Diabetic polyneuropathy
Diabetic polyneuropathy (DPN) is a combination of nervous system damage syndromes pathogenetically associated with diabetes mellitus.
The frequency among people with type 2 diabetes reaches 70-90%. DPN is classified depending on the predominant involvement of the spinal nerves (peripheral neuropathy) and/or the autonomic nervous system (autonomic neuropathy).
Diabetic distal symmetric sensorimotor polyneuropathy is the most common type of peripheral diabetic neuropathy. Typical symptoms are a burning sensation, “pins and needles”, pain in the legs and feet, and night muscle cramps. A neurological examination reveals weakened Achilles reflexes, sensory disturbances of the “socks” and “gloves” type, and decreased proprioceptive sensitivity. It is important that with late diagnosis of the pathology, complications of foot ulcers develop that can lead to gangrene (diabetic foot) and often to amputations. Tricyclic antidepressants (amitriptyline) are effective in treatment as painkillers, alpha-lipoic acid and B vitamins against the background of active glycemic control.
Autonomic neuropathy leads to dysregulation of vital functions and maintenance of homeostasis, which determines the course and structure of mortality in type 2 diabetes.
There is a gastrointestinal form of DPN, characterized by gustatory hypersalivation, hypo- and atony of the stomach, atony of the esophagus, intestinal hypomotility, functional hypoacidosis, reflux esophagitis, atony of the gallbladder and dyskinesia of the biliary tract with a tendency to cholelithiasis.
The urogenital form of DPN can be clinically manifested by atony of the ureters and bladder, reflux and stasis of urine, a tendency to develop urinary infection, and erectile dysfunction.
The main clinical manifestations of cardiovascular autonomic neuropathy include resting tachycardia (“fixed” pulse, often an early sign of developing DPN), arrhythmias (neuropathic prolongation of the QT interval, etc.), orthostatic hypotension, silent myocardial ischemia (SMI), arterial hypertension (increased activity of the sympathetic nervous system caused by parasympathetic dysfunction; lack of blood pressure reduction at night).
The most severe complication of cardiovascular autonomic neuropathy is sudden death.
Methods for diagnosing cardiovascular autonomic neuropathy include: examination of cardiovascular reflexes (Valsalva test, Shelong test, etc.), 24-hour blood pressure monitoring, Holter ECG monitoring, measurement of the corrected QT interval and Q interval dispersion.
Treatment of most forms of autonomic disorders is symptomatic. The main principle of reducing the progression of DPN is glycemic control.
Atrial flutter. Atrial fibrillation (atrial fibrillation)
Atrial flutter (AFL) is one of the most common cardiac arrhythmias, accounting for about 10% of all paroxysmal supraventricular tachyarrhythmias. It is a common complication of acute myocardial infarction and open heart surgery. Other causes of atrial flutter include chronic pulmonary disease, pericarditis, thyrotoxicosis, rheumatism (especially in individuals with mitral stenosis), sinus node dysfunction (Tachy-Brady syndrome), as well as other diseases that contribute to atrial dilatation. Atrial flutter can occur in patients of almost any age. However, it is much more common in those who have heart disease.
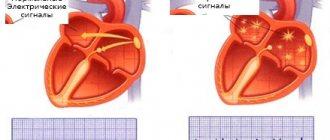
Atrial fibrillation (AF) is a supraventricular tachyarrhythmia characterized by uncoordinated electrical activation of the atria at a rate of 350-700 per minute, which causes deterioration of atrial contractility and the actual loss of the pre-filling phase of the ventricles.
Atrial fibrillation is one of the most common and frequently encountered arrhythmias in clinical practice.
Clinical manifestations
Typically, patients with atrial flutter complain of sudden palpitations, shortness of breath, general weakness, exercise intolerance, or chest pain. However, more severe clinical manifestations are possible - syncope, dizziness due to hypotension, and even cardiac arrest, due to a higher frequency of ventricular contraction. The pathophysiological basis of this symptomatology is a decrease in systemic output, systemic blood pressure and a decrease in coronary blood flow. According to some data, the decrease in coronary blood flow can reach 60% with increasing myocardial oxygen demand. Due to serious hemodynamic disorders, systolic dysfunction of the heart develops, followed by dilatation of its cavities, ultimately leading to heart failure.
Classification of atrial flutter
Atrial flutter is a fast, regular atrial tachyarrhythmia with atrial excitation and contraction rates greater than 200 per minute. It is now generally accepted that this arrhythmia is based on an excitation reentry mechanism.
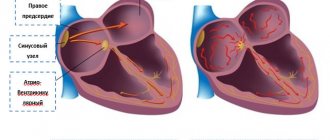
Typical AFL is caused by the right atrial circle of macroreentry, limited anteriorly by the ring of the tricuspid valve, and posteriorly by anatomical obstacles (openings of the superior and inferior vena cava, eustachian crest) and a functional barrier in the form of a terminal crista. In this case, the excitation wave passes through the lower isthmus (slow conduction zone), located between the inferior vena cava and the perimeter of the tricuspid valve. This is the so-called isthmus-dependent TP: it can be controlled by RF exposure in this zone.
Depending on the direction of the depolarization wave in the atria, two types of typical AFL are distinguished:
— AFL with activation of the interatrial septum (AS) in the caudocranial direction, and the lateral parts of the right atrium (RA) in the craniocaudal direction, i.e. with circulation of the excitation wave around the tricuspid valve counterclockwise (CCW) when viewed from the apex hearts. On the ECG it is characterized by negative F waves in leads II, III, aVF, reflecting synchronous activation of the MPP from bottom to top, and positive flutter waves in lead V1. The descending limb of F-waves in the lower standard and enhanced leads has a greater length (flatter) compared to the ascending (steeper) one. An important point is the noticeably smaller amplitude of atrial electrical activity complexes in lead V1, projected onto the ascending phase of the atrial wave in lead aVF;
— AFL with opposite activation of the structures of the right atrium, i.e. with circulation of the excitation wave clockwise (clockwise - CW), electrocardiographically characterized by the positive direction of flutter waves in the lower standard and enhanced leads and comparable in amplitude with F-waves in lead V1 .
However, patients may not always have characteristic ECG signs, so only during endoEPS can the involvement of the cavatricuspid isthmus be proven.
In addition to typical AFL, isthmus-dependent tachycardias include two-wave and lower loop atrial flutter. Two-wave AFL is characterized by the formation of two depolarization waves in the RA, circulating one after another around the tricuspid valve ring in the same direction, resulting in acceleration of the AFL. In this case, the geometry of atrial activation on the surface ECG does not undergo significant changes. This type of arrhythmia probably has little clinical significance, since it persists for a short period of time (up to 11 complexes), subsequently turning into typical atrial flutter, less often into atrial fibrillation.
Inferior loop TP is characterized by the breakthrough of an excitation wave through the terminal crista (TC) in its different parts with the formation of a re-entry circle around the mouth of the inferior vena cava with counterclockwise circulation of the impulse (CWW). In this case, the electrocardiographic characteristics of TP will depend on the level of conduction through the border sulcus. It will vary from an ECG pattern identical to a typical AFL/CWW, with a slight decrease in the amplitude of the positive phase of the flutter wave in the inferior leads and the P wave in lead V1, reflecting the collision of opposing depolarization fronts in the area of the RA fornix (with the breakthrough of the AFL wave in the caudal part TC) to an ECG pattern characteristic of a typical TP/CW, which will reflect the activation of the MPP in the craniocaudal direction (with a breakthrough in the region of the cranial part of the TC). These types of TP, just like typical forms of TP, are amenable to radiofrequency ablation in the area of the lower isthmus.
Isthmus-independent atrial flutter includes superior loop, multi-cycle and left atrial flutter. In case of superior loop AFL, the depolarization wave, breaking through the TC, forms a re-entry circle in the area of the RA arch along the perimeter of the superior vena cava with clockwise circulation of the impulse, while the lower parts of the RA are not involved in the RA cycle. The geometry of atrial activation on the surface ECG is similar to typical AFL/CW.
Multi-cycle AFL is characterized by the simultaneous presence of several cycles of atrial activation due to the possibility of multiple breakthroughs of excitation waves through the TC.
In more rare cases, macroreentry circles can form in the left atrium and are more likely to occur in patients who have undergone surgery on the left atrium. The electrocardiographic picture in these variants of TP will be very variable.
Treatment of atrial flutter
Emergency treatment
Emergency care for AFL depends on the clinical manifestations. In patients with acute vascular collapse, cerebral ischemia, angina pectoris, or with increasing manifestations of heart failure, emergency synchronized cardioversion is indicated. Successful restoration of sinus rhythm can be achieved with a discharge of less than 50 J when using single-phase currents, and with biphasic currents - even less energy. The use of drugs of classes Ia, Ic and III increases the chances of using electropulse therapy.
Frequent atrial pacing, either transesophageal or intraatrial, is the method of choice for restoring sinus rhythm. According to medical literature, its effectiveness averages 82% (from 55 to 100%). Ultrafrequent pacing is particularly appropriate in patients with AFL following cardiac surgery, as epicardial atrial leads are often left in place in these patients postoperatively. Atrial pacing (PAC) should be started at a frequency 10 pulses higher than the spontaneous electrical activity of the atria during AFL. It is recommended to increase the pacemaker frequency to verify effective entry into the tachycardia cycle in increments of 10 extrastimuli. A sharp change in the morphology of TP waves according to the surface ECG in standard inferior and enhanced leads indicates a switching (resetting) of TP. Stopping the pacemaker at this point may be accompanied by restoration of sinus rhythm. The critical frequency required to terminate type 1 TP usually exceeds the flutter frequency by 15-25%. The use of quinidine, disopyramide, procainamide, propafenone, ibutilide increases the chances of the effectiveness of ultra-frequent stimulation to restore sinus rhythm. Attempts to terminate AFL using ultrafrequent pacing can often lead to the induction of atrial fibrillation, which often precedes spontaneous restoration of sinus rhythm. Induction of atrial fibrillation is more likely when using a more “fast” mode of ultra-frequent stimulation (the cycle length during stimulation exceeds the TP cycle by 50% or more).
A number of drugs (ibutilide, flecainide) effectively restore sinus rhythm in AFL, but significantly increase the risk of developing fusiform ventricular tachycardia. Neither drugs that slow AV conduction nor cordarone have been effective in restoring sinus rhythm, although they can effectively control heart rate.
In most cases, with AV conduction 2:1 and higher, patients do not have hemodynamic disturbances. In such a situation, the clinician may opt for drugs that slow down AV conduction. Calcium antagonists (non-dihydroperidine series) and adrenergic blockers should be considered the drugs of choice. Adequate, although difficult to achieve, rate control is especially important if restoration of sinus rhythm is delayed (for example, if anticoagulant therapy is required). Moreover, if medical cardioversion is planned, then monitoring of tachysystole is necessary, since antiarrhythmic drugs, such as class Ic drugs, can reduce the atrial rate and cause a paradoxical increase in the ventricular rate due to slowing of latent AV conduction, which will worsen the clinical status of the patient.
If AFL lasts more than 48 hours, patients are advised to undergo anticoagulation therapy before electrical or drug cardioversion.
Continuous drug therapy
Chronic pharmacological preventive therapy for LT is usually imperial, its effectiveness is determined by trial and error. Traditionally, dual therapy has been recommended using both a drug that effectively blocks conduction at the atrioventricular junction and a membrane-active agent. The exception is class III drugs (sotalol, cordarone), which combine features of all classes of antiarrhythmic therapy.
Catheter ablation of the cavotricuspid isthmus for isthmus-dependent atrial flutter
It is now recognized that the creation of a complete bidirectional block in the isthmus between the inferior vena cava and the perimeter of the tricuspid valve using radiofrequency catheter ablation (RFA) is a highly effective and safe procedure for eliminating AFL and is gradually taking a leading place in the structure of various methods of treating these arrhythmias. Radiofrequency ablation can be performed either during AFL or during sinus rhythm. Previously, it was believed that the criterion for the effectiveness of the operation was the relief of TP. Subsequently, strict criteria were developed to achieve bidirectional conduction block in the area of the lower isthmus, which significantly increased the long-term effectiveness of RFA.
At the X-ray surgical center of the State Military Clinical Hospital named after. acad. N. N. Burdenko since 1999 to 2004 More than a hundred interventions have been performed for typical atrial flutter. Verification of conduction block in the area of the lower isthmus was carried out on the basis of local criteria for achieving conduction block in the area of interest and on the basis of traditional techniques for verifying conduction block (indirect method). The effectiveness of the procedure without maintenance AAT according to the results of prospective observation was 88%. Combined management of patients included: implantation of a system for permanent pacemaker, repeated interventions in the pulmonary veins, and resumption of AAT. Under these conditions, effective control of sinus rhythm during the calendar year was achievable in 96% of all clinical observations. We have proven a significant improvement in the pumping function of the atria, which ultimately can explain the significant positive clinical dynamics. The quality of life was significantly higher in patients after RFA.
Another prospective randomized study compared the effectiveness of continuous oral AAT (61 patients with AFL) and radiofrequency ablation. During a follow-up period of 21±11 months, sinus rhythm was maintained in only 36% of patients receiving AAT, whereas after RFA it was maintained in 80% of patients. In addition, 63% of patients receiving chronic drug therapy required one or more hospitalizations, compared with 22% of patients receiving RFA.
The absolute indication for RFA of LT are cases when resistance to or intolerance to multiple AAT develops or when the patient does not want to receive long-term AAT. However, the development of resistance is the result in many cases of long-term use of AAT, which is inappropriate for financial reasons and due to the risk of developing the proarrhythmogenic effect of AAT. Therefore, we believe that RFA is indicated even when the patient agrees with its implementation, and the first prolonged paroxysm of TP is an absolute indication for RFA.
Types of atrial fibrillation and an example of a diagnosis
Clinically, atrial fibrillation manifests itself in several forms:
- paroxysmal, when an attack of fibrillation lasts no more than 48 hours in the case of successful treatment (cardioversion), or paroxysm is restored within 7 days;
- persistent - arrhythmia lasts more than a week, or fibrillation can be eliminated later than 48 hours with drug therapy and electrical stimulation;
- permanent form, when chronic fibrillation is not eliminated by cardioversion. Drug assistance in this case is ineffective.
Taking into account the heart rate data and signs of typical atrial fibrillation on the ECG, three variants of fibrillation are determined:
- normosystolic form - heart rate within 60-100 beats per minute;
- tachysystolic - heart rate more than 90 beats per minute;
- bradysystolic - heart rate less than 60 beats per minute.
The clinical diagnosis of the patient includes the characteristics of the arrhythmia and ECG data, which are deciphered: atrial fibrillation, persistent form, tachysystolic variant.
Mechanism of atrial flutter
Typical atrial flutter (isthmus-dependent) - a re-entry loop in the right atrium around the tricuspid valve annulus counterclockwise
Atypical flutter:
- loop around the tricuspid valve annulus in a clockwise direction (isthmus dependent)
- the loop captures additional areas of the myocardium (not isthmus-dependent)
- re-entry loop in the left atrium - around the mitral valve annulus (not isthmus dependent)
Fig.1. Formation of a re-entry loop during atrial flutter.
Treatment tactics
- Drug therapy is the prescription of special drugs to relieve attacks of arrhythmia and prevent their occurrence.
- Radiofrequency ablation is a minimally invasive surgical treatment for cardiac arrhythmias. The procedure begins with constructing an electrical model of the atrium and determining the localization of sources of pathological excitation. During the intervention, a catheter is inserted through the patient's femoral vein into the atrium cavity. Electrical isolation of the pulmonary veins is then performed using catheter radiofrequency lesions. The procedure is performed under local anesthesia and takes about two hours.
Radiofrequency ablation (RFA)
When a person has an abnormal pulse and develops arrhythmia as a result of a number of cardiovascular diseases, he needs to undergo a comprehensive examination. Doctors often recommend using the catheter ablation method, that is, RFA of the heart. They made this choice largely due to the wide list of advantages of the technique with a minimum number of disadvantages. Therefore, this heart operation is considered one of the best.
It involves neutralizing cells that cause rhythm disturbances with electric current. The latter's access to the heart is provided by a catheter. The operation is not surgical and is considered minimally invasive. It is performed under local anesthesia.
The source of arrhythmia is destroyed using high-frequency (or radio frequency) current of 400-500 kHz.
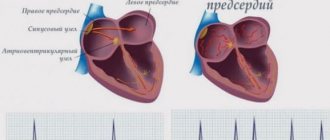
How to diagnose atrial fibrillation using an ECG
Fibrillation is characterized by a tachyarrhythmia-like heartbeat, rapid, irregular pulse and heart contractions.
Most patients experience chest tremors and weakness. A distinctive symptom is an inconsistent pulse. But sometimes atrial fibrillation is asymptomatic, and therefore an electrocardiogram is considered the standard method for detecting heart rhythm disturbances. The main signs of atrial fibrillation on the ECG (photo 1):
- P waves are not recorded in all 12 leads, since the impulses pass chaotically through the atria;
- small random f waves are determined, most often recorded in leads V1, V2, II, III and aVF;
- ventricular QRS complexes become irregular, a change in the frequency and duration of the R-R intervals is observed, AV block is detected against the background of a low frequency of ventricular contraction - bradyform fibrillation;
- QRS complexes do not change, without deformation or widening.
Photo 1: Example of an ECG with atrial fibrillation.
Arrhythmia is manifested by rapid or slow contraction of the heart. Atrial fibrillation on the ECG is divided into two types:
- in the tachysystolic variant, electrocardiography reflects a heart contraction of more than 90 beats per minute (photo 2);
Photo 2: Tachysystolic form of AF.
- bradysystolic variant - contractions less than 60 beats per minute. (Fig. 3);
Photo 3: Bradysystolic form of AF.
With arrhythmia, contractions arise from different sections of muscle fibers, ectopic foci, as a result of which there is no single contraction of the atria. Against the background of hemodynamic failure, the right and left ventricles receive insufficient blood volume, cardiac output decreases, which determines the severity of the disease. Decoding the cardiogram helps to establish the exact heart rhythm disorder.
A characteristic sign of fibrillation on the ECG is f waves (large-wave and small-wave):
- in the first case, fibrillation is determined by large waves, atrial fibrillation reaches 300-500 per minute;
- in the second, the flicker waves become small, reaching 500-700 per minute.
Atrial flutter is a variant of slower contraction of the heart muscle, in the range of 200-300 beats per minute. Patients with persistent atrial fibrillation experience frequent flutter recurrences. Such an emergency requires urgent medical attention.
Analysis of cases of paroxysms shows that on average, in 10% of patients, an attack of atrial fibrillation turns into flutter, which is determined on the ECG in the form of the following description:
- the absence of P waves and the replacement of small f waves with large sawtooth waves F is the main characteristic, which is presented in photo 4;
- normal ventricular QRS complexes.
Photo 4:
ECG No. 1
Pay attention to leads V1 and V2; instead of an isoline, F waves, similar to saw teeth, are clearly visualized in them. They move rhythmically at an interval of FF = 8.5 to small cells, that is, their frequency is about 350 per minute . Of course, under normal conditions * , the AV node is not able to transmit such a frequency to the ventricles, and therefore some of the waves are blocked. If there is one ventricular complex for every two waves, this flutter is called 2:1, if there are three waves, then 3:1, etc.
In this case, every fourth wave is carried out to the ventricles, that is, we are talking about a 4:1 flutter.
This is what a typical flutter looks like, and in this form its diagnosis is not difficult. But when the contraction frequency (AV conduction) increases, say 2:1, difficulties may arise. Look at ECG #2.
Complications of the disease
In atrial fibrillation, the upper chambers of the heart are not fully filled with blood, causing reduced output and heart failure.
WPW syndrome with early excitation of the ventricles provokes the development of supraventricular arrhythmia, worsening the course of the disease and making it difficult to diagnose cardiac arrhythmias.
In addition to reducing the blood filling of the cavities of the heart, the chaotic contraction of the atria forms clots and thrombi, which, with the blood flow, enter the small and large vessels of the brain. Thromboembolism is dangerous due to complete closure of the arteriole and the development of ischemia, which requires resuscitation measures and initiation of treatment as soon as possible.
Basic principles of treatment
Modern therapy for arrhythmia is based on methods of restoring the heart rhythm to sinus and preventing new attacks of paroxysms with the prevention of thrombus formation. The provisions of the medical care protocol include the following items:
- antiarrhythmic drugs are used as medicinal cardioversion to normalize heart rhythm;
- beta-blockers are prescribed to control heart rate and the quality of contraction of the heart muscle (contraindication - patients who have a pacemaker implanted);
- anticoagulants prevent the formation of blood clots in the heart cavity and reduce the risk of stroke;
- metabolic drugs act as a stabilizer and improve metabolic processes;
- Electrical cardioversion is a method of electrical impulse relief of an attack of atrial fibrillation. To do this, atrial fibrillation is recorded on an ECG and defibrillation is performed under the control of vital signs. The only criterion for prohibiting such a procedure is severe bradycardia and persistent fibrillation for more than two years.
ECG No. 2
This is a typical flutter of 2:1 and 3:1, the F waves are poorly visible, but if you look, you can notice them (note that I separately highlighted the F wave in red . This is how the impulse passes through the atria, turn on your imagination and superimpose this segment on the main ECG and everything will become clear.
As you can see, the wave frequency is 375 per minute. Some alteration of the R waves is confused with irregularity, in which case it is probably not a big mistake to call it “atrial fibrillation-flutter”. But still, this is trembling.