Sweating (hyperhidrosis) is a natural physiological process characteristic of all warm-blooded living organisms. It performs a number of vital functions: regulates heat exchange and maintains optimal water-salt balance. But heavy sweating is a symptom of one of the dangerous diseases.
How and why sweat occurs
The content of the article
When overheated, sweat glands begin to release fluid to the surface of the skin, thereby reducing body temperature. Water-salt balance is needed to maintain a constant level of electrolytes and ions in the intracellular fluid. Blood plasma also has a salt composition, but in a slightly different concentration.
The main regulator of sweating is the hypothalamus, a region of the brain that sends signals to various parts of the endocrine system, in particular the sweat glands.
Thus, with an increase in the concentration of salts in the blood plasma and a decrease in the volume of intercellular fluid (workout, visiting a sauna, staying in the sun), the signal is processed by the hypothalamus, which reacts by creating a feeling of thirst.
When body temperature rises, regardless of whether it is external influence (overheating) or internal processes (fever), thermoreceptors reflexively react to this and signal the hypothalamus. It activates the work of more than 2.5 million sweat glands, and they begin to secrete sweat-fat secretion.
Problem with hypertension
The manifestation of excessive sweating is medically called hyperhidrosis. Sweating can be a sign of the influence of external unfavorable factors, or it can be a symptom of some disease. If you sweat even in a calm state, the sweat becomes sticky or changes color and smell, then the problem needs to be given more attention.
With hyperhidrosis, individual parts of the body can sweat, then they talk about a local form, or the whole body can sweat - a generalized subtype. Pressure sweating often comes with other symptoms.
A disease such as hypertension is characterized by high blood pressure and excessive sweating. The usual readings are 120/80 mmHg. When these indicators increase, a person begins to feel unwell. There is a large list of factors when the measurement readings on the tonometer are increased:
- unhealthy diet with a predominance of spicy and salty foods;
- hormonal imbalance;
- age-related changes;
- thyroid diseases;
- excess body weight;
- diabetes;
- consumption of nicotine, alcohol;
- lack of physical activity.
With high blood pressure, the condition is initially accompanied by weakness, drowsiness, headache, dizziness, decreased concentration and memory, and numbness of the limbs. Then other symptoms appear in the form of increased sweating, tinnitus, redness and swelling of the face.
When pressure increases, excessive stimulation of the cerebral cortex begins, which causes disruptions in the autonomic part of the nervous system. The sweat glands begin to actively function and produce sweat at an increased rate.
High blood pressure and the manifestation of hyperhidrosis are accompanied by the release of adrenaline into the bloodstream. There is a rise in blood sugar and blood pressure.
What will help against high blood pressure? During treatment, all actions should be aimed at stabilizing blood pressure. In the initial stages, it is enough to change your diet and lifestyle, eliminate nicotine and alcohol, and constantly monitor your blood pressure. If these measures are not enough for high blood pressure , one drug is prescribed. If the blood pressure does not return to normal within several weeks, several medications are prescribed.
What kind of sweating is considered normal: norms, smell
Normally, even at rest, women secrete about 500 ml. sweat, in men - 700-1000 ml. During illness, when body temperature rises, about 3000 ml of sweat is produced per day. Such losses must be compensated, otherwise unpleasant consequences will arise - dehydration.
In addition to reactions to temperature, sweating is psychogenic in nature. Thus, apocrine glands located in the armpits, groin, and genital area are activated at the moment of emotional arousal, when an object of the opposite sex appears, during a quarrel or an increase in the emotional and mental background
The composition of the sweat from these glands is more concentrated, it contains enzymes that have a strong odor. However, it does not cause rejection, but carries genetic information. These are so-called pheromones, which help to choose a person who is suitable from a genetic point of view.
The unpleasant odor of sweat is due to the fact that the sweat of the subcutaneous sweat glands, eccrine glands, can destroy the keratin that covers the top layer of the skin. Microorganisms living on the epidermis begin to feed on softened keratin and multiply, releasing decay products. This is what causes the unpleasant odor.
It is especially active in the area of apocrine glands, so it is important to maintain hygiene standards. Usually, taking a shower or using wet wipes solves the problem of excessive sweating, but in some cases, hyperhidrosis becomes pathological and indicates serious problems in the body.
What does increased sweating indicate?
Hyperhidrosis is not always a pathology. Sweating affects obese and overweight people, women in the premenopausal period, and teenagers. There is nothing abnormal about this. Men sweat 2 times more intensely than women, people with African roots have a genetic predisposition to hyperhidrosis, and in summer the intensity of sweating increases regardless of gender and age.
Professional athletes who train 5-6 hours a day, even after taking a shower and completely changing clothes, continue to sweat intensely for some time after physical activity, and this is not a deviation from the norm.
Some people don’t see anything wrong with sweating; it doesn’t irritate them, although those around them suffer from it.
We should talk about pathology when the problem not only interferes with the person who has it, but also affects social connections. Sweat has a rather complex composition, which includes lactic and uric acids, ammonia, and various salts. As a result of exposure to the epidermis, bacteria are activated, which feed on softened keratin particles. This is precisely the reason for the specific vinegar smell of sweat.
In principle, it is enough for a healthy person to regularly change his underwear and take a shower daily so that the unpleasant smell of sweat is not heard. Apocrine glands secrete a substance with an individual odor depending on health, age and fertility.
In unhealthy people, it becomes intense and repulsive to others. Moreover, standard preventive measures (changing underwear, using antiperspirants, showering twice a day) do not bring any results.
Sweating for no apparent reason indicates pathological processes in the body, among which there are life-threatening pathologies. In particular, hyperhidrosis is characteristic of impaired hemostasis - the optimal level of hormones. This happens when there is a malfunction of the hypothalamus, a small area of the brain that controls the endocrine system.
The most famous example of disturbances in the functioning of the hypothalamus is menopause - the attenuation of a woman’s reproductive functions. During this period, the hypothalamus sends incorrect signals, the endocrine systems experience disruption and react with involuntary activation of the sweat glands - the so-called hot flashes.
In addition to menopause, hyperhidrosis occurs in case of other disorders.
Deviations from the norm and causes of pathology
In addition to an increase in the amount of sweat even at rest, hyperhidrosis is accompanied by the following symptoms, which can appear individually or in combination:
- pungent odor of sweat (bromidrosis) even with proper hygiene;
- ineffectiveness of hygiene products: deodorants, antiperspirants;
- staining of sweat (chromidrosis) due to intoxication of the body or taking certain medications;
- abrasions and redness in areas of increased sweating.
Hyperhidrosis is divided into primary and secondary, they are caused by different reasons. Primary – characteristic of adolescence and appears during puberty in less than 1% of people.
Secondary hyperhidrosis is a consequence of endocrine, somatic, tumor and other pathologies. It can also accompany normal physiological conditions - menopause, pregnancy.
Each of these types of hyperhidrosis is divided according to its location. Primary is divided into:
- palmar (palmar);
- axillary (axillary);
- foot (plantar);
- hyperhidrosis of the face and scalp (craniofacial);
- perineal (perineal).
Secondary:
- general;
- regional – appears due to damage to peripheral nerves, cerebrovascular disorders;
- focal – Frey's syndrome, eccrine nevi.
Currently, there is no consensus on why primary hyperhidrosis occurs. It is generally accepted that it is based on increased activity of the central division of the sympathetic nervous system.
The main common causes of secondary hyperhidrosis:
- endocrine – diabetes mellitus, increased levels of thyroid hormones;
- lipid metabolism disorder - obesity;
- hormonally active tumors;
- inflammatory and infectious diseases - often tuberculosis, endocarditis;
- psychosomatic pathologies.
In women and men, in addition to the general ones, there are specific causes of heavy sweating. In women, hyperhidrosis is often caused by an increase in the level of sex hormones: estrogen, estradiol, progesterone, prolactin during menstruation, pregnancy, when taking contraceptives, as well as changes in hormonal levels during menopause and the postpartum period.
The cause of increased sweating throughout the body in men is often the level of testosterone. After 40-50 years, the level of this hormone in the body decreases, which disrupts autonomic regulation, as a result of which sweat production increases. Increased sweating can also be caused by nicotine addiction.
Nocturnal hyperhidrosis is classified as a separate category, which is diagnosed in both women and men. There are several reasons for heavy sweating during sleep:
- Sleep apnea syndrome . Mostly typical for men, especially those suffering from constant snoring. 1-2 hours after falling asleep, during deep sleep, heavy sweating begins, and a short-term breath holding suddenly occurs (for a few seconds). After breathing is restored, profuse sweating also occurs.
- Withdrawal syndrome . It is typical for both men and women suffering from alcoholism. With a sudden cessation of alcohol intake, dysfunction of all body systems, malfunctions of various organs, and severe intoxication occur. This condition is characterized by attacks of profuse sweating - very profuse, even to the point of wet underwear and bed linen. Sweat has an unpleasant odor. A similar situation is observed with drug addiction.
- Tuberculosis is often the cause of excessive sweating at night, while with other diseases sweating can increase at any time of the day.
Increased sweating in thyroid diseases
Sweating is characteristic of hyperthyroidism, characterized by an increase in the production of thyroid hormones and the development of intoxication.
In addition to increased, causeless sweating, symptoms of hyperthyroidism include:
- sudden weight loss
- drowsiness
- swelling in the neck area
- tachycardia
- irritability and nervousness
- diabetes. Under the influence of sugar in the blood, blood vessels and nerve connections are destroyed, but not throughout the body, but only in certain areas. The scalp, arms, neck and chest sweat especially heavily in diabetes.
Sweating is also characteristic of hypoglycemia - a lack of glucose in the blood. This is caused by an increase in adrenaline levels, which is activated when there is a lack of sugar.
Pheochromocytoma - sweating due to adrenal tumors
Pheochromocytoma is a tumor of the adrenal gland that stimulates the production of catecholamines - adrenaline and norepinephrine. The disease is characterized by crises, during which panic attacks, tachycardia, nausea, gag reflex, and increased sweating are observed.
The attack is impossible not to notice, because it is accompanied by impaired cerebral circulation, trembling in the body and pulmonary edema. It lasts 2-3 minutes, but is extremely stressful for a person.
In the absence of an adrenal tumor, an increase in catecholamines is caused by heart disease, alcohol withdrawal, and refusal to take certain medications.
Ovarian dysfunction
The pathology occurs in every 10th woman of reproductive age. This may be an ovarian cyst, but polycystic disease often occurs - a complex disease in which ovulation does not occur and the follicle begins to grow. Over time, the ovary becomes like a bunch of grapes due to the many cysts that form.
Hormonal imbalance and lack of female sex hormones lead to increased production of testosterone, the male sex hormone. It increases metabolism, causing increased sweating.
It is also promoted by autonomic disorders, accompanied by irritability, aggressiveness, and sleep disorders. Symptoms of ovarian dysfunction, in addition to sweating, are menstrual irregularities, weight changes, deterioration in health, increased hair growth, etc.
Sweating and central nervous system diseases
The autonomic nervous system is controlled by centers in the medulla oblongata and spinal cord, and the center is located in the hypothalamus. Ganglia, sympathetic nerve ganglia, are located near the spine, and nerve impulses emanating from them travel along nerve fibers to various parts of the body. If there is a disturbance in the functioning of the central nervous system, increased sweating occurs, regardless of the cause of the malfunction.
But this is only a secondary sign, indicating more significant symptoms:
- with Parkinson's disease,
a person's hands and head shake, muscles have increased tone, and their gait changes; - a stroke
is characterized by speech impairment, changes in facial expressions, and severe headache; - with epilepsy,
a person experiences convulsive seizures, during which hyperhidrosis occurs due to severe overexertion; - with a concussion,
loss of consciousness, nausea, and perspiration may appear on the forehead; - injury to the hypothalamus
manifests itself not only by increased sweating, but also by pressure surges, vascular problems, and sleep disturbances; - hormonal changes.
Teenagers tend to sweat a lot. This is due to a sharp hormonal surge, as well as intensive development of the whole organism and an increase in the functioning of most glands. There is nothing pathological about this, but sweating can cause discomfort for a teenager.
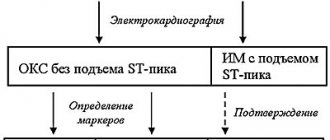
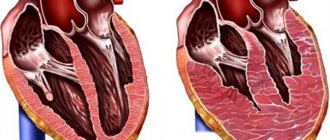
Heart disease and unpleasant symptom
Heart problems may be associated with rhythm disturbances. The normal rhythm is considered to be about 70 beats per minute. If the frequency of contractions is greater, then you need to look for the reason. Medications, exercise, and stress can cause heart palpitations. The symptom occurs with heart problems, hypotension or anemia. Cardiac pathology is recognized by one of the main signs - sweating.
With various heart diseases, low blood pressure (below 100/60 mm Hg on a tonometer) and high pulse are often observed. Characteristic signs include difficulty breathing and weakness. The heart rate becomes rapid, resulting in increased sweat production.
In heart failure, sweating begins from the forehead and gradually spreads throughout the body. The face turns pale, sweating limbs become cold. Blood pressure changes, it is often at a low level, the patient has difficulty breathing and feels nauseous, and is bothered by attacks of dizziness.
With low blood pressure, your heart rate may also decrease. In this case, the low blood pressure is accompanied by a lack of air, shortness of breath, and the patient feels dizzy and has a headache. Worried about weakness, fatigue.
Against the background of all these signs, severe sweating, nausea or even vomiting appears. Low blood pressure is usually hereditary. Children from an early age suffer from this disease. They look apathetic, inactive, and get tired quickly. Among adults, low blood pressure is observed in patients who are underweight and tall.
Other factors can provoke low blood pressure and increased sweating:
- prolonged mental and emotional stress;
- sedentary occupation, lack of sufficient physical activity;
- diseases of the nervous system;
- respiratory diseases;
- disorders of the thyroid gland.
Low blood pressure is life-threatening. A sudden loss of consciousness may occur, vision decreases, coordination of movements is impaired, and interruptions in the functioning of the heart appear.
Only specialists prescribe medications for low blood pressure. Adjusting your lifestyle and diet will help you cope with the problem. It is useful to follow the following recommendations that will help you increase your blood pressure and get rid of excessive sweat production:
- healthy sleep of at least 8 hours;
- after waking up, it is not recommended to immediately get out of bed;
- It is useful to take a contrast shower;
- balanced diet with plenty of fruits and vegetables;
- the presence of moderate physical exercise (10 minutes allotted for gymnastics in the morning is enough).
In the event of a sharp decrease in pressure due to heart failure, the patient is placed on a flat surface. The head should be slightly higher than the body. It is recommended to apply a gauze bandage soaked in cold water to the forehead area and massage the cervical region. This will increase blood flow to all parts of the brain.
For low blood pressure, medications are prescribed: Citramon, Ephedrine, Cordiamine. You can just drink hot tea or coffee.
Sweating during menopause and pregnancy
In women before menopause, the levels of progesterone and estrogen decrease and the amount of FSH increases. This is a rather long process; menopause does not occur in one day. Several years before the onset of hormonal changes, a woman feels changes at the physiological level: her body odor changes, she sweats more often, quickly gains weight and has difficulty losing it.
Gradually, the level of female sex hormones falls, and male sex hormones (androgens) are produced more than during the fertile period.
Sweating is not the biggest problem; it only indicates irreversible changes in the body. If a woman notices an unusual increase in sweating, she should contact an endocrinologist. The doctor will conduct all the necessary tests and prescribe hormone replacement therapy.
Also, increased sweating often occurs in pregnant women, especially in the 1st trimester. The reason is a sharp restructuring in the body caused by implantation of the embryo to the wall of the uterus. The hypothalamus actively stimulates the production of progesterone, while other hormones are produced in smaller volumes.
A characteristic feature is sweating of the feet, regardless of the intensity of physical activity or its absence. At the same time, in other parts of the body, dehydration and dry skin occurs, even to the point of peeling. This is not a pathology, and by the 2nd trimester, local hyperhidrosis appears much less pronounced.
Types of hyperhidrosis
Hyperhidrosis can be local (localized) or generalized (generalized). When localized, increased sweating manifests itself in certain areas of the body, most often the armpits, palms, knees and elbows, and soles. Sweating may increase in one of these areas or in all of them together. This type of hyperhidrosis is usually caused by increased excitability of the nervous system, in some cases by heredity.
General hyperhidrosis is characterized by excessive sweating over almost the entire surface of the body. It can be physiological, associated with changes in hormonal levels - in adolescence, pregnancy, menopause, and also be a symptom of infectious diseases, functional disorders or diseases of the endocrine and nervous system.
Cardiovascular disease and sweat
They are also characterized by hyperhidrosis caused by activation of the central nervous system. Other symptoms, depending on the disease, include the following:
- for hypertension: increased blood pressure, increased heart rate, tinnitus, headaches, numbness of the hands;
- with coronary heart disease: pain behind the sternum (angina pectoris), inability to take a full breath, nausea and very profuse sweating;
- during myocardial infarction, perspiration covers the entire body, a feeling of fear arises, blood pressure drops, and the person feels very severe pain in the heart area;
- hyperhidrosis with thrombophlebitis occurs in advanced forms of blockage of the vein lumen;
- tachycardia occurs as a reaction to stress or fear, while a person’s adrenaline level increases, the body becomes covered in perspiration, and it becomes difficult to breathe. With tachycardia, there is heat in the head, but the hands remain cold;
- with vegetative-vascular dystonia, sweating is a reaction to stress, even the slightest one.
But with this pathology, the body mobilizes regardless of the reality of the situation. Often a person suffering from VSD experiences bouts of sweating and panic attacks completely unexpectedly: in the subway, in a crowd or in a quiet environment. In this case, hyperhidrosis is a side reaction to imaginary or real stress.
Sweating due to infection
The vital activity of viruses and bacteria is accompanied by the production of pyrogens that affect the thermal sensitivity of neurons. During the period of exacerbation of an infectious disease, body temperature always rises significantly, which is why hyperhidrosis occurs. The virus is accompanied by muscle pain and body aches, the bacterial infection is accompanied by a skin rash and general toxicity.
Rheumatism is also infectious in nature. The patient's body temperature is constantly elevated, which causes severe sweating. Damage to joints and connective tissue prevents normal movement, but people sweat as if after intense training.
Syphilis is a sexually transmitted disease that affects the mucous membranes. It is characterized by damage to the nerve roots located along the spine, which is expressed by a local increase in sweating.
Sweating is often the first symptom of a serious illness. In medicine, it is known under the term “hyperhidrosis”, and is characterized by impaired function of the sweating system. Hormonal disorders, endocrine and infectious diseases are often accompanied by excessive sweating. It is necessary to consult a doctor and find out what disease was the source of excessive sweating.
What types of hyperhidrosis are there?
With hyperhidrosis, different localization of the pathological process is noted. Taking this criterion into account, 2 types of sweating are distinguished:
- Generalized. Profuse sweat appears on all parts of the body; the patient experiences increased sweating of the face, neck and head. Generalized hyperhidrosis is characteristic of various diseases; it is never an independent disorder.
- Local. With this type of hyperhidrosis, the legs, arms, palms, feet and other individual parts of the body sweat. Local hyperhidrosis often occurs as an independent disease.
Diseases that cause sweating and additional symptoms
If sweating is observed in various diseases, doctors talk about secondary hyperhidrosis. To eliminate it, it is necessary to directly influence the underlying disease. Sweating occurs against the background of infectious infections, tuberculosis, and endocrine pathologies. Also, increased sweating may occur due to drug therapy, in which case a change in drug is required.
Endocrine diseases that cause severe sweating
Most often, severe sweating is caused by impaired function of the endocrine system. Diabetes mellitus is the most common source of sweating during the day and night. In type 1 and type 2 diabetes, it manifests itself in 3 forms, presented in the table:
| Form of sweating in diabetes | Features of manifestation |
| Unfounded | Sweating is not associated with any pathological manifestations |
| Not accompanied by high temperature or fever | |
| Flavoring | Appears after consuming a product |
| Only sweating of the face and neck is observed | |
| Night | Caused by a decrease in insulin levels at night |
Other diseases of the endocrine system can also affect excessive sweating:
- Acromegaly. The disease is characterized by the formation of a benign formation in the pituitary gland region of the brain. A person with acromegaly, in addition to increased sweat production, will experience signs of disproportionate growth of muscles and bones.
- Menopause period. In women, menopause often occurs with increased sweating. More than half of menopausal women suffer from this symptom. The problem is caused by abnormal levels of estrogen in the body.
- Thyrotoxicosis. With this disease, there is increased production of thyroid hormones. Additional symptoms appear more clearly in the later stages of the disease.
Infectious diseases are the main source of sweating
This symptom often indicates that an infection has entered the human body. Increased sweat production is caused by the following infectious diseases:
- Tuberculosis. In addition to increased sweating, the patient will be bothered by a cough with expectoration of blood, high fever, and soreness in the sternum. Particularly increased sweating occurs at night during sleep.
- ARVI. Acute respiratory viral infections accompanied by fever often cause the patient to sweat excessively.
- Inflammation of the bronchi. With bronchitis, a person constantly has a high temperature, which becomes a source of increased sweating.
- Malarial infection. When the disease occurs, symptoms such as fever, cold sweat, and chilly feeling appear.
- Purulent processes, including syphilis. With the latter, nerve fibers are damaged, which provokes impaired function of the sweating system.
Increased sweating is the first sign of a tumor
Sometimes excessive sweating is the first sign of a malignant or benign tumor in the body.
Acute intoxication of the body
If severe poisoning by chemicals or toxic substances is detected, the patient will be bothered by the following symptoms:
- swelling;
- high blood pressure;
- increased heartbeat;
- excessive sweating.
This condition is observed in patients with excessive consumption of caffeine, abuse of cocaine, alcohol and certain medications. When taking certain medications, the sympathetic nervous system is stimulated, resulting in increased sweating. A patient with excessive sweating due to intoxication requires emergency care.
Physician-therapist Boyko E.A.
Malignant and benign tumors
The center of thermoregulation is the hypothalamus, and tumors of any nature in this area cause hyperhidrosis. Sweating especially increases at night, regardless of the temperature in the room.
If this happens without explanation, then the following diseases can be assumed:
- histiocytic lymphoma (malignant lesion of lymphoid tissues);
- lymphocytic lymphoma (oncological damage to the lymph nodes);
- mixed lymphoma (complex cancer of the lymph nodes);
- Burkitt's lymphoma (malignant tumor of the jaw).
Oncological neoplasms are accompanied not only by hyperhidrosis, but also by sudden weight loss, sleep disturbances, general weakness and fatigue.
Preventive measures
To prevent hyperhidrosis, it is first necessary to exclude the development of somatic diseases and promptly treat chronic pathologies. To do this, you need to regularly visit a doctor for medical examination or prescribe treatment.
If excessive sweating is not a consequence of other diseases, you should adhere to the following measures:
- exclude spicy, hot dishes, spices, alcohol from the menu;
- stop smoking;
- take a contrast shower, warm baths with herbal decoctions (chamomile, oak bark);
- do not take medications without a doctor’s prescription;
- in clothing, give preference to natural fabrics (cotton, linen);
- shoes should be made of genuine leather or breathable materials with special moisture-absorbing insoles.
Article sources:
- Hyperhidrosis: method of correction. Batyrshina S.V., Khaertdinova L.A. Practical medicine No. 8, 2014. p. 16-23
- Hyperhidrosis and its impact on those living with it. Mary Lenefsky, 1Department of Dermatology, Emory University School of Medicine, Atlanta, GA, 2021.
- Pathophysiology and Treatment of Hyperhidrosis. Tomoko Fujimoto. 1Department of Dermatology, Graduate School of Medical and Dental Sciences, Tokyo Medical and Dental University, Tokyo, Japan. 2016
- Axillary hyperhidrosis: a focused review. Jason E Sammons, Amor Khachemoune. Department of Clinical Medicine, Avalon University School of Medicine, Willemstad, CW, USA. 2b SUNY Downstate and VA Medical Center, Brooklyn, NY, USA. 2017
What research is being done to identify the true causes of hyperhidrosis?
Excessive sweating is a subjective concept. Not everyone is alarmed by hyperhidrosis, so we need to talk about pathology if increased sweating is not typical for a person, causes him severe discomfort and causes anxiety.
The initial examination is carried out by an endocrinologist or therapist, because in most cases the cause of excessive sweating is a disruption in the functioning of the endocrine system. The specialist gives a referral for standard tests showing the general condition of the patient’s body.
These include:
- general blood analysis;
- general urine analysis;
- blood chemistry;
- analysis of thyroid hormones (T3, T4, TSH);
- ECG.
Depending on the test results, the patient undergoes additional examinations.
Description of tests and ultrasounds prescribed for excessive sweating
| Preliminary diagnosis | Research | What is the essence of the study? |
| Suspicion of cancer | Analysis for tumor markers | Analysis for tumor markers Tumor markers are specific proteins, the concentration of which increases in the body only during oncological processes. In healthy people, tumor markers are contained in minimal quantities. The main tumor markers are: PSA is a protein that concentrates in a man’s blood during the development of prostate cancer. An increase in protein also occurs with adenoma (benign tumor) of the prostate gland. HCG is present in the body of both women and men. It increases significantly during pregnancy, so it is additionally taken along with a blood test for alpha-fetoprotein (AFP). When the concentration of both proteins increases, a preliminary diagnosis of testicular cancer is made, and in women with ovarian cancer, the AFP level increases significantly. Also, an increase in hCG is observed in cancer of the stomach, uterus, intestines, liver, as well as uterine fibroids. AFP - increases in oncological processes, especially in the liver, as well as in cirrhosis, hepatitis and renal failure. In a pregnant woman, it indicates fetal pathology. Ca-125 is a tumor marker that helps identify cancer of the uterus, breast, stomach, liver, pancreas, etc. It also increases with endometriosis, ovarian cysts, and peritonitis. |
| Suspicion of a pituitary tumor | MRI and angiography Analysis for prolactin X-ray with an eye to the sella turcica Analysis of cerebrospinal fluid (CSF) | For pituitary tumors, a combined MRI and angiography technique is used - studying cerebral circulation. The technique allows you to detect tumors as small as 5 mm. Prolactin is a pituitary hormone that is responsible for milk production in women, but is also present in men. It increases with uterine fibroids, pregnancy, ovarian tumors, and pituitary tumors. Breast discharge in men is associated with an increase in prolactin, which reduces the concentration of male sex hormones and increases the levels of estrogen and progesterone. A pituitary adenoma is indicated by a prolactin concentration in the blood of more than 250 ng/l. The sella turcica is a bone formation in the bed of which the pituitary gland is located. When the walls of the sella turcica are deformed, one can judge the growth of a pituitary tumor. The only drawback is that bone deformation occurs only when the tumor is large. When identifying pituitary tumors, myelin basic protein (MBP) is of great importance. In a healthy person, its value does not exceed 4 mg/l. Also, with neoplasms, epithelial cells are detected in the cerebrospinal fluid, which should not normally be present. The analysis does not yet confirm pituitary adenoma, but is an indication for a more in-depth study. |
| Suspicion of diabetes mellitus | Blood and cerebrospinal fluid test for glucose | A feature of hyperhidrosis in diabetes mellitus is excessive sweating in the armpits, palms, neck, but dry skin of the legs and feet. A blood test will quickly indicate an increase in blood sugar. with an increased glucose content in the cerebrospinal fluid, we can talk about viral lesions of the brain (meningitis). |
| Menopausal syndrome | Sex hormone analysis | “Hot flashes” shortly before the onset of menopause are associated with a decrease in the level of female sex hormones and an increase in androgens. Determining the ratio of estrogen, progesterone, LH and FSH shows a complete picture of hormonal levels. |
| Suspicion of tuberculosis | PCR diagnostics | Polymerase chain reaction helps identify Koch's bacillus within 4 hours. Unlike Mantoux, PCR detects even one bacilli of the pathogen at the earliest stage of the disease. The analysis will also help to select an effective drug and identify resistance to certain drugs. |
| Suspicion of infection | Linked immunosorbent assay | ELISA allows you to see the connection between the body’s immune cell and the cell of the infectious agent. Depending on the type of immunoglobulin (IgE, IgD, IgG, IgM, IgA), the type of pathogen is identified. The analysis identifies more than 600 infectious agents and viruses. |
| Suspicion of heart disease | Laboratory blood test | ESR increases with endocarditis, rheumatic heart disease. In chronic heart failure, the level of protein, as well as potassium and sodium in the blood serum increases. High cholesterol indicates atherosclerotic vascular disease. An increase in white blood cells indicates inflammation. A large number of platelets is observed with venous thrombosis. Enzymes ALT and AST increase during myocardial infarction. An increase in electrolytes occurs when the heart rhythm is abnormal. C-reactive protein is concentrated during myocardial infarction. |
| Suspicion of pheochromocytoma | Ultrasound of the abdominal organs | Pheochromocytoma is a tumor of the adrenal glands that leads to hormonal imbalance. The tumor is visualized on ultrasound as an oval or round formation of increased echogenicity. |
| Suspicion of acromegaly | Analysis for somatotropin | Somatotropic hormone (GH) affects not only growth, but also overall metabolism. A high concentration of the hormone indicates a tumor of the pituitary gland, stomach or lungs, anorexia nervosa, cirrhosis of the liver, and renal failure. Sometimes an illiterate diet leads to an increase in growth hormone, leading to depletion of the body. Low levels of growth hormone indicate pituitary insufficiency caused by infectious lesions of the brain, autoimmune pathologies, vascular disorders and postpartum blood loss. |
Sweating and hypotension
Excessive sweating, which does not go away even in the cold months, from which no clothing can save you, is a very unpleasant condition that is familiar to millions of people.
Cardiologist of the highest category Ivan Sergeevich Gruzdev, Ph.D.
Excessive sweating, which does not go away even in the cold months, from which no clothing can save you, is a very unpleasant condition that is familiar to millions of people. It is especially painful for a person of working age, who, having gotten “wet through” already in public transport on the way to work, must then either spend the whole day in sticky and wet underwear, or look for somewhere a secluded place to change clothes and wear them every day. bring a change of clothes with you.
To solve this problem, a person suffering from excessive sweating (or hyperhidrosis) sooner or later consults a doctor. He learns from the doctor that excessive sweating is most often not an independent disease, but a signal of arterial hypotension, that is, low blood pressure (less than 100/60 mm Hg blood pressure). You can detect this disorder in yourself by the following signs: reduced psychophysiological energy, such as weather dependence, lethargy, difficulty getting up in the morning, emotional instability, apathy, absent-mindedness, deterioration of memory and performance.
Hypotension can be either a normal state of the body or a disease, and a very common one. Most often it occurs in women 20-40 years old. Each person can figure out, without the help of a doctor, what kind of hypotension he has - “healthy” or “sick”. “Healthy” hypotension has clear signs. Firstly, it is clearly detected already in the first phase of human puberty (from birth to 10 years of age) and never begins at a young or mature age, like hypotension-disease. Secondly, for a normal hypotensive person, all the manifestations of decreased energy that I talked about are morning “animals” that are not difficult to cope with. True, with the exception of increased sweating, which can remain throughout the day. In short, although the quality of life decreases, it is only insignificant. For approximately 10-15% of people, hypotension is normal. In other words, out of 6.7 billion earthlings, there are more than 700 million hypotensive people!
As for hypotensive patients, these “animals” do not retreat from them either day or night. And, in addition to the fact that all of the above “energy failures” manifest themselves much more strongly, they are accompanied by complications unfamiliar to “healthy” hypotensive patients: nausea, dizziness, coldness and numbness of the extremities, anxiety and depression, and most importantly - hypotensive crises with heavy cold sweat (also and constant sweating worries such patients) with fainting, thread-like pulse.
My patients often ask me, “if I am a “healthy” hypotensive person, will I have to put up with a slight deterioration in my health at the beginning of the day and continued sweating?” In fact, it is possible to cope with both. We must avoid lack of sleep, and in the morning you should not get up quickly or abruptly. Do some physical exercise while still in bed. At least five minutes of gymnastics and a contrast shower are useful. Breakfast for a hypotensive person should include, in addition to a cup of invigorating coffee, some spicy dish to increase appetite. And definitely something salty. Natural restorative drugs also help “healthy hypotensive people” to normalize blood pressure in order to get rid of excessive sweating, which I will talk about a little later.
But if hypotension, a disease, has begun, it is urgent to figure out what kind of painful hypotension the patient is experiencing. Until recently, it was believed that more than 90% of cases of such ailments are so-called neurocirculatory hypotension, where the functioning of nerve cells in the vasomotor nuclei of the brain is disrupted. And doctors habitually stamped out a similar diagnosis for any hypotension, without even trying to understand its causes. Today it has been proven that about 30-40% of painful hypotension are the consequences of hidden bleeding. Another 10% are caused by damage to the endocrine glands and other organs, but not the brain. True neurocirculatory hypotension occurs in approximately 50-55% of cases.
But how can we find out what caused the hypotension-disease? You need to start with a detailed blood test. If the number of red blood cells is reduced, the level of iron in the blood has dropped, then the cause is hidden bleeding. In men, it most often begins due to stomach or duodenal ulcers, and in women - due to gynecological diseases. Then you need to immediately clarify the cause of blood loss and fight it. If there are not enough hormones of the thyroid gland, adrenal glands, pituitary gland, then the root cause of hypotension is the deterioration of the functioning of these glands. But if there is no blood loss, the endocrine and other organs whose work is assessed by a blood test are not affected, then neurocirculatory hypotension remains suspected. Official medicine has not yet developed a single reliable medicine against it.
Then the last hope remains - natural stimulants, which are drugs with a general strengthening effect. There is hardly any ailment where the healing power of natural remedies, which have been selected by traditional medicine over the centuries, would be as noticeable as with neurocirculatory hypotension! I will only list the remedies that I prescribe to my patients. Royal jelly, the drug Apilak, normalizes blood pressure well and relieves excessive sweating. Its beneficial properties were known back in medieval England and were also used for problems with thermoregulation (cold hands and feet). This was considered a great disadvantage for women. Tincture of ginseng root also has a direct vasoconstrictive effect. However, treatment with ginseng, as well as with two other “stimulant plants”, aralia and eleutherococcus, is contraindicated for sclerosis of the coronary and cerebral arteries, and especially for internal bleeding, while at the same time there are practically no contraindications for royal jelly.
Hypotensive patients should take all natural stimulants only in the first half of the day. At night, calming plants are useful, since full sleep is the best medicine for hypotension. I recommend to my patients an infusion of valerian and lemon balm tea before dinner.