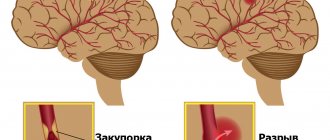
Stroke is a complex disease that disrupts the normal functioning of the brain. Develops against the background of diabetes mellitus, coronary heart disease, atherosclerosis, hypertension, aneurysms. A stroke disrupts brain function and entails changes in the functional characteristics of a number of organs, impaired mobility, and sensitivity.
Stroke ranks first among the causes of disability in middle-aged and elderly people. Moreover, 30% of cases occur in people of working age – up to 65 years.
In case of a stroke, proper first aid plays a significant role. In the process of rehabilitation - competent treatment and care for patients after a stroke. Even after the most severe form of an attack, the victim can regain partial mobility.
Caring for patients after a stroke: what is worth knowing?
While a person who has suffered a stroke is in hospital, he is looked after by qualified medical personnel. But sooner or later the patient is discharged, and then his relatives have to look after him. To help your loved one recover and to maintain the strength to perform the necessary procedures, it is worth learning the basics of correct and high-quality general nursing care.
From a medical point of view, there are two types of paralysis: right-sided and left-sided. The behavior of patients with different types of paralysis differs significantly. This is worth considering when developing an exit strategy. With right-sided paralysis, damage to the left side of the body, the patient’s motor function on the left side of the body is impaired. As a result, he:
- does not feel the left lower and upper limbs;
- does not understand where they are located;
- does not perceive the surrounding space (while walking he bumps into doors, cannot calculate the distance to the nearest object);
- loses place of reading.
Tips that will make life easier for such a patient:
- the bed must be placed so that the patient can see with his right eye the center of the room and whoever enters the room;
- Place household items on the side of your right hand;
- encourage your ward to talk more, as speech helps to quickly restore spatial perception.
With left-sided paralysis, damage to the right side of the body, the patient’s emotional background is disturbed. He is in a lethargic depressed state and does not experience any emotional experiences. Patients with left-sided stroke:
- have problems with speech, it is difficult for them to pronounce words and form sentences;
- have difficulties with perception, do not understand what is being said to them;
- they forget words and names of objects.
Tips on how to make the life of such a patient more comfortable:
- at first, replace words with gestures, facial expressions, and gentle touches;
- speak slowly, clearly, avoid complex sentences;
- try using written language instead of spoken language;
- perform smooth, unhurried movements;
- ask the doctor to develop a speech therapy complex, help the patient perform the developed speech therapy exercises.
Dietary recommendations
The patient should receive food of sufficient calorie content - 30-35 kcal/kg body weight/day. At the same time, patients with acute diseases, including those accompanied by fever, require a higher energy value of food. Obese patients, on the other hand, require fewer calories per unit of body weight.
It is necessary to ensure a sufficient amount of protein from food. A patient at risk of developing bedsores should receive 1.25-1.5 g/kg body weight per day.
In some cases, it is possible to achieve such an amount of protein only by using special protein-rich mixtures for enteral nutrition.
If the amount of food a patient can take is limited, but there are signs of protein deficiency, it is better to use formulas for feeding cancer patients, since they contain more protein. Examples of such mixtures are Fortiker (NUTRICIA) and Enshur (Abbot).
Preventing swelling of the arms/legs
Poor circulation causes the formation of edema in the upper and/or lower extremities. Factors indicating the appearance of edema are cold, red extremities. Tips on how to prevent the problem:
- Sore limbs should be in a comfortable position. It is important to ensure that they do not hang down.
- Frequently changing the positions of the limbs helps avoid blood stagnation.
- In a sitting position, you can place a soft pillow/cushion under your arm and a strong support (small stool, hard cushion) under your leg. You can place a pad under your calves to improve support.
- In a sitting position, you must ensure that your back fits snugly against the back of the chair or other support.
Prevention of thrombosis
Almost every stroke patient leads a sedentary lifestyle. This causes the development of physical inactivity—a weakening of muscle tone. As a result, blood clots begin to form in the lower extremities. This process is dangerous due to the occurrence of thrombosis. You can prevent a dangerous condition:
- performing preventive exercises;
- using compression stockings, elastic bandage;
- taking medications to thin the blood (prescribed by your doctor).
Prevention of pneumonia
Prolonged bed rest causes stagnation of blood in the lungs. Against the background of this problem, pneumonia occurs. The danger of the phenomenon is its asymptomatic occurrence. Over time, the bedridden patient experiences weakness, cough, shortness of breath or heart failure, and fever. Pneumonia can occur at an early stage of a stroke (2nd - 3rd day of the disease) or a late stage (2nd - 6th week of the disease). To prevent the occurrence of pneumonia you must:
- perform a drainage massage - lightly tap the back at the level of the lungs (do not touch the spine);
- ventilate, moisten the room - dry air dries out the nasal mucosa, which becomes a breeding ground for infection;
- do passive gymnastics - several times a day the patient should be raised in bed, raise and lower the upper limbs, thus improving breathing;
- perform breathing exercises;
- give expectorants (as prescribed by a doctor).
Depression
Depression is very common in stroke patients, and a patient is more likely to be depressed than not. Sometimes depression arises from the experience of loss of some functions. Moreover, if the patient becomes dependent on others, the likelihood of depression increases. Depression can also be caused by disturbances in brain biochemistry due to a stroke, even if there are no significant neurological deficits. Therefore, the very fact of a stroke, even with minor disturbances, can lead to the development of depression due to disturbances in brain biochemistry.
Early detection of signs of depression is necessary to allow the condition to be effectively treated. Sadness that lasts more than two weeks or fear that does not go away may be signs of developing depression.
The same signs of incipient depression are hopelessness and desperation of one’s situation. Patients may also not comply with medical advice and express thoughts about the futility of life and a desire to die, which are already signs of serious depression. Fortunately, depression is very successfully treated with medication thanks to modern advances in pharmacology. In addition to antidepressants, communication with the patient and discussion of the consequences of the stroke that have affected the patient's life can be beneficial. The presence of depression is not a sign of weakness in the patient, but only an integral part of the consequences of a stroke, and this condition can be successfully treated.
Preventing constipation
People after a stroke often have problems with bowel movements. Drinking plenty of fluids, abdominal massage, medicinal and natural laxatives (beets, dried apricots, prunes, bran, bananas, and other foods) help combat constipation. Abdominal massage is performed with light circular movements. The intestinal area can be massaged with gentle pressing touches.
You can help improve the bowel movement process by developing a bowel movement routine: daily enemas/suppositories should be done until the natural process is restored. Developing a reflex to have a bowel movement at the same time helps avoid constipation.
You can improve natural intestinal motility with proper nutrition. The patient's diet should include vegetables and fruits, cereals, and dairy products. You should not eat spicy or fatty foods, baked goods, alcohol, or sugar. It is better to steam or bake food.
Preventing the formation of bedsores
Bedsores are formed under the influence of a number of factors:
- body overheating;
- unsuitable underwear and bed linen - injure the skin;
- illiterate care can provoke the appearance of long-term non-healing wounds;
- untimely treatment of abrasions, cuts, and other damage to the epidermis.
A bedsore is a source of infection entering the blood, which causes complications in the course of the disease. Bedsores appear in places where the skin is in constant contact with a hard surface. This is easy to avoid - you need to periodically change the position of your body. Do all manipulations of turning over and changing body position slowly and carefully. The client must be left in the selected position for 2 – 3 hours. Make sure that no folds form under the body and that the laundry does not bunch up.
Air baths are a good prevention of skin necrosis. Light massage of areas prone to bedsores (shoulder blades, hips, sacral area, heels, other areas) helps avoid damage to the epidermis. Before massage, it is best to lubricate the skin with camphor oil. The massage is done until the surface of the epidermis becomes slightly red, which indicates restoration of blood circulation.
Patient Assessment
Treatment of pressure ulcers begins with a complete assessment of the patient's general condition and the characteristics of the wounds. The development of pressure ulcers indicates the need to reconsider preventive measures.
A standardized approach should include initial assessment, appropriate treatment planning, and monitoring of wound healing.
Figure 2 Typical locations for pressure ulcers
The condition of the wound, dressing and surrounding skin, any possible complications and pain control should be assessed and recorded daily. The description should be supplemented by a rating on one of the scales developed for pressure ulcers.
Table 1 Stages of development of pressure ulcers (The National Pressure Ulcer Advisory Panel (NPUAP)
| Stage | Description |
| I | The skin is intact, the area of hyperemia does not disappear >1 minute after the pressure is removed. |
| II | Blisters or other skin lesions with partial damage to the dermis; Possible wound infection. |
| III | Full-thickness tissue damage. Subcutaneous fatty tissue can be seen in the wound; destruction extends to muscles; Possible wound infection. Detachment of the epidermis and the formation of fistulas are possible. |
| IV | Full-depth skin involvement, involvement of bones, tendons or joints; Possible wound infection. Often accompanied by detachment of the epidermis and the formation of fistulas. |
| The stage cannot be determined | Damage to the skin to its full depth, in which the base of the wound is made of necrotic masses and/or the surface is covered with a scab. |
| Deep tissue damage is expected | A bright red or maroon area surrounded by healthy skin or a blister filled with blood that has formed due to compression and/or displacement of the underlying tissue. |
Figure 3 Stages of development of pressure ulcers (The National Pressure Ulcer Advisory Panel (NPUAP)
Prevention of contractures
A side effect of a stroke is loss of mobility. Against the background of this functional disorder, contractures occur—limited mobility of the upper and lower extremities. Limitation of mobility leads to the fact that the patient cannot move, work with his arms and legs. This joint disease is easier to prevent than to treat later. Preventive measures:
- Correct body position - in bed, the patient should lie in a position close to normal physiological. To reduce muscle tone, you need to use rollers, pillows, and other means. Orthoses help keep your limbs in the correct position. To prevent your hand from clenching into a fist, it is convenient to use a massage ball, dumbbell, etc.
- Therapeutic gymnastics - exercises should affect all joints. Start gymnastics by warming up the muscles. For maximum effect, you can use a special gel. Therapeutic gymnastics lasts 20–30 minutes, includes 5–10 repetitions. A set of exercises must be practiced from the first days of the disease. This will avoid joint contracture and guarantee a better result.
Caring for a patient who has suffered a stroke requires great patience and perseverance from the caregiver.
Remember, high-quality home care, compliance with doctor’s orders, and emotional support are the conditions for the patient’s rapid recovery. In contact with
Help with rehabilitation
Caring for a person after a stroke at home is a set of rules that must be followed:
- Constant surveillance;
- Performing gymnastics and massage;
- Compliance with nutrition and diet;
- Drug treatment prescribed by a doctor;
- Consultation with a specialist about the relative’s condition.
To provide proper care to a person after a stroke, it is important to follow the rule of physical therapy and massage, which is performed every 3-4 hours. It is advisable that the nurse performing the massage has appropriate training.