How to protect yourself from heart attack and stroke
The development of one of the dangerous vascular pathologies - stroke or heart attack - is increasing every year. Men, hypertensive patients and those who suffer from endocrinopathies are especially at risk. People whose close relatives have suffered from cardiovascular diseases are also at increased risk.
Fortunately, the risks of both stroke and heart attack can be significantly reduced. To do this, you don’t need to perform any complex actions or completely change your usual schedule. We will talk about those measures to prevent stroke and heart attack that will minimize the risk of both vascular (vascular) disasters.
Risk factors for both diseases
Prevention of any pathology is based on the maximum elimination of risk factors. They are:
- Factors that cannot be influenced. These are age, gender (men under 50 get sick more often, then the numbers become equal), genetic predisposition to cardiovascular pathologies.
- Factors that can be modified: prevention of stroke and heart attack is aimed specifically at their elimination. This is smoking (including hookah or vaping), high cholesterol, hypertension, alcohol abuse, physical inactivity, consumption of trans fats and simple carbohydrates in large quantities, excess body weight (especially with an increase in the layer of abdominal fat), diabetes mellitus and others diseases of the endocrine system, hypercoagulable states, increased levels of homocysteine (a special sulfur-containing acid), peripheral vascular diseases, connective tissue pathologies.
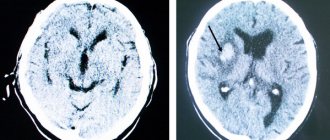
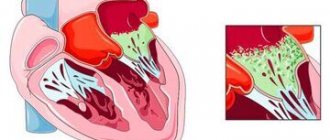
Of course, each of the vascular accidents has its own predisposing factors. Thus, necrosis of an area of the heart muscle occurs mainly in those people who have hypertrophied the wall of the left ventricle, sometimes the coronary vessels spasm, and amyloidosis has developed. Risk factors for stroke are predominantly heart rhythm disturbances, hemoglobinopathies, brain tumors, endocarditis or rheumatic heart valve disease. However, both diseases are based on a similar development mechanism. This is a blockage of an artery supplying the heart or brain with a blood clot that either formed on the surface of an atherosclerotic plaque or “flew off” from the heart or veins of the lower extremities.
Since both the mechanism and most of the risk factors are identical, there are many similarities in measures to prevent stroke and heart attack. Let's talk about this.
Non-drug preventive measures
This:
- Nutrition. Clinical studies in the prevention of stroke and heart attack have confirmed the effectiveness of a low-calorie diet, which will be rich in fruits, vegetables and nuts, and will also include the mandatory consumption of fish and garlic. There should be almost no foods rich in animal fats and trans fats in the diet. The amount of table salt also needs to be reduced - to 3-5 g per day.
- Physical activity. It is optimal to calculate your individual daily load so that it lasts at least 30 minutes a day, and the heart rate does not exceed 60% of the calculated maximum frequency.
- Weight loss. The body mass index should not exceed 25–27 kg/m2, otherwise the weight becomes an additional burden on the blood vessels. To reduce it, you need to choose a therapeutic diet. You may also need drugs to prevent stroke and heart attack, which will reduce your appetite.
- Independence from bad habits. Nicotine and ethanol damage all layers of the vascular walls and increase blood viscosity. Giving up these bad habits leads to restoration of the cardiovascular system within three years (maximum changes occur in the first 3–6 months). This reduces the risk of vascular accidents by 60%.
- Correction of psychological state. Based on clinical research data, anti-stress programs, psychotherapy or work with a psychologist for stress, depression, and loss of social support reduces the risk of vascular accidents by 34%, and a second heart attack by 29%. In some cases, drugs from the group of antidepressants were prescribed for psychological prevention of stroke and heart attack.
Medicinal preventive measures
Various drugs are used to prevent the development of cardiovascular accidents. In the last section, we already talked about medications that help reduce appetite and restore emotional balance: they are not required to be used, but only help reduce risk factors. But there are also drugs for the prevention of stroke and heart attack that actually reduce the risks of these diseases. They are recommended by the World Health Organization.
Antihypertensive drugs
There is a close relationship between vascular accidents and blood pressure levels. Thus, an increase in the “lower” pressure figure by only 7 mm Hg. Art. increases the risk of heart attack by 27%, death of a part of the brain by 42%, and also more likely leads to the development of heart failure and kidney pathologies. Therefore, an important step in the prevention of stroke and heart attack is lowering blood pressure.
People who have a low risk of vascular accidents (no bad habits, excess weight, diabetes) need to reduce their blood pressure if it exceeds 140/90 mmHg. Art. For those who have diabetes, chronic kidney disease, or cardiovascular pathologies, numbers should not be allowed above 130/90 mmHg. Art.
For such prevention of stroke and heart attack, drugs can be used from different groups. Basically, these are angiotensin-converting enzyme blockers (ACEIs). Such drugs not only help maintain blood pressure at target values, but also prevent changes in the myocardium that occur with hypertension and coronary artery disease.
In addition to ACE inhibitors, beta blockers can be used. Their task is to reduce the heart's need for oxygen. The drugs slow down the heart rate. Non-selective representatives of this group are not prescribed for bronchial pathologies.
Other antihypertensive drugs for the prevention of stroke and heart attack may include diuretics. They are prescribed mainly when only the “lower” pressure increases. They are effectively combined with ACE inhibitors, reducing the risk of vascular accidents.
Lipid-lowering therapy
Based on the results of multicenter studies, effective prevention of stroke and heart attack requires a mandatory reduction in cholesterol and low-density lipoproteins. For this purpose, drugs from the groups of statins or fibrates are used.
When prescribing lipid-lowering therapy, the performance of the liver, kidneys, and heart is carefully monitored. Taking these drugs continues until the cholesterol level reaches 1.8 mmol/l, if no side effects occur.
Often, statins or fibrates are supplemented with the use of omega-3 fatty acids. These substances are especially effective for secondary prevention - preventing recurrence of a vascular accident.
Antithrombotic therapy
The key role in the development of cardiovascular accidents is played by platelet activation. Therefore, in people at high risk, antiplatelet therapy is a necessary condition for prevention.
The standard of care for such therapy is aspirin, used in low doses (50–100 mg/day). It inhibits the enzyme cyclooxygenase, which blocks the formation of a substance called thromboxane A2 in platelets. In this case, blood platelets do not settle in areas of the vessels where there are atherosclerotic plaques or where there is a low blood flow rate. Consequently, then there will be no substrate that can “come off” and clog one of the arteries - feeding the brain or heart.
One of the representatives of such drugs for the prevention of stroke and heart attack is Thrombo ACC 50 or 100 mg. It is acetylsalicylic acid (ASA). Each tablet containing ASA is film-coated with an enteric coating, and this is not without reason. According to a number of studies, the use of an enteric form reduces the risk of complications from the gastrointestinal tract and improves tolerability of the drug during long-term therapy.1 Acetylsalicylic acid helps reduce the risk of blood clots and directly prevent myocardial infarction and stroke.2
*There are contraindications, please consult a specialist before use
1B. V. Kosarev, S. A. Babanov “Clinical pharmacology of modern antiplatelet agents and their place in the pharmacotherapy of coronary heart disease and associated conditions”, Breast Cancer Cardiology, No. 5, 2013
2R.
M. Gazizov, E. A. Atzel “The use of acetylsalicylic acid for primary and secondary prevention of cardiovascular diseases” Breast Cancer Medical Review, No. 11, 2014 p.827-831 RUS-GPS-THR-NON-12-2018-1415
Information as a protective factor
Experienced doctors often talk about the need to massively explain to ordinary people how to prevent stroke and heart attack. The point is not that the majority simply do not think about the possible consequences of their careless attitude towards their own health, but that in the event of damage to the circulatory system, the correct and timely actions of others can save a person. To help yourself or your loved ones in time, you need to:
- recognize the first signs of the disease, which include regular pain in the head or heart, increased fatigue, shortness of breath even after minor exertion, high blood pressure;
- provide first aid to the victim, and do it as quickly as possible (in most cases, minutes count);
- promptly call doctors for emergency hospitalization, which should occur no later than 4-6 hours after the attack.
These actions will not only help the patient survive, but will also greatly facilitate the process of rehabilitation and restoration of key body functions.
Antihypertensive therapy
Hypertension is not only the main risk factor for the development of the first IS, but also increases the risk of recurrent stroke, cardiovascular morbidity and mortality. To date, the results of 7 largest studies on the effective treatment of hypertension and simultaneous reduction in the risk of stroke in 15,527 patients [35] included in the observation period from 3 weeks to 14 months after a cerebrovascular episode for 2 to 5 years have been summarized.
This meta-analysis included the following studies:
• Dutch TIA trial (study of the β-blocker atenolol),
• PATS (indapamide diuretic study),
• HOPE (angiotensin-converting enzyme inhibitor study - ACE, ramipril),
• PROGRESS (study of the ACE inhibitor perindopril with/without the diuretic indapamide),
• as well as 3 smaller studies with a sample of patients.
The PROGRESS (Perindopril pROtection aGainst REcurrent Stroke Study) clinical trial is the first published large-scale prospective study of BP control during secondary prevention in stroke survivors [34]. The results of the PROGRESS study showed that long-term (four-year) antihypertensive therapy based on a combination of perindopril and indapamide reduced the incidence of recurrent stroke by an average of 28% and the incidence of major CVDs (stroke, MI, acute vascular death) by an average of 26%. It has been shown that antihypertensive therapy leads to a reduction in stroke not only in hypertensive patients, but also in normotensive patients, although its effect is more significant in hypertensive patients. The combination of perindopril (4 mg/day) and indapamide (2.5 mg/day), used for 5 years, prevented 1 recurrent stroke in 14 patients who had suffered a stroke or TIA.
Data obtained from the LIFE ( Losartan Intervention For Endpoint reduction in hypertension ) and ACCESS (The Acute Candesartan Cilexetil Therapy in Stroke Survivors) trials [37] suggest that the use of angiotensin II type 1 receptor antagonists may also have a beneficial effect on patients suffering from cerebrovascular diseases. This position was confirmed by the results of the MOSES study (MOrtality and morbidity after Stroke - Eprosartan vs nitrendipine in Secondary prevention), which indicate a decrease in the number of first-time cardiovascular events and the total number of cerebrovascular episodes in patients who suffered stroke, when treated with eprosartan, and also indicate on the advantages of this angiotensin II receptor blocker over nitrendipine in terms of the degree of preventive effect on high-risk patients.
Summarizing the data from published studies, we can recommend antihypertensive therapy to all patients with TIA or IS after the acute period, regardless of the presence of a history of hypertension, in order to prevent recurrent strokes and other vascular accidents. The optimal strategy for drug therapy for hypertension, the absolute target level of blood pressure, as well as the degree of blood pressure reduction today, from the standpoint of evidence-based medicine, have not yet been determined and must be determined strictly individually. The recommended reduction in blood pressure is on average 10/5 mmHg. Art. It is important to avoid a sharp decrease (especially in patients with suspected hemodynamic stroke or patients with bilateral stenosis of the carotid/vertebral arteries). Taking into account the recommendations of ESO (European Stroke Organization, 2008/2009 [28]) and AHA-ASA (American Heart Association/American Stroke Association, 2011 [29]), when choosing specific drug therapy, it is also necessary to take into account the presence of an occlusive lesion in the patient’s extracranial sections of the main arteries and concomitant diseases (pathology of the kidneys, heart, diabetes, etc.).
What foods must be present in the diet?
Speaking about a healthy diet, it is necessary to note the mandatory inclusion of vegetables and fruits of different colors. Fortifying your diet with flavonoids (found in citrus fruits) has also been shown to reduce the risk of ischemic stroke.
Proteins of plant and animal origin are building materials. The daily diet should include meat and fish dishes. It is better to give preference to low-fat varieties and sea fish. To ensure your body gets protein, eat more nuts and legumes.
Plant foods also lower blood pressure and improve vascular elasticity. Add whole grains, brown unprocessed rice, and vegetable oils such as canola, olive, and flaxseed to your diet.
Dairy products should be consumed with a low percentage of fat, especially since many people are now diagnosed with lactose intolerance. If this is your case, and after consuming dairy products you feel discomfort, it is better to drink low-lactose milk or plant milk, or avoid it altogether.
Nutrition is an essential part of preventing stroke and dementia. Without a balanced diet and healthy foods, not a single pill will protect you from atherosclerosis. We are what we eat, don't forget that!
What foods should be excluded from the diet?
In order to minimize the risk of stroke, it is better to avoid certain foods. For example, from table salt. Excessive salt consumption can lead to the development of hypertension, one of the complications of which is stroke. People with high blood pressure and older people should reduce their salt intake.
Do not add salt to prepared foods or cook with salt. Healthy spices such as turmeric, black pepper, and basil will diversify the taste of food and make it less bland.
Turmeric is the best care for the brain. Curcumin penetrates directly into brain cells, bypassing the barrier between the circulatory system and the central nervous system.
Beneficial properties of curcumin:
- powerful antioxidant;
- has an anti-inflammatory effect;
- helps improve memory in people with Alzheimer's disease;
- helps new brain cells grow;
- relieves symptoms of depression by increasing serotonin and dopamine levels.
It can be added to food or taken as a dietary supplement.
The effect of curcumin on the body is confirmed by scientific research data, for example, the publication Antidepressant activity of curcumin: involvement of serotonin and dopamine system, Shrinivas K., 2008 states that the use of curcumin reduced symptoms of depression more effectively than the use of antidepressants.
You should also limit the consumption of foods with a high glycemic index (sugar, sweet carbonated drinks, juices, confectionery, ice cream, etc.). They sharply increase blood glucose levels. Their constant use can lead to the development of diabetes, which, in turn, contributes to the development of diseases of the cardiovascular system. These include, among other things, vascular atherosclerosis, a condition that precedes a stroke.
Since the progression of atherosclerosis is associated with increased cholesterol levels, it is necessary to review the structure of the diet and try to avoid eating refined and fatty foods. It’s better not to fry food, but to stew it (with the addition of healthy spices it will be very tasty!), season it not with sunflower oil, but with olive oil, which preserves the health of blood vessels and is included in the healthy Mediterranean diet.
Anticoagulant therapy
It has been established that in more than 67% of cases, strokes develop against the background of cardiac pathology; and about 15% occur against the background of chronic atrial fibrillation.
A breakthrough in the secondary prevention of IS in patients with atrial fibrillation was the use of vitamin K epoxide reductase inhibitors (warfarin, dicumarol, acenocoumarol, phenindione), which reduced the incidence of recurrent strokes in atrial fibrillation from 12 to 4%. The mechanism of action of drugs in this group is the suppression of vitamin K-dependent synthesis of biologically active forms of blood coagulation factors II, VII, IX and X. Doses of drugs that ensure maximum effectiveness of oral anticoagulant therapy largely depend on the individual sensitivity of the patient, and therefore A prothrombin test and international normalized ratio (INR) are used to monitor therapy.
It must be emphasized that therapy with oral anticoagulants after non-cardioembolic ischemic stroke is not more effective than therapy with antiplatelet agents (acetylsalicylic acid - ASA), but leads to a greater number of bleedings [7, 32, 41. However, drugs in this group (with achieving the target INR level of 2 ,0–3.0) are the drugs of choice for the secondary prevention of cardioembolic stroke (in patients with non-valvular atrial fibrillation in both permanent and paroxysmal forms), as well as in most other conditions accompanied by cardiac embolism.
The advantages of warfarin over antiplatelet therapy in the secondary prevention of IS are most clearly demonstrated in the EAFT and ACTIVE W studies.
The EAFT (European Atrial Fibrillation Trial) study included 455 patients with non-rheumatic atrial fibrillation who had suffered a minor IS or TIA within 3 months before inclusion in the study. As the primary endpoint, the study analyzed the incidence of vascular death, nonfatal stroke, nonfatal myocardial infarction, and systemic (noncerebral) thromboembolic episodes recorded at least once every 4 months. Patients were prescribed an open-label oral anticoagulant (the drug was chosen by the attending physician) until an INR of 2.5–4.0 was achieved, or using a double-blind method—ASA (300 mg/day) or placebo. The rate of reaching the end point was 8% per year for patients receiving oral anticoagulants, 17% in the control group. Thus, indirect anticoagulant therapy is more effective than ASA therapy as secondary prevention of thromboembolic episodes in patients who have suffered an IS or TIA [21].
The ACTIVE W (Atrial fibrillation Clopidogrel Trial with Irbesartan for prevention of Vascular Events) study analyzed the effectiveness of warfarin therapy (up to an INR of 2.0–3.0) compared with combined antiplatelet therapy ASA (75–100 mg/day) and clopidogrel (75 mg/day). The study included 6702 patients with atrial fibrillation and one or more risk factors for stroke (age 75 years and older; hypertension; previous IS or TIA; decrease in left ventricular ejection fraction below 45%; peripheral atherosclerosis; coronary artery disease or diabetes in people 55– 74 years old). The primary endpoint was the incidence of IS, non-cerebral thromboembolic events, MI and vascular death. The safety criterion was the incidence of hemorrhagic complications. The study was interrupted in September 2005 due to evidence of superiority of warfarin over combination antiplatelet therapy: 5.64% of patients receiving antiplatelet therapy and 3.94% of patients receiving warfarin reached the end point (p = 0.0002). It should be noted that more than 3/4 of the patients were initially treated with warfarin. The risk of hemorrhagic complications in the study groups did not differ and amounted to 2.4 and 2.2% per year (p = 0.67) in the groups of combined antiplatelet and anticoagulant therapy [6].
However, despite the convincing evidence base, the use of warfarin and other drugs in this group is associated with a number of clinical problems, such as genetically determined resistance to therapy, variability of the anticoagulant effect depending on the diet and concomitant therapy, as well as the need for monthly INR monitoring, which is not always done by patients.
Recent years have been marked by the emergence of several drugs whose anticoagulant effect does not require laboratory monitoring. The drugs dabigatran, a direct thrombin inhibitor, and rivaroxaban, a selective and reversible inhibitor of factor Xa, have proven their effectiveness in the primary and secondary prevention of stroke due to atrial fibrillation, comparable to warfarin, and well tolerated in the RELY [17] and ROCKET AF studies [33 ] respectively.
Anticoagulant therapy after cardioembolic stroke must be carried out for a long time or for at least 3 months after IS that occurred against the background of acute MI [44]. There are conflicting opinions about when anticoagulant therapy should be started. After a TIA or minor stroke, therapy (with warfarin, dabigatran or rivaroxaban) should begin immediately, but in the case of a severe stroke with signs of extensive infarction, according to neuroimaging methods (for example, when the lesion size is more than a third of the blood supply of the middle cerebral artery), anticoagulant therapy is necessary start in a few weeks (the issue must be resolved individually in each case).
Patients with atrial fibrillation and stable coronary artery disease should not combine oral anticoagulants with ASA [26]. Anticoagulant therapy may be preferable for patients with aortic atheroma [20], fusiform basilar artery aneurysm [22], or cervical arterial dissection [24].
Today, according to evidence-based medicine, the use of oral anticoagulants for the purpose of secondary prevention is recommended for patients with atrial fibrillation who have had a stroke, as well as for patients with verified cardioembolic origin of stroke. Moreover, if warfarin is used as an oral anticoagulant, the target INR level is 2.0–3.0 [28, 29]. When using rivaroxaban or dabigatran, INR monitoring is not required.
Antiplatelet therapy
The effectiveness of the use of antiplatelet agents to prevent recurrent IS has been confirmed by many researchers. Four antiplatelet drugs have been shown to reduce the risk of recurrent IS after stroke or TIA.
The results of a meta-analysis of data from 287 studies, including 212 thousand patients with a high risk of occlusive vascular events, showed that against the background of antiplatelet therapy, the number of cases of non-fatal stroke decreased by an average of 25%, and vascular mortality - by 23%. Moreover, according to a meta-analysis of 21 randomized trials that compared antiplatelet therapy with placebo in 18,270 patients who had a stroke or TIA, antiplatelet therapy leads to a 28% relative risk reduction in nonfatal stroke and a 16% relative risk reduction in fatal stroke [ 10].
Acetylsalicylic acid
The clinical effectiveness of ASA for the secondary prevention of IS was first shown in 1977. Subsequently, numerous international placebo-controlled studies demonstrated that ASA at a dose of 50–1300 mg/day is effective in the prevention of recurrent IS or TIA [10, 15].
The first experience in world clinical practice of using small doses of ASA (1 mg/kg/day) in patients with cerebrovascular pathology due to hypertension, carried out at the Research Institute of Neurology of the Russian Academy of Medical Sciences, showed a rapid and persistent elimination of platelet hyperaggregability due to an almost 3-fold decrease in the initial concentration of thromboxane A2 in the blood regardless of the gender of patients and the type of ischemic cerebrovascular accident. The study included patients with TIA and post-IS [5].
Two large international controlled studies compared the effectiveness of different doses of ASA for patients with TIA or IS (1200 vs. 300 mg/day and 283 vs. 30 mg/day) [25, 40]. In both studies, high- and low-dose ASA was effective in preventing IS, but higher doses of ASA were associated with a higher risk of gastrointestinal bleeding [10].
When choosing the optimal daily dosage of ASA for the prevention and treatment of IS, its side effects play an important role. Like other non-steroidal anti-inflammatory drugs, ASA can have both local (due to irritation of the mucous membrane) and systemic (by reducing the synthesis of prostaglandins) damaging effects on the mucous membrane of the gastrointestinal tract (GIT) when taken orally, including. including the occurrence of erosions and ulcers, as well as the development of gastrointestinal bleeding. The frequency of this complication directly depends on the daily dose. Thus, the side effect of ASA on the gastrointestinal mucosa decreased when taking 300 mg/day compared with the use of higher (1200 mg/day) doses of ASA and amounted to 31 and 41%, respectively, for discomfort in the abdominal area, 3.1 and 4. 8% for gastrointestinal bleeding (UK-TIA Study Group, 1991) [25]. At the same time, the ESPS 2 (European Stroke Prevention Study 2) study showed that low doses of ASA do not completely eliminate its ability to induce bleeding [19].
To eliminate the adverse effect of ASA on the gastrointestinal mucosa, various dosage forms with an enteric coating have been proposed, for example thrombo ASA. Absorbed from the upper part of the small intestine, this drug causes local ulcerogenic effects to a much lesser extent.
Ticlopidine
The effectiveness of ticlopidine (thienopyridine) was assessed in three randomized trials in patients with cerebrovascular disease. The CATS (Canadian-American Ticlopidine Studi) trial compared the effectiveness of ticlopidine 250 mg/day with placebo in the prevention of stroke, MI, or death due to vascular pathology in 1053 patients with IS. Ticlopidine has been shown to lead to a 23% reduction in the relative risk of meeting the combined endpoint of the study [27]. The TASS (Ticlopidine Aspirin Stroke Study), which compared the effectiveness of ticlopidine (250 mg twice daily) and ASA (650 mg twice daily) in 3069 patients with a recent minor stroke or TIA [30], demonstrated a reduction in the relative risk of stroke. by 21% over a 3-year follow-up, as well as a slight (9%) reduction in the risk of end events (stroke, MI, death due to vascular pathology) when using ticlopidine.
The most common side effects of ticlopidine: diarrhea (approximately 12%), gastrointestinal symptoms, rash, hemorrhagic complications, are identical to those that occur when taking ASA. Neutropenia was observed in approximately 2% of patients receiving ticlopidine in the CATS and TASS studies. However, the incidence of particularly severe complications was less than 1%; in almost all cases they were reversible and disappeared when the drug was discontinued. In addition, thrombocytopenic purpura has been described.
Clopidogrel
The effectiveness of clopidogrel was assessed in comparison with ASA in the CAPRIE study (Clopidogrel Versus Aspirin in Patients at Risk of Ischemic Events, [14]). More than 19 thousand patients with stroke, MI or peripheral vascular disease were randomized to receive ASA at a dose of 325 mg/day or clopidogrel at a dose of 75 mg/day. The primary end event - IS, MI, death due to vascular pathology - occurred with a frequency of 8.7% lower in patients receiving clopidogrel compared to the ASA group.
Two studies [12, 36] indicated a relatively greater effectiveness of clopidogrel (compared to ASA) for patients with diabetes and patients who have already had an ischemic stroke or myocardial infarction. In general, clopidogrel is safer when taken compared to ASA and especially ticlopidine. Clopidogrel, like ticlopidine, was less likely to cause gastrointestinal symptoms and hemorrhage compared to ASA. Neutropenia was not noted at all; there were isolated reports of the occurrence of thrombocytopenic purpura [11].
Thus, clopidogrel is slightly more effective than ASA in preventing vascular events. Clopidogrel may be more effective in patients with high vascular risk (history of stroke, peripheral arterial atherosclerosis, symptomatic coronary artery disease, or diabetes) [28].
Dipyridamole sustained release
Dipyridamole is close to ASA in its effectiveness in reducing the risk of recurrent strokes [19].
Combined antiplatelet therapy
Taking into account the different points of application and mechanisms of action of drugs with an antiplatelet effect, as well as the variability of the platelet response, their combined use to achieve an additive effect of aggregation inhibition seems theoretically justified.
Combination of clopidogrel and ASA
The MATCH (Management of Atherosclerosis with Clopidogrel in High-Risk Patients with Recent Transient Ischemic Attack or Ischemic Stroke, [18]) study, involving 7599 patients who had suffered an IS or TIA and had additional risk factors, assessed the effectiveness and safety of combination therapy, which included clopidogrel 75 mg and ASA 75 mg/day in relation to clopidogrel monotherapy at a dosage of 75 mg. The primary outcome event was a composite of stroke, myocardial infarction, death due to vascular pathology, or rehospitalization associated with ischemic episodes. There was no significant benefit of combination therapy over clopidogrel monotherapy in reducing the incidence of primary endpoints or recurrent ischemic events.
The effectiveness of combination therapy with clopidogrel (75 mg/day) and ASA (325 mg/day) compared with ASA monotherapy (325 mg/day) was assessed in the CHARISMA (Clopidogrel for High Atherothrombotic Risk and Ischemic Stabilization Management and Avoidance) study. After 30 months of observation of patients, the incidence of the combined endpoint, which included IS, MI, death from a vascular cause in patients receiving combination antiplatelet therapy, was 6.8% and was less than in the group of patients receiving ASA monotherapy, where this indicator was 7.3% (p = 0.22). Thus, the study did not demonstrate the advantages of combination therapy with clopidogrel and ASA compared with ASA monotherapy for this category of patients [28, 29].
Combination of dipyridamole and ASA
In the ESPS-2 study (European Stroke Prevention Study, [19]), 6602 patients with a history of stroke or TIA were randomized, taking into account the main risk factors for the development of ischemic brain injury, into groups of different regimens of extended-release dipyridamole and ASK. A significant reduction in the risk of stroke was achieved with ASA alone by 18%, dipyridamole alone by 16%, and the combination of both by 37%. No reduction in the risk of death was observed with any of the dosage regimens used. The effectiveness of combination therapy compared with ASA monotherapy was observed in reducing the risk of recurrent stroke (by 23%) and was 25% higher than the effectiveness of dipyridamole monotherapy.
Similar results were obtained in the international randomized, non-blinded study ESPRIT (European/Australian Stroke Prevention in Reversible Ischaemia). The purpose of one of the directions of this study was a comparative analysis of the effectiveness and safety of the combination of ASA (30–325 mg/day) with slow-release dipyridamole (400 mg/day) and ASA monotherapy (30–325 mg/day) in patients who had suffered a TIA or IS ( with a neurological deficit assessed as no more than 3 points on the modified Rankin scale) within 6 months before inclusion in the study. It is important to note that the study included only patients who had suffered atherothrombotic cerebrovascular accidents: 1363 received combination therapy, 1376 received monotherapy. The primary endpoint (vascular death, non-fatal IS, MI, symptomatic hemorrhagic complications) was achieved by 16% of patients receiving ASA monotherapy and 13% of patients receiving combined antiplatelet treatment (hazard ratio [HR] = 0.8; 95% confidence interval [CI] – 0.66–0.98), which allowed the authors to conclude that the combination of ASA and dipyridamole is more effective than ASA in the secondary prevention of vascular complications of IS of atherothrombotic origin. Following the publication of the ESPRIT results, a meta-analysis of studies on the combined use of dipyridamole and ASA, which included all the studies described above, confirmed the reliability of the conclusions of the ESPRIT study [7].
The results of the ESPS-2 and ESPRIT studies formed the basis of the ESO (2008) recommendations for secondary stroke prevention, in which the combination of ASA and slow-release dipyridamole is a first-line drug (along with clopidogrel) as an effective antiplatelet therapy (Class I, level of evidence A ). It should also be noted that for those in whom secondary prophylaxis with oral anticoagulants is indicated but is contraindicated, the ESO also recommends a combination of slow-release dipyridamole and ASA (although the level of evidence for this recommendation is low - class IV, GCP - Good Clinical Practice).
Thus, the range of drugs - antiplatelet agents - with proven efficacy and safety in multicenter studies is quite wide, and therefore the question of choosing an oral antiplatelet agent is logical. When choosing antiplatelet drugs after stroke or TIA, the influence of several factors should be taken into account. Concomitant somatic pathology, side effects, and the cost of the drug may influence the choice of therapy: monotherapy with ASA, clopidogrel or a combination of ASA and dipyridamole. The low cost of ASA promotes its long-term use. However, if you look at it differently, even a small reduction in the frequency of vascular episodes observed with the use of dipyridamole or clopidogrel suggests a certain adequacy of the cost-effectiveness ratio of the drugs, which is comparatively more noticeable than with ASA. In patients who cannot tolerate ASA due to allergies or gastrointestinal side effects, clopidogrel or dipyridamole should also be recommended. The combined use of ASA and clopidogrel may be acceptable for patients who have recently suffered an acute coronary attack or stenting surgery [46].