Our expert - cardiologist-neonatologist, head of the department of pathology of newborns and premature babies No. 2 of the National Research Medical Center for Obstetrics, Gynecology and Perinatology named after V. I. Kulakov, Doctor of Medical Sciences Ekaterina Bockeria.
Every year in the world (and in Russia too), 8–10 out of 1000 children are born with congenital heart defects (CHD). Heredity is not the leading cause of their development. Nevertheless, when severe defects are detected, doctors recommend that parents undergo genetic testing. By the way, in some syndromes, congenital heart defects are more common (children with Down syndrome have them in 70% of cases).
Why is the physiological maturity of a newborn more important than a healthy weight or being born at term?
The most common criterion by which young mothers assess the condition of their baby is height and weight.
Born 3500 grams and 54 cm - a “hero”, and if 2800 grams - then sympathy and words of support immediately appear in the eyes of those around him: “It’s okay, he’ll gain more, but the birth went well.” But is it really important how much a baby weighs at birth? How will his height and weight affect his further development, resistance to diseases and psycho-emotional state?
Neonatologists and pediatricians, who have been observing the growth and development of children for years, have come to the conclusion that external signs in the form of weight and height do not provide much information about the child. Much more important is physiological maturity.
To wait or not to delay?
A quarter of the defects are critical, for which surgery must be done immediately after birth. You can wait with other types of them. And there are also defects (for example, small defects of the interventricular septum of the heart) that often close on their own over time.
Previously, such children were diagnosed with a huge delay and often when it was too late to do anything. But with the advent of high-quality ultrasound diagnostics, many congenital heart defects are detected even at the stage of intrauterine development. And, although a definitive diagnosis can only be made at birth, such a diagnosis is extremely important.
Sudden death - during physical education. Why do children die in class? More details
What is physiological maturity?
Physiological maturity implies the baby’s readiness for independent life outside the mother’s body. The concept extends to assessing the functioning of the main systems - nervous, cardiovascular, musculoskeletal, respiratory.
Even to a person far from science, it is obvious: in order for a baby to grow and develop harmoniously, his body must itself maintain a constant temperature, the lungs must exchange oxygen and carbon dioxide in the blood, and the heart must fully saturate all organs with blood.
Why is it so important to correctly assess physiological maturity? To preserve it in mature babies and help “mature” those who have deviations.
The more the baby corresponds to the concept of maturity, the less often he will get sick. Its correct development from the first days is insurance against endless viral infections, allergic reactions to drugs and diathesis.
Phases of the disease
CHD occurs in three phases:
- first phase: during it, a compensatory and adaptive reaction to a failure in the dynamics of blood circulation is observed; in case of a serious violation, myocardial hyperfunction occurs.
- second phase: relative compensation occurs. The child’s motor activity and physiological development improves.
- the third phase is terminal. The body has already exhausted the possibilities of compensation; degenerative, dystrophic pathologies of the heart and nearby blood vessels are developing. If a child is sick, especially with complications, then the terminal phase occurs faster. Its outcome is only fatal. Source: E.E. Chepurnykh, E.G. Grigoriev Congenital heart defects // Siberian Medical Journal (Irkutsk), 2014, No. 3, pp. 121-127
Therefore, the earlier the pathology is detected, the more favorable its prognosis.
Musculoskeletal reflexes
These are motor reflexes that are characteristic of physiologically mature children. They represent the baby’s reaction to irritation of various parts of his skin.
- Robinson's reflex or "grasp" reflex
If you put an adult’s finger into the baby’s palm, he grabs it so tightly that the doctor can calmly lift the child on this finger. Because simultaneously with the contraction of the palm muscles, the overall tone of the body and all skeletal muscles are strengthened.
- Plantar reflex
The doctor touches the skin of the baby’s foot with line movements, that is, irritates it along the inner edge of the sole. In response to the impact, the baby extends the big toe and bends all the other toes. At the same time, it can be noted that the child bends his legs at the knee and hip joints, and the contractile activity of the remaining muscles of his body increases.
- Difficulty straightening the leg at the knee
If a child’s leg is bent at the hip joint, it is difficult to straighten at the knee joint. This is explained by the fact that in a physiologically mature infant, the tone of the flexor muscles always prevails over the tone of the extensor muscles.
- "Crawl"
If you put a child on his tummy and put your palm on his soles, he reflexively pushes away from it. A crawling effect is created, although the baby remains in place.
- Negative reaction to support
The baby, who is lifted vertically above the table, held under the arms, does not lean on it. Even if his legs are lowered to the table. The child bends his legs and pulls them towards his tummy.
- Heel reflex, or Arshavsky reflex
With moderate pressure on the baby's heel bone, a generalized reaction of the body occurs in the form of extensor motor activity, screaming and crying grimace.
- General motor activity of the baby
During sleep, physiologically mature infants exhibit spontaneous motor activity. It occurs due to periodic changes in the composition of the baby’s blood. Its manifestations are a separate trembling of the arms or trembling of the legs, more with a tendency to extension than to flexion.
Note!
It would seem that it is easier to check a baby’s reflexes during breastfeeding: the baby is busy, not distracted, and the reflexes arise independently. In reality, it turns out that when feeding, the severity of all the reflexes described above decreases. Therefore, such untimely testing may mistakenly classify a physiologically mature infant as immature.
- When sucking, you can check only one reflex - sucking: stroking the baby's cheeks leads to increased sucking.
While eating, shuddering, flapping of arms and other physical activity of the baby are the absolute norm. Babies who actively move their limbs during feedings gain weight and grow in length faster. If the baby is swaddled tightly so that he does not “scare himself” while eating, the processes of metabolism in his body and growth slow down sharply.
Muscle activity, which is triggered and regulated by the child’s nerve centers, is the main factor on which the further development of his brain, the increase in brain mass and the intellectual development of the baby in later life depend.
Respiration rate
The respiratory rate in infants who are physiologically mature is 35-42 breaths per minute.
Heart rate
A baby's heart beats 135-140 times per minute at rest. This surprising heart rate is the absolute norm for infancy.
Arterial pressure
Measuring blood pressure in mature newborns in the first days after birth shows values of 80-85 mm Hg. for “upper” pressure, and 45 mm Hg. for "bottom".
Nervous system
In physiologically immature children, the process of maturation of the nerve pathways - the formation of the myelin sheath around nerves and nerve fibers, or myelination - is not yet completed, therefore the conduction of nerve impulses to various organs and tissues is disrupted, which affects the viability of their functions. The peripheral nervous system is not sufficiently myelinated; bundles of nerve fibers are rare and unevenly distributed. Myelination normally continues in the postnatal period, i.e. after birth.
The walls of blood vessels in immature babies may consist of only one inner layer - the endothelium and do not contain smooth muscle tissue, collagen or elastin (especially if the mother has hypoxia during pregnancy and a deficiency of protein, iron, copper, vitamin C, etc.). That is, the formation of the connective tissue framework in the vascular wall does not end, which reduces resistance to hypoxia and increases the risk of developing intracranial hemorrhages.
In immature newborns, there is no mechanism for autoregulation of cerebral vessels due to the incomplete formation of vascular fibers. In addition, the metabolic activity of endothelial cells depends on the pathways that ensure the occurrence of oxidation processes, and therefore there is a high probability of their damage during hypoxia.
During childbirth, even without complications, the baby’s brain experiences significant stress. The pressure on the membranes of the brain becomes so strong that spasms, circulatory disorders, and hemorrhages in the brain can develop. These phenomena are more likely in premature and immature children due to immaturity of brain structures. To determine the degree of immaturity and damage to the central nervous system, the so-called neurological status of the newborn is described, which is determined by such factors as: behavioral state, muscle tone, motor activity, unconditioned reflexes, reaction to external stimuli.
Those with an immature nervous system have reduced motor activity and muscle tone, and are characterized by weakness and rapid decline of physiological reflexes. A slow reaction to stimulation is characterized by its prevalence throughout the entire body, weakness of active inhibition, and irradiation of the excitation process, i.e. irritation from one center spreads to another, but on a smaller scale. The immaturity of the cortex determines the predominance of subcortical activity: movements are chaotic, shudders, tremor (shaking) of the hands, clonus of the feet (convulsive muscle contractions in response to impact), twitching of the eyeballs, and transient strabismus may be observed.
We invite you to “SM-Clinic”
Our clinic’s staff includes some of the best specialists in the Northern capital. We employ experienced pediatricians and pediatric cardiologists who will promptly identify the presence of alarming symptoms and prescribe all the necessary examinations. “SM-Clinic” is well equipped; we can conduct all tests for the presence of congenital heart disease.
Make an appointment with us as soon as possible if you notice signs of congenital heart disease in your child. Time plays a huge role in this disease.
Sources:
- HER. Chepurnykh, E.G. Grigoriev. Congenital heart defects // Siberian Medical Journal (Irkutsk), 2014, No. 3, pp. 121-127.
- L.N. Falyush, V.V. Florensov. Risk factors for congenital heart defects // Clinical medicine. Bulletin of the All-Russian Scientific Center SB RAMS, 2010, No. 6(76), p.67-69.
- J. I. Hoffman, S. Kaplan. The incidence of congenital heart disease // JACC, 2002, Vol. 39, p.1890—1900.
The information in this article is provided for reference purposes and does not replace advice from a qualified professional. Don't self-medicate! At the first signs of illness, you should consult a doctor.
Respiratory system
Due to the immaturity of the nervous system, as well as the lipid metabolism system, the derivative of which is surfactant - a surface substance that ensures the opening of the lungs during the first breath and their normal functioning in the future, physiologically immature infants often develop a syndrome of respiratory disorders, which is manifested by the development of atelectasis. Atelectasis are areas of collapsed or incompletely straightened lung tissue that do not participate in breathing and can cause respiratory failure. Such a child is transferred to artificial ventilation until the respiratory system begins to function on its own. Against the background of respiratory distress syndrome, various infectious diseases (pneumonia) often occur, which certainly worsens the child’s condition.
The cardiovascular system
The structure and function of the fetal heart in the prenatal period differs from that of a newborn child. The fetus has a three-chambered heart, special openings are open - the “oval window” and the “botal duct”, through which the blood is mixed and in utero the child receives only “mixed” blood, which allows him to be quite resistant to a possible lack of oxygen. After birth, a restructuring of blood circulation occurs and the heart becomes four-chambered and the child begins to receive purely arterial, not mixed blood. Of course, the “holes” do not close immediately, but “mixing” of blood through them does not occur from the first minutes of life. In a physiologically immature child, such a restructuring of the heart occurs much more slowly—additional openings and vessels (patent foramen ovale and ductus ductus botallis) can not only persist for a long time, but also function.
The pulse in immature newborns is very labile, weak in filling, frequency 120-160 per minute, but can reach 180. Since the cardiovascular system of immature babies is sensitive to external stimuli, you need to try to protect the baby as much as possible from them, for example, from loud sounds .
Types of heart defects
| Type | Name |
| Congenital | |
| Without the development of cyanosis (pale type) | Defects of the interventricular and interatrial septa |
| Patent ductus arteriosus | |
| Pulmonary stenosis | |
| Coarctation of the aorta | |
| With the development of cyanosis (blue) | Transposition of the great vessels |
| Common ventricle | |
| Tetralogy of Fallot | |
| Purchased | |
| Mitral valve (between the left atrium and ventricle) | Mitral stenosis |
| Mitral regurgitation | |
| Tricuspid valve (between the right atrium and ventricle) | Tricuspid valve stenosis |
| Tricuspid valve insufficiency | |
| Aortic valve (between the left ventricle and the aorta) | Aortic stenosis |
| Aortic insufficiency | |
| Pulmonary valve | Pulmonary valve stenosis |
| Pulmonary valve insufficiency | |
Stenosis
- narrowing of the valve opening, which causes difficulty in blood flow.
Failure
- inability of the valves to close tightly. In people with valve stenosis, valve insufficiency develops over time - this is called combined PS.
Septal disorders:
A condition in which the septum between the chambers of the heart is damaged:
- atrial septum -
“extra” blood enters the right atrium and causes it to enlarge; - interventricular
- blood flows from the right to the left ventricle, expanding its boundaries.
Changes are found in 2 out of 1000 newborns. Perhaps the most favorable form, since small defects can heal on their own.
Coarctation of the aorta:
Narrowing of the lumen of the main vessel in the area of the isthmus - the transition of the arch to the descending part. The defect causes disruption of the blood supply to organs. This form of pathology accounts for 10% of all defects. Often combined with disruption of interchamber septa. A serious condition requiring medical attention immediately after birth.
Pulmonary valve stenosis:
At the site of the valves from the right ventricle to the pulmonary artery, a narrowing occurs. The heart requires more effort to pump blood. 10% of the total number of defects.
Transposition of the great vessels:
Rare pathology (about 5%). In this case, the main vessels “change places.” Arterial blood flows through the veins, and venous blood through the arteries.
Tetralogy of Fallot:
The most severe form. Consists of four violations simultaneously:
- the opening between the left and right ventricles;
- pulmonary stenosis – narrowing of the pulmonary trunk;
- enlargement of the right ventricle;
- Aortic displacement is the exit of the aorta from the heart in an atypical location.
Circulatory system
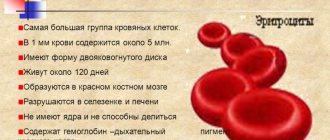
Due to the immaturity of bone marrow sprouts, as well as the low sensitivity of red bone marrow to erythropoietin (an active hormone of the kidneys that stimulates the production of red blood cells), lower levels of red blood cells and hemoglobin are observed in immature children, which leads to the development of early anemia of physiologically immature children, which develops during 2 first months of life. Rapid depletion of the white sprout leads to the development of neutropenia - a decrease in the number of neutrophils in the blood, especially in conditions of intra- and extrauterine infection of the child.
Physiologically immature newborns at birth have lower concentrations of vitamin K, vitamin K-dependent blood coagulation factors, and other disorders in the blood coagulation system. In this situation, bleeding from the first minutes of life can be combined with thrombosis due to the low activity of fibrinolysis and anticoagulants, which can lead to the development of DIC syndrome (disseminated intravascular coagulation syndrome).
Metabolic adaptation processes in immature infants are slowed down. They are more likely to experience hypoglycemia (low blood sugar), hypoxemia (low oxygen in the blood), hyperbilirubinemia (increased bilirubin in the blood serum), and early anemia in conditions of excess iron.
Digestive system
The digestive system of immature children also has a number of features. First of all, this is expressed in the immaturity of the enzyme system. The glands of the gastrointestinal tract do not produce the required amount of enzymes and gastric juice. When the gastrointestinal tract is colonized by microorganisms, even a small amount of pathogenic bacteria, which would normally be neutralized by the protective properties of gastric juice and pancreatic juice, causes dysbiosis in immature children (an incorrect ratio of certain microorganisms in the gastrointestinal tract).
Also, due to the immaturity of the nervous system and the transmission of nerve impulses, the motor function of the gastrointestinal tract suffers, and the movement of food through the gastrointestinal tract slows down. As a result, problems arise with the flow of food into different parts of the stomach and intestines and its excretion.
Features of the gastric tract in physiologically immature infants are:
- poor development of the sphincter at the entrance to the stomach, which leads to frequent regurgitation;
- poor development of longitudinal muscle bundles of the stomach wall, which causes lethargy and bloating due to overfeeding and exposure to air
- slow evacuation of stomach contents (130-140 min);
- high viscosity of original feces.
Despite the imperfection of the digestive system in physiologically immature infants, the gastric juice still contains rennet, which curdles milk. Therefore, mother's milk is mandatory for an immature child. In addition to its nutritional value, milk provides an invaluable service to protect the baby’s body from environmental aggression. Therefore, even if the child is immediately after birth in the intensive care unit or intensive care unit and receives parenteral nutrition (via a drip) or is so weak that he cannot breastfeed, it is necessary to take all possible measures to preserve breast milk, feed the baby from a spoon . This is one of the necessary factors when nursing immature babies.
In physiologically immature newborns, functional inferiority of the liver is possible; as a result, an insufficient amount of the enzyme glucurone transferase is produced, and this predisposes to the development of prolonged jaundice. A low level of prothrombin causes increased bleeding.
Immature children are predisposed to intestinal dysfunction. The intestinal wall has increased permeability, so microbes and toxins in the intestines are absorbed through the intestinal wall into the blood. Due to hypotension of the intestines and the anterior abdominal wall, flatulence is often observed; as a result, the diaphragm rises upward, squeezing the lower parts of the lungs and disrupting their normal ventilation.
The mucous membrane of the digestive canal in immature children is tender, thin, and easily vulnerable. There is low proteolytic activity of gastric juice, insufficient production of pancreatic and intestinal enzymes, as well as bile acids. All this complicates the processes of digestion and absorption, contributes to the development of flatulence and dysbacteriosis. Many immature children, even those who are breastfed, have a deficiency of intestinal bifid flora in combination with the carriage of opportunistic flora.
The nature of a child's stool is determined by feeding characteristics; As a rule, in the coprogram of physiologically immature children there is a lot of neutral fat.
Functional disorders of the gastrointestinal tract are one of the most widespread problems among children in the first months of life. A distinctive feature of these conditions is the appearance of clinical symptoms in the absence of any organic changes in the gastrointestinal tract (structural abnormalities, inflammatory changes, infections or tumors) and genetic metabolic abnormalities.
With functional disorders of the gastrointestinal tract, motor function, digestion and absorption of nutrients, as well as the composition of the intestinal microbiota and the activity of the immune system may change. The causes of functional disorders often lie outside the affected organ and are caused by a violation of the nervous and humoral regulation of the digestive tract.
Resuscitation and intensive care of newborns with asphyxia
There is no generally accepted definition of newborn asphyxia. The most informative and objective definition of asphyxia presented by N.P. Shabalov and co-authors (2003). They consider newborn asphyxia to be a syndrome characterized by the lack of efficiency of gas exchange in the lungs immediately after birth, the inability to breathe independently in the presence of heartbeats and (or) other signs of live birth (spontaneous muscle movement, pulsation of the umbilical cord).
Until the mid-1980s. the main criterion for diagnosing asphyxia was the Apgar score, which is reflected in the International Classification of Diseases, 9th revision (1975). However, in 1986, the American Academy of Pediatrics and the American College of Obstetricians and Gynecologists, based on numerous follow-up studies, concluded that Apgar scores at 1 and 5 minutes after birth are poorly correlated with both the cause of this condition and the prognosis and in themselves should not be considered as indicators of the manifestation or consequences of asphyxia.
At the same time, in a condition with a low Apgar score (0–3 points) that persists for 15 minutes, cerebral palsy is observed in 10%, and within 20 minutes - in 60% of patients.
Despite the critical attitude towards the Apgar score and contrary to the opinion that it should not be considered as a criterion for the diagnosis and severity of birth asphyxia (N.P. Shabalov et al., 2003), it is advisable to turn directly to the International Classification of Diseases 10- th revision (1993).
Rubric R 21. Asphyxia during childbirth
Note. This rubric should not be used for low Apgar scores without mention of asphyxia and other respiratory distress.
R 21.0. Severe asphyxia at birth.
The pulse at birth is less than 100 beats/min, slow or steady, breathing is absent or difficult, the skin is pale, the muscles are atonic. Asphyxia with an Apgar score of 0–3 points one minute after birth. White asphyxia.
R 21.1. Moderate and moderate asphyxia at birth.
Normal breathing has not been established within the first minute after birth, but the heart rate is 100 beats/min or more, there is little muscle tone, and there is little response to stimulation.
Apgar score 4–7 one minute after birth. Blue asphyxia.
There are also acute asphyxia, which is a manifestation of intrapartum hypoxia, and asphyxia, which developed against the background of chronic intrauterine antenatal hypoxia.
The incidence of asphyxia in newborns, according to various authors, varies within very wide limits, which is obviously due to the lack of a generally accepted definition. Thus, Carter et al (1993) believe that the frequency of asphyxia is 1–1.5%. In another 10–15% of cases, a low Apgar score is due to cardiorespiratory depression. In total, these states account for up to 16.5%. Approximately the same indicators for 2003 were published by the Ministry of Health and Social Development of the Russian Federation. At the same time, the mortality rate from asphyxia among full-term children is 0.2%, and among premature infants - 1.16%.
According to S. G. Ezutagan (1999), the frequency of perinatal asphyxia in premature infants is 30%, and in full-term newborns - 20%.
N. N. Volodin and S. O. Rogatkin (2004) report that every year in the world 4 million children are born in a state of asphyxia: 840 thousand of them die, and the same number subsequently suffer from persistent disorders of the functional activity of the central nervous system.
There are five main causes of newborn asphyxia.
- Disorders of the umbilical cord blood flow (true umbilical cord knots, compression of the cord, tight entanglement of the umbilical cord around the neck or other parts of the child’s body, loss of umbilical cord loops).
- Disorders of placental gas exchange (infarction, calcifications, edema and inflammatory changes in the placenta, premature placental abruption and placental previa).
- Insufficient hemoperfusion of the maternal part of the placenta (arterial hypotension or hypertension in the mother, disturbances in uterine contractility).
- Impaired maternal blood oxygenation (anemia, shock, cardiovascular and/or respiratory failure).
- Disturbances of early neonatal adaptation with inability to make a successful transition from fetal to postnatal circulation due to congenital malformations of the brain, cardiovascular and respiratory systems, prematurity and immaturity, congenital pneumonia or compression of the respiratory tract (for example, with a diaphragmatic hernia), birth injuries of the head and spinal cord, hydrops fetalis, congenital hypothyroidism, generalized congenital infections.
Hypoxemia, hypercapnia and associated acidosis are the leading links in the pathogenesis of asphyxia. They activate hemodynamic redistribution of blood volumes, secretion of stress-type hormones, production of cytokines, adhesion molecules and growth factors, and a cascade system of plasma proteases. These same factors, after reoxygenation, activate lipid peroxidation of cell membranes with the formation of arachidonic acid metabolites (prostaglandins and leukotrienes) and an increase in the content of cellular metabolites (adenosine, nitric oxide, endothelin, etc.).
Blood oxygen tension is below 40 mm Hg. Art. includes the so-called “ischemic reflex”, the chemoreceptor mechanism of which leads to simultaneous excitation of the vasomotor and respiratory centers, centralization of blood circulation, i.e. ischemia of the skin, lungs, kidneys, liver, gastrointestinal tract, for the sake of providing vital organs (heart, brain , diaphragm, adrenal glands).
In the process of centralization of blood circulation, in addition to adrenaline and norepinephrine, angiotensin II and vasopressin are involved.
High pulmonary vascular resistance, supported by hypoxemia and hypercapnia, causes pulmonary hypertension and blood shunting, respiratory failure, as well as overload of the right side of the heart with pressure, and the left side with volume.
The negative effect of hypoxemia, hypercapnia and centralization of blood circulation is the accumulation of under-oxidized products and severe mixed acidosis. Compensatory activation of anaerobic glycolysis with lactate accumulation further enhances acidosis. The latter has an extremely negative effect on systemic hemodynamics, microcirculation, hemorheology, water and electrolyte balance, and metabolic processes.
An increase in hypoxia and mixed acidosis causes the opening of precapillary sphincters, decentralization of blood circulation with a drop in blood pressure, i.e., hemodynamic collapse, which reduces tissue perfusion in vital organs.
In the vessels of ischemic tissues, platelets, endothelial cells, and monocytes are activated, which leads to the activation of a cascade of plasma proteases, as well as the release of cellular enzymes, pro- and anticoagulants, arachidonic acid metabolites, reactive oxygen species and nitric oxide, which are involved in damage to organ function.
Activation of the thrombin, fibrinolytic, kinin and complement systems leads to endotoxicosis by proteolysis products and, along with acidosis, to damage to cell membranes, mitochondria, lysosomes, the blood-brain barrier, increased vascular permeability, decreased vascular tone, cell destruction, edema of the interstitial space, sludge phenomenon, triggering intravascular coagulation, thrombosis, blockade of microcirculation, dystrophic processes, and ultimately, multiple organ failure.
Clinical signs and symptoms
With moderate asphyxia, a child is born with apnea or single gasps, with a heart rate of 90–160 beats/min, with reduced muscle tone and a reflex response to the nasopharyngeal catheter, with severe cyanosis (blue asphyxia). The general condition is assessed as severe or moderate. In the first minutes of life, the child is lethargic and quickly cools down. Poorly responds to inspection and irritation. Spontaneous motor activity is low. Physiological reflexes are suppressed. Auscultation of the heart often reveals tachycardia, muffled sounds, and an accent of the second tone over the pulmonary artery. Breathing is often with the participation of auxiliary muscles, auscultation is weakened, with an abundance of dry and moist rales of various sizes.
Often, already in the first hours of life, hyperexcitability, large-scale tremors of the hands, hyperesthesia, spontaneous Moro reflex, and short-term convulsions appear. At the same time, clinical signs of depression of the central nervous system increase in some patients. The dynamics of muscle tone, physiological reflexes, signs of depression or increased excitability of the nervous system are very individual and largely depend on the adequacy of assistance.
Severe asphyxia is characterized by the presence at birth of signs of stage II or III shock: there is no breathing or ineffective gasps are observed, pulse is less than 100 beats/min, the skin is very pale (white asphyxia), muscles are atonic, there is no reaction to the nasopharyngeal catheter, the “white spot” symptom » more than 3 s, arterial hypotension.
The general condition is assessed as severe or extremely serious.
In the first hours and days of life, the clinical picture is caused by multiple organ failure. From the central nervous system: hypoxic-ischemic encephalopathy, cerebral edema, intracranial hemorrhage, convulsions.
From the lungs: meconium aspiration syndrome, pulmonary hypertension, type II respiratory distress syndrome.
From the cardiovascular system: shock, hypotension, polycythemia, hypervolemia or hypovolemia, pathological shunting of blood, tricuspid insufficiency, ischemic necrosis of the endocardium/myocardium.
From the excretory system: oliguria, acute renal failure with or without renal vascular thrombosis.
From the gastrointestinal tract: functional obstruction, vomiting, regurgitation, liver dysfunction, necrotizing enterocolitis.
From the endocrine system: transient insufficiency of the sympathetic-adrenal system, thyroid gland, adrenal glands.
All this is accompanied by disturbances of homeostasis (decompensated acidosis, hypoglycemia, hypocalcemia, hypoantremia, hypomagnesemia) and hemostasis (thrombocytopenia, DIC syndrome).
Secondary immunodeficiency, accompanying multiple organ failure, contributes to the activation and generalization of intrauterine infections, as well as the development of hospital infections.
Diagnosis and recommended clinical studies
The criteria for severe asphyxia are:
- severe metabolic or mixed acidosis (pH less than 7.0) in the blood from the umbilical artery;
- Apgar score 0–3 points more than 5 minutes;
- multiple organ disorders;
- clinical neurological consequences in the early neonatal period, including seizures, coma or hypoxic-ischemic encephalopathy.
Important criteria for the severity of asphyxia are the response to adequate therapy, as well as the course and outcome of the pathology in the early neonatal period, reflecting the severity of damage to vital functions. Consequently, the final severity of asphyxia is diagnosed not immediately after birth, but at the end of the early neonatal period.
Required amount of research:
- monitoring of blood pressure, body temperature, heart rate, respiratory rate, acid-base status, carbon dioxide and oxygen tension in the blood, hemoglobin oxygen saturation, hematocrit, blood glucose;
- neurosonography;
- biochemical blood test: sodium, potassium, calcium, magnesium, total protein, glucose, creatinine, urea, bilirubin.
The optimal option is Doppler ultrasound determination of central and cerebral hemodynamics.
Taking into account the need for a differential diagnosis with severe infectious diseases, microbiological and virological studies are indicated.
Differential diagnosis must first be carried out with the following conditions:
- birth injury of the central nervous system;
- damage to the nervous system due to congenital infections (cytomegalovirus and herpetic infections, toxoplasmosis, syphilis, ECHO viruses, etc.);
- dismetabolic and toxic-metabolic disorders of the central nervous system;
- malformations of the central nervous system;
- lung malformations, diaphragmatic hernia;
- cardiorespiratory depression caused by maternal drug administration.
General principles of treatment
Carrying out resuscitation measures for asphyxia of newborns is regulated by the order of the Minister of Health and Medical Industry of the Russian Federation “Primary and resuscitation care for a newborn in the delivery room” (1995).
When providing resuscitation care to a newborn, the following sequence of actions must be strictly observed:
- predicting the need for resuscitation measures and preparing for their implementation;
- assessment of the child’s condition immediately after birth;
- restoration of free airway patency;
- restoration of adequate breathing;
- restoration of adequate cardiac activity;
- administration of medications.
During primary resuscitation, medications are prescribed in the absence of a heartbeat and in cases where, despite artificial ventilation of the lungs (ALV) with 100% oxygen and chest compressions performed for 30 s, the child maintains bradycardia below 80 beats/min. .
The following drugs are used: adrenaline hydrochloride solution, drugs that replenish the volume of circulating fluid (albumin solution 5%, isotonic sodium chloride solution, ringer's solution), sodium bicarbonate solution 4%.
Epinephrine hydrochloride is a synthetic analogue of adrenaline adrenaline. It has an adrenopositive effect, exerting a stimulating effect on α- and β-adrenergic receptors. The inotropic cardiotonic effect of adrenaline is associated with its effect on β1-adrenergic receptors localized in the myocardium. This leads to increased strength and heart rate. Along with this, adrenaline, acting on α-adrenergic receptors, increases peripheral vascular resistance and blood pressure, thereby increasing coronary blood flow and blood supply to the myocardium.
The bronchodilator effect of adrenaline is due to its effect on β2-adrenergic receptors.
The indications are as follows:
- heart rate less than 80 beats/min after 30 seconds of mechanical ventilation with 100% oxygen simultaneously with chest compressions;
- Absence of heartbeat in the baby at birth. In this case, adrenaline is administered simultaneously with the start of mechanical ventilation and chest compressions.
Adrenaline is administered to newborns at a dilution of 1:10,000 in a volume of 0.1–0.3 ml/kg body weight (0.01–0.03 mg/kg) intravenously or endotracheally. When administered through an endotracheal tube, additional dilution with saline solution (1:1) is required. Adrenaline is administered intravenously as a stream.
As a result, there should be an increase in heart rate to 100 beats/min and higher 30 s after drug administration. If the heart rate remains less than 100 beats/min, the administration of epinephrine should be repeated. In the absence of effect and signs of general blood loss or hypovolemia, it is necessary to administer circulating blood volume replenishers.
Indications for replenishment of circulating blood volume are blood loss and hypovolemia. The following symptoms are observed:
- pale skin;
- “white spot” symptom for 3 s or more;
- weak pulse filling;
- muscle hypotension;
- arterial hypotension;
- lack of effect from the measures taken.
Circulating blood volume restorers (isotonic sodium chloride solution, 5% albumin solution, Ringer's solution) are administered to newborns during primary resuscitation into the umbilical cord vein at the rate of 10 ml/kg body weight for 5–10 minutes.
Expected effect:
- reduction of pallor;
- increase in pulse filling and heart rate;
- increased blood pressure;
- reducing acidosis by improving microcirculation in tissues.
Indications for the use of sodium bicarbonate:
- confirmed decompensated metabolic acidosis (pH < 7.0; BE > –12);
- lack of effect from mechanical ventilation, chest compressions, adrenaline and replenishment of circulating blood volume (in this case, deep acidosis is assumed, depressing cardiac activity and respiration).
A 4% sodium bicarbonate solution containing 0.5 mEq/ml is used. It is prescribed at a dose of 2 mEq (4 ml of 4% solution) per kg of body weight. Injected into the umbilical cord vein against the background of mechanical ventilation at a rate not exceeding 1 mEq/kg/min.
Expected effect: increase in heart rate to 100 or more beats per minute while reducing metabolic acidosis.
The positive effect of resuscitation measures - within the first 20 minutes after birth, adequate breathing, normal heart rate and skin color are restored - serves as the basis for stopping mechanical ventilation and chest compressions. However, resuscitation in the delivery room is only the first stage of providing assistance to children born with asphyxia.
Further observation and treatment of newborns who have suffered asphyxia, including children who have not recovered adequate breathing, have convulsions, and central cyanosis, are carried out in the intensive care unit.
With intravenous administration of sodium bicarbonate solution against the background of inadequate ventilation, increased acidosis may occur, and excessive administration of this drug leads to hypernatremia and the risk of developing intraventricular hemorrhages.
Effective cardiopulmonary resuscitation for asphyxia is the main factor that improves the prognosis. With moderate and moderate asphyxia, the prognosis is usually favorable. In severe asphyxia, persistently low Apgar scores (0–3 points) at 10, 15 and 20 minutes correlate quite closely with an unfavorable outcome and indicate an increased risk of death (60% in full-term newborns and 50–100% in children with very low body weight).
Literature
- Volodin N.N., Rogatkin S.O. Modern approaches to complex therapy of perinatal lesions of the central nervous system in newborns // Pharmateka. 2004. No. 1 (80). pp. 72–82.
- Dementyeva G. M., Ryumina I. I. Drug therapy during primary resuscitation of newborns: a guide to pharmacotherapy in pediatrics and pediatric surgery. Neonatology. M.: Medpraktika-M, 2004. pp. 21–23.
- Shabalov N.P., Lyubimenko V.A., Palchik A.B., Yaroslavsky V.K. Asphyxia of newborns. M.: Medpress-inform, 2003. 367 p.
- Ezutagan S. G. Perinatal asphyxia: materials of the conference “Primary and resuscitation care for newborns in the delivery room. Results of the implementation of Order No. 372 of the Ministry of Health of the Russian Federation. Problems. Development prospects". Samara, 2000.
A. G. Antonov, Doctor of Medical Sciences, Professor of the Scientific Center for Gynecology and Pediatrics of the Russian Academy of Medical Sciences, Moscow
Skeletal system
In physiologically immature children, the skeletal system is formed by birth, but bone mineralization is often not yet complete, and therefore they additionally need calcium (as recommended by a doctor).
And in prematurely born immature children there is often a deficiency of vitamin D, since it is in the last months of pregnancy that a supply of substances such as vitamin D, calcium, and phosphates occurs. If mom gets all this in abundance. A reduced amount of these substances in the body causes the development of diseases such as rickets, the signs of which are softening of the bones, slowing down of growth processes, especially of the legs, late appearance of teeth and closure of the large fontanelle, changes in the pelvic bones, as well as hip dysplasia, when due to lack of calcium, the femurs become deformed. Physiologically immature children are at risk for developing this disease. In them it is especially acute and progresses quickly. Therefore, physiologically immature children are often prescribed vitamin D to prevent rickets.
It happens that physiologically immature children are born with unformed hip joints. Dysplasia (underdevelopment) of joints threatens further subluxations, dislocations and deprivation of the ability to move independently. Therefore, it is necessary to diagnose this pathology in time and prescribe treatment. To detect dysplasia, an ultrasound examination of the joints is performed, which allows for a correct diagnosis. A common cause of joint dysplasia is a mother’s deficiency of magnesium, iron, protein, vitamin C and other nutritional factors during pregnancy.
Killer virus
If congenital heart disease is detected, the cardiologist will determine further tactics. If the defect is not critical, then the patient will be regularly monitored by doctors. They will prescribe treatment and determine the timing of surgery. If the child is in good health and condition, the cardiologist may allow massage and therapeutic exercises.
In addition, a child with congenital heart disease must be vaccinated (due to reduced blood circulation, infections stick to him).
In addition to vaccinations common to all children, children with congenital heart disease and some other children under 1 year of age need protection against respiratory syncytial virus (RSV infection). For them, this virus can be fatal, as it causes dangerous changes in the lungs, fraught with severe bronchitis and even pneumonia.
Article on the topic
Diseases from childhood. It is important to identify heart pathologies as early as possible
Children are also at risk:
- premature babies (especially those born before the 32nd week of pregnancy);
- with immunodeficiency;
- with Down syndrome.
During the first six months (and children with congenital heart disease - throughout the entire first year of life) during the dangerous season (from October to May), they must be immunized by injecting a special drug containing antibodies to the virus once a month.
Genitourinary system
Water-mineral metabolism in physiologically immature newborns is labile, so children are equally predisposed to the formation of edema and the development of dehydration (dehydration).
Early edema develops in utero or in the first hours and days after birth. In the pathogenesis of edema, in addition to renal factors, hypoproteinemia plays a significant role, which is important in maintaining plasma oncotic pressure. Clinically, early edema is expressed in mild tissue infiltration (from general pastiness to massive generalized edema that does not have a specific localization). They disappear 1-2 weeks after birth.
Late edema appears 2-3 weeks after birth and is characterized by a specific localization: on the thighs, legs, feet, pubis, lower third of the abdomen. They are dense to the touch, with smooth, shiny, low-elastic skin. The appearance of edema is associated with the nature of feeding, with illnesses of the child or with severe hypoproteinemia (low levels of proteins in the blood).
The immune system
The immune system of a physiologically immature child is already capable of responding when encountering foreign microorganisms, but this response can also proceed inadequately, violently, or, conversely, with a delayed reaction. In subsequent periods of the child’s development, an increased allergic mood of the body is observed, and various types of diathesis arise in such children. There is also a reduced ability to produce substances that provide protection to the mucous membranes, so infectious agents more easily, compared to a full-term baby, damage these membranes, causing focal infections. High sensitivity to viral infections. In 60-80% of cases they occur in an asymptomatic manner.
Causes of pathology
CHD may develop if:
- parents smoke;
- parents drink alcohol;
- the fetus is affected by external factors during the period of development and formation (high background radiation, lack of vitamins, viruses carried by the mother, polluted air, water, a number of chemicals, including heavy metals). Source: L.N. Falyush, V.V. Florensov Risk factors for congenital heart defects // Clinical medicine. Bulletin of the All-Russian Scientific Center SB RAMS, 2010, No. 6(76), p.67-69
Thermoregulation system
In physiologically immature children, it is extremely imperfect. This is due to a number of reasons: first of all, the immaturity of the central mechanisms for regulating heat exchange (namely the hypothalamus), as well as the anatomical and physiological characteristics of these children. Their body temperature is subject to cooling and overheating depending on the temperature of the external environment.
Excessive warming of a physiologically immature child leads to overheating due to the imperfection of the thermoregulatory center. At the same time, they do not have an adequate increase in body temperature to respond to the infectious process. Underdevelopment of sweat glands also contributes to overheating.
In adolescence, “immature” infants are more likely than others to suffer from mental inferiority.
85% success
Only a small proportion of children with congenital heart disease can be operated on endovascularly (when the surgeon inserts instruments through a vessel, without cutting the chest). In other cases, surgery is performed on an open heart using artificial circulation. This surgery is difficult, but rewarding. After all, 85% of children with congenital heart disease who were operated on in a timely manner successfully survive the 18-year mark and enter adulthood. They get a profession, play sports, start families and have children. While without surgery they would have no chance of life.
Unfortunately, there are defects for which radical, that is, complete, correction is impossible, and such patients require not one, but several complex operations. But even if in the end the child does not become completely healthy, nevertheless, such treatment will help save his life and improve its quality.
Heart surgeries are performed in large cardiology centers and are classified as high-tech medical care. Despite this, they are carried out free of charge as part of the state guarantee program, or, as people say, according to quotas. But if the child and his parents are citizens of another state, then the treatment will have to be paid either at their own expense or with the help of charitable foundations.
Maximum adherence to regimens that meet the needs and rhythms of the newborn!
Early and regular latching of the baby to the breast should not be ignored, even if after this latching the baby is bottle-fed. The connection between mother and baby helps him better adapt to the conditions of the “new” environment. The later breastfeeding is started, the worse it is for the baby. Delaying feedings for 2-4 days from the moment the baby is born can have a negative impact: a baby recognized as physiologically mature at birth will show signs of physiological immaturity.
For mothers whose child was born physiologically mature, it is very important to have adequate nutrition for absolutely all ingredients: protein, carbohydrates, saturated and polyunsaturated fats, vitamins, microelements. It is necessary to enrich your diet with vitamin-mineral complexes, well-digestible proteins (meat, fish, cottage cheese, eggs), offal, vegetables, fruits, berries, and a moderate amount of boiled cereals (rice, buckwheat).
You should not eat more often than 4 times a day and drink tea with milk 20 minutes before or after feeding. It is enough to drink a few sips of water before feeding the baby, and quench your thirst if necessary, but not with sugary drinks. Carbonated drinks, especially cola-type drinks, are prohibited.
It is important that the baby stays with the mother frequently, caresses, plays with the baby, and kind words from the first days of birth. But the baby should sleep in his crib or in a stroller in the fresh air (as often as possible).
It is necessary to put the baby to the breast regularly, even in the absence of breastfeeding. In this case, the baby must hold the nipple in his mouth for at least ten minutes, after which he can be offered a bottle.
The air temperature in the room should be from 18 to 20 degrees during wakefulness (this temperature stimulates physical activity), from 20 to 22 degrees during sleep. At an ambient temperature of about 32 degrees Celsius, the baby’s physical activity is practically zero, which is harmful, not a concern.
Often immature babies are prescribed therapeutic massage. But only a specialist should do it. Mothers must master the rules of stroking and light massage for newborns.
The basis of the physiological maturity of the baby is the correct course of pregnancy
For the harmonious development of the baby and the timely maturation of all its systems, maximum attention should be paid to the stages of preparation for pregnancy and the first weeks of pregnancy. This is the time when fetal exposure to drugs, alcohol, nicotine and other substances is especially dangerous. This is the time when any nervous stress of the mother is reflected in the processes occurring with the baby. Hunger in the mother, even hidden hunger in the form of a deep deficiency of the most important nutritional factors (amino acids, B vitamins, iron, oxygen, iodine, omega-3 polyunsaturated fatty acids, etc.) can also be the cause of the physiological immaturity of the baby.
Tune in to a positive pregnancy. Make sure that there is no teratogenic effect in every tablet you are going to swallow, in every food you eat or glass of liquid you drink, in every cream, toothpaste, procedure, and detergent.
Pregnancy lasts only nine months. Therefore, a “sacrifice” in the form of refusing a glass of wine, a cosmetic procedure or a long flight is nothing compared to a healthy baby, ready for life in a new world.