needs extensive examination, including from a geneticist.
The causes of the pathology are still not clear, but studies show that a lack of umbilical cord vessels is more common among women with diabetes, as well as among dark-skinned women. There may also be influence of external unfavorable factors that contribute to all sorts of deviations in the formation of the fetus, placenta and umbilical cord.
What threatens the presence of two vessels in the umbilical cord is the most important question that worries a pregnant woman, because any mother wants to give birth to a healthy baby. In such a situation, it is important to exclude other developmental defects, which determine the further prognosis and tactics of pregnancy management.
If the deficiency of one of the umbilical cord arteries is the only anomaly that doctors see with multiple ultrasounds, and chromosomal abnormalities are not confirmed by additional studies (cordocentesis, amniocentesis), then there is no reason to worry. Up to 90% of pregnancies with EAP in isolated form end successfully in the birth of a healthy child.
Of course, until the end of gestation you need to regularly monitor blood circulation, but, as practice shows, even one vessel is quite enough, because it is able to take on double the load. Only every tenth woman with an anomaly of the umbilical cord vessels may give birth to a low birth weight baby, but this most likely will not affect its further development.
Women with isolated EAP are recommended to undergo additional Doppler and ultrasound examination of the fetus at 28 weeks to exclude possible developmental delay. If the baby’s blood flow and growth rate correspond to the average norm, then the pregnancy develops correctly, and intrauterine growth retardation is excluded.
As they say, everything would be fine, but an isolated defect with the presence of 1 vessel in the umbilical cord of the arterial type is registered in only 7% of women, the rest of the cases are due to combined pathology, therefore, a much more dangerous scenario is considered to be the one when EAP is detected on ultrasound other structural abnormalities in the fetus. Especially often, malformations of the heart, blood vessels and genitourinary system are observed.
It has also been established that the deficiency of the left umbilical artery is more often accompanied by other defects on the part of the embryo than the underdevelopment of the right artery, although the reasons for this phenomenon are precisely unknown.
Pathology associated with a single artery in the umbilical cord:
- Heart defects;
- Anomalies of the genitourinary system;
- Underdevelopment of the bones of the skeleton and skull;
- Trisomy 21 pairs of chromosomes (Down syndrome);
- Miscarriages and intrauterine fetal death.
Umbilical cord - norm and pathology
Arterial blood flows through the umbilical cord vein, carrying oxygen to the fetal organs. Venous blood flows through the umbilical arteries from the fetus to the placenta; this blood contains metabolic products of the fetus. The vessels of the umbilical cord are located in a special gelatinous substance, which fixes them and protects them from injury, and also carries out the exchange of substances between the fetal blood and amniotic fluid. The umbilical cord begins to form from 2–3 weeks of pregnancy and grows with the baby. By the time of birth, its length is 45–60 cm (the length of the umbilical cord on average corresponds to the height of the child), and its diameter is 1.5–2 cm.
The umbilical cord can attach to the placenta in different ways. In some cases, attachment occurs in the center of the placenta (central attachment), in others - on the side (lateral attachment). Sometimes the umbilical cord is attached to the membranes without reaching the placenta itself (mechanical attachment). In these cases, the umbilical cord vessels approach the placenta between the membranes. Such attachment of the placenta is a risk factor for the occurrence of fetal-placental insufficiency.
The umbilical cord may also have such features as true and false nodes. False nodes are local thickenings of the umbilical cord due to varicose veins of the umbilical cord or accumulation of Wharton's jelly. They do not affect the development of the fetus and the birth process. True umbilical cord knots form in early pregnancy, when the fetus is still small, allowing it to slip through the umbilical cord loop. True umbilical cord knots can affect the outcome of birth. When the umbilical cord is stretched, the knot tightens, stopping the flow and flow of blood through the vessels. In this case, acute fetal hypoxia occurs.
A pathology of umbilical cord development is also a condition in which only one umbilical cord artery is formed instead of two; in some fetuses with one umbilical cord artery, various developmental defects are observed. The reason for this formation of the umbilical cord can be factors that cause fetal malformations - so-called teratogenic factors (chemicals, certain medications, ionizing radiation, genetic diseases of the parents).
Some problems may also arise due to shortening of the umbilical cord. Shortening of the umbilical cord can be divided into absolute and relative. With absolute shortening of the umbilical cord, the length of the umbilical cord is less than 45 cm. During pregnancy, this condition does not affect the development of the baby in any way. During childbirth, both with relative and absolute shortness of the umbilical cord, due to its tension, the placenta can prematurely detach, which the umbilical cord pulls along with it, which creates a direct threat to the life of the fetus.
False shortening of the umbilical cord occurs when the umbilical cord is entwined around the neck and torso of the fetus. The reason for entanglement of the umbilical cord may be its excessively long length (more than 70 cm), as well as increased motor activity of the fetus, which may be associated with chronic intrauterine fetal hypoxia. The causes of chronic lack of oxygen are different - these are maternal diseases, fetal diseases, and pathology of the placenta. The umbilical cord can be entangled once, twice or even three times. During pregnancy, the condition usually does not affect the fetus, but problems may occur during childbirth. Tension or compression of the umbilical cord vessels leads to disruption of blood flow.
Conditions such as umbilical cord shortening (absolute and relative) and true umbilical cord knots during labor can lead to acute intrauterine fetal hypoxia. It is manifested by a change in the number of heartbeats. (The normal fetal heart rate is 120–160 beats per minute.) When acute intrauterine fetal hypoxia occurs, original feces (meconium) appears in the amniotic fluid, and the water turns green. The appearance of all these symptoms requires emergency treatment. First of all, it is necessary to eliminate the cause of hypoxia, which is achieved through early delivery. The method of delivery depends on the stage of labor and how far the presenting part of the fetus (head or pelvic end) has advanced along the birth canal. If acute hypoxia occurs during pregnancy or in the first stage of labor, the woman undergoes a cesarean section. In the second stage of labor, when the head or pelvic end is already close to the exit from the pelvis, various obstetric aids are used to speed up the completion of the second stage of labor.
Fortunately, this condition does not occur often. Therefore, umbilical cord entanglement and umbilical cord knots are not an absolute indication for a planned cesarean section (absolute shortness of the umbilical cord cannot be diagnosed before birth). These conditions are relative indications for surgery, i.e. Caesarean section is performed only in cases where, in addition to them, there are other relative indications for the operation (the woman’s age is over 30 years, mild forms of gestosis, etc.).
The only method to suggest umbilical cord pathology is ultrasound scanning. Ultrasound can detect umbilical cord abnormalities, such as abnormal vascular development (single umbilical cord artery), true and false umbilical cord nodes, and umbilical cord entanglement. But the length of the umbilical cord during pregnancy is almost impossible to determine.
Special mention should be made about the diagnosis of umbilical cord entanglement. Sometimes during examination only loops of the umbilical cord in the neck area are visible, but it is impossible to determine whether they wrap around the neck. In these cases, a Doppler study helps, during which you can study the movement of blood through the vessels, including the umbilical cord. In addition, during childbirth, the cardiotocography method is used, which allows you to monitor the number of heartbeats, or listen to the fetal heartbeat using a stethoscope.
Thus, during pregnancy, umbilical cord pathology can only be suspected. However, timely ultrasound examinations will help doctors make your birth safe.