Fatty degeneration
Diabetes
3618 10 September
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment.
In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor. Fatty degeneration: causes, symptoms, diagnosis and treatment methods.
Definition
Fatty degeneration, or lipodystrophy, is a group of rare disorders that are characterized by complete or partial loss of subcutaneous fat, as well as its abnormal distribution, in the absence of a previous fasting or catabolic state. These diseases are accompanied by various metabolic disorders: insulin resistance, specific diabetes mellitus (lipoatrophic diabetes), fatty hepatosis, steatohepatitis, lipid metabolism disorders, arterial hypertension.
Fatty degenerations are quite rare conditions; according to various sources, their incidence ranges from 1 to 60 cases per 1 million population.
Causes of fatty degeneration
Fatty degenerations are divided into congenital and acquired. Congenital lipodystrophies are always hereditary and associated with genetic mutations that lead to metabolic disorders in adipose tissue, resulting in its atrophy.
The mechanism of development of acquired generalized lipodystrophy is unknown; the disease is assumed to be related to genetic mutations and autoimmune processes.
Genetic mutations are also suspected in the occurrence of acquired partial lipodystrophies. Today, the most common type of lipodystrophy is a special variant of acquired partial dystrophy - lipodystrophy, which develops as a result of highly active antiretroviral therapy in HIV-infected patients. In addition, there are local lipodystrophies, which are usually associated with injections of drugs, for example, insulin.
Classification of the disease
Fatty degenerations are divided according to the degree of fat loss into generalized, when subcutaneous fatty tissue is absent over most of the body, and partial, or segmental, when adipose tissue atrophies in certain areas of the body.
Hereditary and acquired lipodystrophies are divided into 4 types:
- congenital generalized lipodystrophy (CHL, Berardinelli-Seyp syndrome) with 4 types depending on the gene in which the mutation occurred;
- acquired generalized lipodystrophies (PGL, Lawrence syndrome);
- familial partial lipodystrophy (FPL, Dunnigan-Cobberling syndrome) with 3 types;
- acquired partial lipodystrophy (PPL, Barraquer-Simons syndrome).
Separately, there are fatty degenerations that develop as a result of other genetic syndromes and those associated with drug injections.
Symptoms of fatty degeneration
With congenital generalized lipodystrophy, immediately after birth or in the first year of life, the child develops a complete absence of subcutaneous fat. Lipoatrophy can occur on the trunk, limbs, and face. In severe cases of the disease, there is a significant risk of intrauterine growth retardation. Due to the lack of fatty tissue, the patient experiences pseudohypertrophy of skeletal muscles, as a result of which the patient has an “athletic” appearance (usually observed in children over 10 years of age). Patients with generalized lipodystrophy are tall (ahead of bone age), they may have an enlarged lower jaw, hands and feet, there is an enlargement of the clitoris in women and external genitalia in men, children have a very high appetite - they are “insatiable.” Due to the difficulty in digesting fats, the level of lipids (triglycerides, cholesterol) in the blood increases and the load on the organs involved in their metabolism increases. There is an abnormal accumulation of fat in the liver, kidneys, myocardium, and skeletal muscles, which disrupts their functions.
This type of lipodystrophy is characterized by severe fatty hepatosis, leading to liver enlargement, steatohepatitis, liver cirrhosis and liver failure.
Since metabolism is a balanced system, when lipid metabolism is disturbed, both protein and carbohydrate metabolism suffer. Disorders of carbohydrate metabolism lead to insulin resistance from the first years of life and to the development of type 2 diabetes mellitus by the age of 15-20 years. Such patients experience hyperpigmentation of the groin area, neck, armpits, weight loss, increased thirst, and excessive urination. Some forms of congenital generalized lipodystrophy are accompanied by damage not only to adipocytes (adipose tissue cells), but also to skeletal muscle cells and myocardium (heart muscle), which can lead to hypertrophic cardiomyopathy, heart failure and subsequently to an unfavorable outcome.
In addition, with this type of lipodystrophy, psychomotor retardation, intellectual impairment, hirsutism (excessive hair growth in women according to the male pattern - in the armpits, on the pubis, above the upper lip) or hypertrichosis (excessive hair growth in all areas of the body and head, not associated with the secretion of sex hormones). Due to the lack of subcutaneous fat, the veins of the upper and lower extremities bulge - this is called phlebomegaly. The characteristic appearance of the patient is a thin face against the backdrop of a developed figure, noticeable saphenous veins, increased size of the feet and hands, areas of hyperpigmentation (acanthosis nigricans) in the area of skin folds.
With acquired generalized lipodystrophy, a child is born with a normal amount of subcutaneous fatty tissue, and its degradation begins in childhood or adolescence and occurs gradually. Large areas of the body are affected, especially the face and extremities, including the palms and soles. In approximately a quarter of cases, patients with PGL are first diagnosed with panniculitis (inflammation of subcutaneous fat tissue), which manifests itself as local lipodystrophies. There are also PGL associated with autoimmune diseases (~25%) and idiopathic (~50%).
Familial partial lipodystrophies appear in childhood or adolescence. A progressive loss of adipose tissue begins in the chest, anterior abdominal wall and limbs with its redistribution to other areas - the face, neck and inside the abdominal cavity. This redistribution of subcutaneous fat may resemble Cushing's syndrome or create a false impression of an “athletic” physique in women. In men, the redistribution of adipose tissue and the expression of skeletal muscles are often perceived as a normal physique. Metabolic disorders develop after puberty and are more severe in women.
SPF is characterized by insulin resistance, a significant increase in the concentration of free fatty acids and triglycerides in the blood, accumulation of fat in skeletal muscle cells and hepatocytes, and impaired leptin secretion.
Patients have a high risk of developing diabetes mellitus and insulin resistance, dyslipidemia, mainly due to increased triglyceride levels, pancreatitis, liver steatosis, hyperpigmentation in skin folds (this symptom is less pronounced than with VHL), arterial hypertension. In rare cases, myopathies and cardiomyopathies may develop, as well as hirsutism, menstrual irregularities and polycystic ovary syndrome, however, in most patients, reproductive function remains intact.
Acquired partial lipodystrophy is characterized by a progressive loss of subcutaneous fat in the upper body - in the face, neck, chest, upper extremities, and epigastric region.
This process can begin at any age, lasts from several months to several years and moves from top to bottom from the head to the feet, but, as a rule, does not affect the lower limbs. On the contrary, some patients may develop excess accumulation of fatty tissue in the lower abdomen, buttocks and thighs. Metabolic disorders are less common than in other types of fatty degeneration, but PPL is associated with the development of chronic kidney disease.
Diagnosis of fatty degeneration
When collecting complaints and anamnesis, the doctor pays attention to the patient’s appearance, and also studies the family history of the disease to identify the nature of its inheritance.
From laboratory examinations the patient is given:
- general blood analysis;
Myocardial dystrophy
Myocardial dystrophy is a non-inflammatory damage to the heart muscle caused by metabolic disorders in the body.
The causes of the disease can be the following factors:
- Avitaminosis;
- Violation of carbohydrate, protein, fat metabolism (with liver failure, uremia, diabetes, etc.);
- Endocrine system disorders (thyrotoxicosis, hypothyroidism, dysfunction of the pituitary gland);
- Disorders of electrolyte metabolism (when the content of potassium and calcium in the body is higher or lower than normal);
- Systemic neuromuscular disorders (myasthenia gravis, myopathy);
- Oxygen starvation (with pulmonary and heart failure);
- Intoxication (poisoning of the body with dangerous substances, including alcohol intoxication, drug overdose, as well as in the case of kidney and liver failure, etc.).
- Infections (acute and chronic);
- Neurogenic effects (stress, sympathicotomy).
- Anemia;
- Physical overexertion.
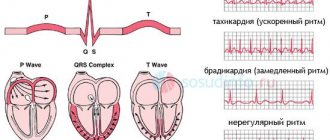
Myocardial dystrophy does not have clear symptoms, since it is a concomitant diagnosis, and the patient’s well-being is largely determined by the course of the underlying disease. The patient's complaints boil down to unpleasant sensations, dull pain in the heart area, shortness of breath, palpitations, and fatigue. With this disease, the ability of the heart muscle to contract is impaired, which causes mild and, much less frequently, moderate forms of heart failure. Cardiologists distinguish three stages of development of myocardial dystrophy:
- Neurofunctional (when there is no deviation from the norm yet, but metabolic tension already exists);
- Metabolic-structural or organic changes (there are already signs of changes in the myocardium);
- Stage of heart failure (pronounced changes in the structure and functions of the heart muscle).
It is believed that myocardial dystrophy is reversible. Treatment of this disease is aimed at influencing metabolic processes, conduction disorders, and heart failure.
Thus, medications that affect electrolyte metabolism are widely used. These are mainly potassium salts, magnesium and phosphorylated vitamins B and B6.
A popular remedy is anabolic hormones, which have shown their effectiveness in disorders of protein metabolism and nutrition of the heart muscle. This group of drugs includes methandrostenolone, pyridine (orotatkaly) and purine (riboxin, inosid) mononucleotides, ATP and AMP.
An important role in the treatment of myocardial dystrophy is played by systematic visits to sanatoriums specializing in the treatment of cardiovascular diseases. Mineral waters, rich in potassium, calcium and magnesium and other essential substances, will replenish the biochemical imbalance in the body and restore electrolyte metabolism.