The left atrial appendage is a muscular bursa connected by a lumen to the left atrium and is part of the normal anatomy of the heart. However, in most cases, it is the left atrial appendage that is the main source of blood clots and thrombotic complications in patients with atrial fibrillation.
Atrial fibrillation (AF) is a major risk factor for the formation of blood clots (thrombi), which can block blood flow to the brain and lead to cerebral infarction (stroke).
How the left atrial appendage is associated with stroke in patients with AF
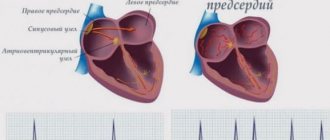
With AF, disruptions occur in the conduction system of the heart and irregular electrical impulses occur in the upper parts of the heart (atria), which leads to their trembling and irregular contraction. Irregular heartbeats lead to decreased blood flow, rapid heart rate, difficulty breathing, and shortness of breath. These irregular heartbeats lead to an increased risk of developing blood clots. The left atrial appendage has a long, tubular shape and connects to the left atrium. During AF, blood can pool in the atrial appendage and lead to the formation of blood clots. When the heart rhythm returns to normal, these blood clots can fly out of the appendage into the left atrium and then travel through the blood throughout the body, causing blockage of arteries in the brain and leading to the development of a stroke.
Uniqueness of the operation
Surgically isolated left atrial appendage has an advantage over conservative treatment methods in patients with persistent or paroxysmal atrial fibrillation. After surgery, 70% of patients maintain sinus heart rhythm during a long observation period. Clinical signs of the disease are significantly reduced, and overall well-being improves.
This operation is unique and is performed in only a few institutions in Russia. In our center, this operation is performed by the head of the department of x-ray surgical methods of diagnosis and treatment - Sergey Vladimirovich Korolev.
Specialists of the cardiac surgery department of the Federal Scientific and Clinical Center of the Federal Medical and Biological Agency successfully use advanced methods of treating cardiac arrhythmias. Our clinic performs unique minimally invasive operations, as well as high-quality diagnostics of various forms of arrhythmia, coronary heart disease and other cardiovascular diseases.
Our center provides services for mammary coronary bypass surgery, thoracoscopic isolation of the ostia of the pulmonary veins, the posterior wall of the left atrium and suturing of the appendage. As a result of these procedures, hundreds of patients annually manage to prevent a number of serious complications: such as stroke, heart attack, heart failure.
You can obtain more detailed information about other methods of treating cardiovascular diseases at the Cardiology Center of the Federal Scientific and Clinical Center of the Federal Medical and Biological Agency of Russia.
How is left atrial appendage occlusion performed?
The procedure is performed using an endovascular, minimally invasive technique in a cath lab. By puncturing the femoral vein (usually on the right), the x-ray surgeon inserts a thin, flexible and long tube (catheter) into the right side of the heart. Next, puncture of the interatrial septum is performed and special instruments are carried out to the mouth of the left atrial appendage. During the entire procedure, X-ray images, as well as transesophageal echocardiography (TEE-CG) data, are used to monitor the implementation of instruments and their correct placement in the cavities of the heart.
Thoracoscopic isolation of the left atrium
This type of operation is performed in situations where traditional catheter ablation is impossible or ineffective. The impact on the heart is carried out through the inserted thoracoscope. Through 6-8 punctures in the chest area (symmetrically on the right and left), electrodes are inserted. High-frequency current destroys the source of arrhythmia. At the same time, in case of a blood clot, the left atrial appendage is sutured to prevent re-formation of clots, as well as reduce the risk of strokes and heart attacks.
The procedure is performed under anesthesia. Its distinctive features:
- high efficiency (75-96%);
- low morbidity;
- no need for artificial blood circulation and long-term hospitalization;
- short rehabilitation period, low risk of complications;
- rare relapses (less than with other methods).
A relative contraindication for treatment is severe heart disease (decompensated ischemic disease, valvular pathology), requiring more extensive surgical interventions.
Preparing for the study
Before the procedure, a consultation with a cardiologist and/or a neurologist is necessary, who will tell you in detail about all stages of the study, possible results and complications. A detailed allergy history is also collected to determine if there is an allergy to medications and/or contrast used during the procedure.
Your doctor will tell you which medications you are taking to stop taking on the day of your procedure. The patient should not independently decide to stop taking medications and can do this only after agreement with the cardiologist. It is advisable to avoid taking liquids and food several hours before the procedure.
Preparation for the procedure
Before performing the procedure, it is necessary to exclude complicating factors and determine the shape and size of the left atrial appendage. To do this, transesophageal echocardiography is first performed in 4 projections. The study allows you to examine in detail the parts of the heart, coronary vessels, and aortic arch. Clarification of the anatomical features is important in order to correctly select the type and diameter of the occluder, so that the occlusion of the appendage located at the left atrium is successful.
It is also necessary to undergo a number of standard tests for hospitalization:
- general analysis of urine and blood;
- photo of the lungs;
- cardiogram;
- blood biochemistry;
- tests for infections (hepatitis, syphilis, HIV).
Taking medications before and after surgery is agreed with the doctor. If necessary, additional studies and consultations with related specialists are prescribed. A few hours before the intervention, the consumption of food and liquid is excluded.
At a preliminary consultation, an arrhythmologist from the Federal Scientific and Clinical Center of the Federal Medical and Biological Agency will answer all your questions about the features, stages of the procedure and its results.
What is the Amplatzer Cardiac Plug Occluder?
The Amplatzer Cardiac Plug is a device specifically designed for non-surgical, low-impact closure of the left atrial appendage.
The device is folded into a thin catheter (~4 mm in diameter) and delivered folded to the left atrial appendage. Next, the occluder is released from the catheter and takes on the shape as shown in the figure.
The occluder is securely fixed to the delivery cable and, if necessary, the x-ray surgeon can repeatedly remove the occluder again into the lumen of the catheter until he is sure that the occluder is securely fixed in the cavity of the ear. Only after this is the occluder disconnected from the delivery device.
Amplatzer Cardiac Plug is manufactured at the plant in Minnesota (USA) from a special alloy Nitinol (nickel-titanium alloy). Nitinol is absolutely not susceptible to corrosion, its strength exceeds both titanium and steel, and also has a special property of “shape memory”, when, when straightened, it acquires its original shape as shown in the figure.
What happens after the occluder installation procedure
Because the occluder procedure is minimally invasive, recovery is likely to be quick and easy. Many patients are discharged from the hospital within the next 48 hours, with subsequent medication recommendations to continue treatment and recovery in an outpatient setting. It is necessary to conduct a control TEE-CG 3 and 6 months after installation of the occluder to monitor the process of endothelialization of the installed device. Endothelialization is the growth of the occluder with connective tissue and, in fact, its ingrowth into the wall of the heart. This is a normal and desirable process. In 99% of cases, complete endothelialization of the occluder occurs within several months. The patient returns to his normal lifestyle within the first month.
Is it possible to travel with an implanted device? Will there be problems going through the metal detector at airport security?
The metal parts of the Amplatzer Cardiac Plug are very small and will not normally trigger an alarm in an airport metal detector frame. However, for your comfort and peace of mind, you will be given a special card confirming the fact that the occluder has been installed.
Will an MRI interfere with or disrupt the occluder?
Most modern devices do not in any way affect the operation of the occluder, and the presence of an occluder does not affect the operation of the devices. However, it is best to alert staff to the presence of implanted devices before undergoing any medical procedure. Magnetic resonance imaging (MRI) is acceptable and the Amplatzer Cardiac Plug will not affect the performance of an MRI in any way, even at 3 Tesla. It is necessary to inform the staff of the MRI department about the presence of an implant.
Is the procedure possible for pregnant women and nursing mothers?
The risk of exposure of a child to X-ray radiation and the benefits of treatment must be weighed, and the correct and most effective tactics must be adopted. If it is necessary to implant a device during pregnancy, all possible measures will be taken to minimize radiation exposure to the fetus and mother.
There is no evidence of the effect of installing an occluder on the lactation process in nursing mothers.
Rehabilitation period after installation of an occluder in the left atrial appendage
Intensive observation and monitoring is carried out for 6 hours after implantation:
- blood pressure;
- heart rate;
- blood oxygen saturation;
- neurological status.
The patient is discharged from the hospital provided hemodynamics are stable and there is no risk of complications. At the same time, during the rehabilitation period it is important to control the process of implantation of the occluder into the tissue. During the first week, the remaining elements of the ear are thrombosed. Endothelialization then occurs over several weeks. Scarring is completely completed after six months.
Until complete healing, all patients must continue treatment with anticoagulant drugs. The regimen and combination of drugs are selected individually, taking into account individual indications and contraindications. Discontinuation of medications in this group is carried out under the supervision of a doctor and depends on the quality of the closure of the ear. Only after scarring is complete, patients are transferred to continuous use of aspirin (at a dose of 75 mg).
Transesophageal ultrasound is performed on the 45th day and six months later. If a hole is detected, coagulants are continued with subsequent observation and examination every 6 months until the fistula is completely closed.
Possible complications associated with the Amplatzer Cardiac Plug installation procedure
There are some potential risks associated with the placement of an occluder, as well as additional risks associated with the vein puncture procedure itself. It is necessary to consult with a radiologist about the possible risks of implanting the device.
Potential risks include, but are not limited to the following:
- air embolism (an air bubble that can move through the vessels and block the work of some of them);
- allergic reactions to contrast;
- allergic reaction to anesthetic drugs;
- cardiac arrhythmias (the occurrence of irregular heart rhythms);
- bleeding;
- heart failure;
- cardiac tamponade (rupture of the heart muscle);
- death;
- fever;
- hypertensive or hypotensive reactions of the body;
- infections;
- multiple organ failure;
- myocardial infarction (heart attack);
- perforation of the heart cavity or vessel;
- pericarditis (excess fluid in the pericardial sac);
- renal failure/renal dysfunction;
- cerebrovascular accidents (temporary or permanent);
- arterial thrombosis;
- valvular regurgitation or insufficiency.