Signs of pathology
The left hemisphere controls the following body functions:
- logical thinking;
- ability to process received information;
- the ability to operate with accurate data;
- speech function;
- ability to read;
- ability to perceive verbal information.
With an ischemic stroke on the left side, the functions described above are disrupted, and motor activity on the right side of the body becomes difficult or completely stops.
Functions of the cerebral hemispheres (Infographics)
Based on the location of the blood flow disturbance, the following are distinguished:
- Carotid basin. Blockage of the arterial plexus by a thrombus or atherosclerotic plaque is accompanied by hemiparesis, paralysis of the tongue and facial muscles on the right. But if blood flow in the left carotid system is disrupted, the eye on the left suffers. If, against the background of right-sided disorders, the patient experiences visual impairment on the right, then it can be assumed that extensive damage to the left hemisphere caused partial stenosis of the vessels in the right carotid system.
- LSMA. Ischemic stroke in the LSMA basin is accompanied by speech impairment, paralysis of the eye muscles, and a left-sided decrease in the strength and sensitivity of the limbs. Ischemic stroke in the left MCA often has “predecessors” - transient ischemic attacks. If a person is diagnosed with middle cerebral artery syndrome, then neurologists often identify foci of previous micro-strokes.
- Posterior cerebral artery. Ischemic stroke in the posterior cerebral artery is accompanied by loss of visual fields, aphasia, memory loss, monoparesis of the foot or hand on the left. As with ischemic stroke in the left MCA, damage to the posterior cerebral artery rarely occurs suddenly; patients are additionally found to have foci of microdamage to brain tissue.
- Anterior arterial vessel. Paresis or hemiparesis of the limbs with more severe damage to the leg (the arm may not be affected), speech impairment, urination disorder, and the appearance of pathological grasping reflexes. More often, the victim develops an ischemic atherothrombotic stroke, provoked by narrowing of the vessel by deposits due to atherosclerosis.
- Internal cerebral artery. When this vessel is blocked, the symptoms are relatively mild and the person may not be aware of the development of pathology. Patients experience slight weakness and numbness on one side, memory deterioration, the appearance of uncriticism towards their actions and statements, and decreased vision. The cause is the slow formation of a blood clot or atherosclerotic plaque.
- Vertebrobasilar basin. The vessels in the vertebrobasilar basin supply blood to the occipital lobe, cerebellum and brain stem. Ischemic stroke of the left basin in the vertebrobasilar region is accompanied by movement disorders: unsteadiness of gait, problems with coordination and muscle paralysis or paresis.
According to statistics, ischemic stroke is more often diagnosed in the territory of the left middle cerebral artery with characteristic symptoms. Previously suffered microstrokes provoke disruption.
Let's look at the basic information: middle cerebral artery syndrome, what it is and how it manifests itself.
An ischemic stroke of the left hemisphere of the brain, when the middle cerebral artery is affected, causes the following symptoms:
- right-sided paralysis or paresis of the limbs (never occurs with left-sided hemiparesis);
- decreased sensitivity of the skin on the right;
- the emergence of problems with coordination;
- speech disorder;
- smell disorder;
- hearing loss;
- blurred vision;
- decreased memory (sometimes the patient ceases to recognize others, loses previously acquired knowledge and skills);
- loss or impairment of speech (the person loses the ability to speak or slurs words).
Left-sided cerebral stroke is characterized by autonomic disorders:
- causeless anxiety and fear;
- feeling of lack of air, shortness of breath;
- increased sweating;
- heart rhythm disturbances (bradycardia, tachycardia or arrhythmia);
- the appearance of nervous tremors;
- pallor or hyperemia of the skin;
- feeling of heat.
In addition to the symptoms described, due to increased intracranial pressure, a victim of an ischemic attack experiences severe headaches, clouding of consciousness or fainting, and convulsions.
The clinical picture will vary slightly depending on the location of the lesion. In a victim of an ischemic stroke on the left side, speech disorders or motor disorders may predominate.
Short description
The middle cerebral artery (ICD-10 code - I63.0 - I63.8) is the largest branch of the internal carotid artery. It is divided into the left and right MCA and serves as the source of blood supply to the cerebrum, insula and cortex. Since the SMA is part of the circle of Willis, blood flow in the areas supplied by it does not occur through this circle, but through the cortical and meningeal branches.
The incidence rate of this type of pathology is small. Middle cerebral artery stroke is diagnosed in 3% of all cases.
Dangerous consequences
Complications that appear after an ischemic stroke on the left side depend on the location of the lesion on the cerebral hemisphere (hemisphere). Let us consider the consequences characteristic of left-sided ischemic stroke that may persist after treatment and rehabilitation.
Physical activity
If the motor centers are affected, then a person develops:
- sagging of half the face (half-lowered eyelid, swollen cheek, distorted mouth);
- decreased muscle strength (in severe cases, paralysis occurs);
- impaired sensitivity (the skin of the affected limbs reacts poorly to external irritations).
Difficulty in movement and sensory disturbances in left-sided cerebral ischemia occur on the right side of the body.
Internal organs
Ischemic stroke in the left hemisphere is not limited only to disruption of the innervation of muscles and skin; organs located on the right (kidney, lung, and partially the digestive tract) are affected.
The degree of change in the functioning of organs depends on how severe the innervation disorder is:
- Easy. The deviation is minor, the functions are preserved.
- Average. There is a decrease in organ functions. The patient's right side of the chest lags behind when breathing, and there may be problems with digestion and bowel movements.
- Heavy. Paralysis and complete cessation of functions occurs.
Stopping the functioning of the lung, liver or kidney is considered one of the dangerous consequences of an ischemic stroke on the left side. It is noteworthy that the severity of external and internal deviations are not related to each other. People may be paralyzed on the right side of the body, but the functionality of the internal organs is not impaired.
Speech
The centers responsible for speech are on the left. Depending on the area of damage to the hemisphere, the victim will have:
- Difficulty in grammatically constructing sentences. People begin to speak in short, simple phrases reminiscent of telegraph style. Intonation disappears. This occurs when the anterior lobes of the hemisphere are affected.
- Problems with sounds. The patient confuses sounds, placing them incorrectly in words. This is typical for stroke of the posterior lobe.
- Problems with the perception of spoken language. A person hears words addressed to him, but cannot associate them with known concepts. Similar problems arise when trying to read text. Such patients speak mainly in prepositions or conjunctions, with long, but uninformative phrases. The disorder appears with ischemia of the temporal lobe.
- Complete aphasia. Extensive ischemic stroke of the left hemisphere is often accompanied by a complete loss of the ability to speak and perceive speech.
There is also false aphasia, when the impairment of the ability to speak is associated with paralysis of the muscles of the tongue or larynx. Such people understand what is being said to them and can adequately formulate their thoughts, but when they try to speak, the result is slurred, blurred speech or isolated sounds.
Ability to think
The left side of the brain marks the ability for logical thinking. The consequence of a left-sided stroke can be:
- loss of ability to remember numbers (dates, phone numbers);
- inability to perform simple arithmetic operations in the mind (add, multiply);
- difficulty in perceiving abstract concepts;
- difficulty when trying to draw conclusions from the information received;
- difficulty making independent decisions.
Such people do not always understand their condition and often commit stupid or ridiculous actions. They are uncritical of their actions.
Psycho-emotional sphere
Another consequence of a stroke in the left hemisphere is a change in the psyche. The patient may experience depression associated with limited mobility and dependence on the care of loved ones. The person becomes:
- Maudlin. He often feels sorry for himself and cries, saying that he has become a burden to his relatives.
- Restless. Anxiety and fear appear associated with the fear of being left without outside help.
- Aggressive. The patient finds fault with others, conflicts over trifles. May complain to strangers about poor feeding or care, attracting attention to himself.
- Irritable. Such people are dissatisfied with everything, find fault with little things, and often accuse loved ones of waiting for their death.
Often, those who have suffered a cerebral infarction experience sudden mood swings when, during a calm conversation, a person becomes angry, starting to throw objects or punch the bed.
Diagnostic features
For any type of cerebrovascular accident, the outcome of the disease is often decided in minutes.
It is important to notice the first signs of deterioration in the patient’s condition in time in order to be able to provide him with adequate pre-medical care. A left-sided stroke manifests itself with the following symptoms:
- confused consciousness;
- impaired coordination of movements;
- speech becomes slow, often meaningless;
- motor activity decreases sharply;
- the smile becomes unnatural and is skewed to one side.
- There may also be drooping of the corners of the eye on the left side.
If at least one of the listed signs is detected, it is necessary to urgently call emergency help. The sooner the victim receives qualified medical assistance, the greater his chances of survival. Strokes suffered at home are fatal in 95% of cases. But even if the result does not lead to a sad outcome immediately, there is a huge risk of developing a second stroke.
Therapeutic measures
Therapy begins in the first hours after the onset of an attack. It is important to remember that the prognosis and severity of consequences depend on the timeliness of assistance provided.
Patients are prescribed:
- thrombolytics (Urokinase, Fibrinolysin) for resorption of formed blood clots;
- anticoagulants (Warfarin, Heparin), which reduce blood density and prevent recurrent thrombus formation;
- neuroprotectors (Nootropil) and antioxidants (Glycine, Mexidol) to reduce possible damage to brain cells;
- vasoactive agents (Actovegin, Cinnarizine) to improve cellular metabolism.
Regardless of which areas of the brain are affected, clinical stroke is almost always accompanied by arterial hypertension. To reduce and stabilize blood pressure, fast-acting drugs (Captopril, Clonidine) and long-term medications are used to prevent the development of crises (Lisinopril, Prestarium).
In the first days after an ischemic stroke in the left MCA or in other areas, the patient is provided with rest to prevent cerebral edema and prevent a recurrent ischemic attack.
After the person’s condition becomes stable, he is transferred to the general ward and, while continuing drug therapy, rehabilitation measures to restore impaired functions begin.
Symptoms
There are several stages in the development of the disease. Acute lasts for 21 days. Within this stage, the most acute stage is distinguished, lasting approximately five days and characterized by an increase in the brightness and variety of symptoms.
Next comes the early rehabilitation stage, which lasts up to 5 months. At this time, the blood supply to the remaining cells is restored, and compensation tasks are distributed.
The late recovery stage conventionally lasts from the seventh month to a year. At this stage, the affected tissues become scarred. Cysts and glial formations form at the site of damage.
Beginning of the disease
Many people imagine that during an attack a person falls due to sudden paralysis and loses consciousness. Indeed, such a beginning is very characteristic of a blow. At the same time, a person does not feel any warning signs.
Sometimes symptoms begin to increase in waves. The patient's condition either worsens or returns to normal. The pathology resembles a microstroke. Patients complain that, for example, their arm has temporarily failed.
Approximately a third of patients with intact memory, who are able to speak and express their thoughts after an attack, describe certain symptoms that anticipated the attack.
Visual disturbances are noted. Floaters appear before the eyes, parts of the field of vision fall out. Pain occurs.
Motor functions, the ability to sit and turn disappear. Signs of paresis appear. There is a feeling that an arm and leg are paralyzed on one side or both. The patient loses his balance.
The person notices arrhythmia and feels that the pulse disappears. Dizziness appears. Patients often report pain that is described as very severe.
However, they often do not pay enough attention to a sudden speech disorder, the inability of a loved one to utter simple words or answer an easy question. The drooping corner of the mouth on one side and the fact that one of the arms has failed is ignored. Delay in identifying the disease prevents patients from surviving.
Development of the disease
If the warning signs of an attack can be confused with signs of other diseases and attributed to poor health, then the signs of a blow occurring to a person are unlikely to be confused with anything.
If you notice the following symptoms in others, immediately call an ambulance:
- Impaired consciousness. In this case, several degrees are distinguished. With mild and moderate changes, there is stupor, heaviness in the head, lethargy of the patient, fixation of the gaze at one point, and inability to answer questions. With stupor, it is impossible to establish contact with a person; pain and pupillary reflexes remain intact. The most severe disorder is coma. It is almost impossible to survive with this condition.
- Change in breathing. It becomes superficial, weak, sometimes noisy and rapid.
- Inability to move. With a stroke, paresis and paralysis develop.
- Cramps. The whole body is affected by convulsions, muscles tense, and the person is unconscious.
- Distorted face.
- Stiff neck.
Signs of a left-sided injury
Damage to the left side in a stroke leads to muscle weakness on the right side of the body. There is a loss of memory, analysis, and counting. Left-sided stroke is characterized by speech impairments and inability to understand what is heard.
The arm on the right is bent at the elbow, the leg, on the contrary, is extended, the foot is turned inward. Palms clenched into fists.
The emotional background is characterized by dejection and depression. A person is prone to depression, apathy, and isolation. This mood does not increase the chances of improvement.
After a stroke with paralysis on the right side, recovery is more difficult.
Signs of right-sided lesion
Damage to the right hemisphere leads to left-sided hemiparesis. Characterized by a disorder of sensations. A person thinks that he has several legs and arms. Sometimes it seems as if the limbs do not belong to him at all.
After a stroke, the left side is often completely paralyzed.
Rehabilitation therapy
Neurologists have developed a scheme for how to recover from an ischemic stroke in the left MCA or in another area of the brain. It includes:
- Massage. Rubbing and kneading the muscles improves blood supply and helps restore damaged innervation.
- Physiotherapy. A magnet, laser and other hardware procedures are used to improve tissue microcirculation and restore the conductivity of nerve fibers.
- Exercise therapy. An individually selected set of exercises helps restore motor function. With the help of exercise therapy, treatment after stroke, if the side of the body is paralyzed, is carried out by making the patient passive flexion and extension movements in the immobilized limbs.
- Diet. The diet of patients should consist of foods that are easily digestible. You should exclude fatty meats, smoked and pickled foods, baked goods, and also limit the consumption of salt and sugar. It is recommended to include vegetables, vegetarian soups and cereals in the menu.
- Classes with a speech therapist. Necessary for restoration of speech functions.
Neurologists are positive if folk remedies are used in addition to the main treatment. It is recommended to drink tincture of fir cones or decoctions of chamomile, St. John's wort, and sage. Traditional medicine recipes help improve the functioning of internal organs and prevent possible inflammation associated with weakened immunity.
Treatment
The sooner the diagnosis is made, the better the treatment prognosis. If you hit the therapeutic window, dangerous consequences can be avoided. This is the period from the beginning of oxygen starvation of the brain (the appearance of the first symptoms) until the development of irreversible disorders - 3-6 hours after the attack.
Treatment for stroke can be basic or specific.
It begins in the ambulance and continues in the intensive care setting. The objectives of basic treatment include stabilizing the patient and supporting the functioning of vital organs. Therapy includes the following actions:
- sanitization of the respiratory tract, connecting the victim to a ventilator (artificial lung ventilation) in case of breathing problems;
- control of body temperature and pressure;
- maintaining optimal water-alkaline balance in the body;
- relief of seizures;
- regulation of cardiac activity through intravenous administration of drugs.
Specific therapy helps restore blood circulation and prevent the development of irreversible consequences. Treatment includes the following methods:
- drug therapy;
- physiotherapy;
- surgical intervention aimed at restoring blood circulation and reconstructing blood vessels.
Drug treatment
To relieve symptoms, eliminate blood stagnation and the consequences of a stroke, the following groups of medications are prescribed:
- Thrombolytics – Actilyse, Gemaza. Used in the first 3-6 hours after an attack to dissolve blood clots and restore blood circulation to the brain.
- Nootropics – Phezam, Semax, Piracetam, Cerebrolysin. Reduce brain swelling and protect neurons from damage. During the recovery period, nootropics improve the processes of concentration and memory.
- Anticoagulants – Heparin, Clopidogrel. Prescribed to prevent recurrent blood clot formation and blood thinning. The drugs are contraindicated in the presence of bleeding and hemorrhagic stroke.
- Diuretics – Furosemide, Torasemide. They remove excess fluid from tissues and help relieve cerebral edema.
- Angioprotectors – Troxevasin. Restore vascular permeability and prevent microthrombosis.
- Vasoactive agents – Cavinton, Vinpocetine. They improve blood circulation in ischemic brain tissues and help restore lost neuronal functions.
- Metabolic drugs – Mildronate, Actovegin. Promotes increased blood circulation and tissue metabolism.
- Volume-substituting agents – Albumin, Reopoliglyukin. They normalize hemodynamics and replenish the missing volume of fluid in the body.
Recovery period after a stroke
Rehabilitation helps patients regain lost motor functions, speech, and other consequences of a stroke. The recovery period is divided into 3 stages:
- Acute – first 3-4 weeks. Rehabilitation is carried out in intensive care conditions. Bed rest and medication are prescribed.
- Early recovery stage – 6 months after the attack. The victim is prescribed a diet. Spicy, fried, smoked foods and salt are excluded from the diet. To restore motor skills, physical therapy (PT) is prescribed.
- Late recovery period – a year after the attack. It takes place on an outpatient basis or in special rehabilitation centers.
The following methods help eliminate the consequences of a stroke and improve the prognosis:
- Kinesitherapy – treatment by position. The affected limbs are temporarily fixed in a splint. Prescribed for pain relief and after operations.
- Massage. The procedure improves blood circulation in tissues and helps remove excess fluid from the body.
- Reflexology. Acupuncture is prescribed for spastic conditions. The procedure speeds up the tasks of therapeutic exercises and has a positive effect on the nervous system.
- Exercise therapy. Exercises help improve muscle tone and strengthen the respiratory and cardiovascular systems. They help restore mobility to the injured arm or leg.
- Working with a speech therapist-aphasiologist. Prescribed for speech restoration. The doctor re-teaches the patient to speak and develops ligamentous-motor skills. Prescribes exercises for articulation and phonation.
- Psychotherapy. A visit to a psychologist helps stabilize the emotional background and avoid depression. Classes are held individually or in groups with other patients.
Features of rehabilitation
The rehabilitation period after a right-sided stroke lasts a long time. After an ischemic type of pathology, recovery is more successful; many patients manage to regain lost functions and return to normal life. After a hemorrhagic stroke, rehabilitation rarely gives positive results, so people remain disabled.
During the recovery period, measures are taken to normalize the ability to move, mental activity, memory, and psycho-emotional state.
Sanatorium recovery
Rehabilitation after a stroke is allowed to be carried out at home, but doctors strongly recommend giving preference to treatment in sanatoriums. In these institutions, the patient is always under the supervision of specialists, has the opportunity to undergo all the necessary procedures, and eat right.
In the process of sanatorium-resort rehabilitation, the following methods are used:
- physiotherapy;
- sessions with a psychologist;
- physiotherapeutic procedures;
- taking medications;
- massage;
- breathing exercises.
A set of measures is developed for each patient individually, depending on which functions are impaired and the severity of the consequences.
Home rehabilitation
At home, there are fewer opportunities to restore the body than in a sanatorium. But the patient can also, under the supervision of relatives, perform therapeutic exercises that help restore motor ability. If the family has the opportunity, you can hire a physical therapy instructor.
In addition to therapeutic exercises, it is necessary to do body massage and spend more time in the fresh air. Relatives also need to feed the patient in accordance with the diet prepared by the doctor and visit the clinic to undergo the necessary physiotherapeutic procedures.
Traditional methods of rehabilitation
Patients use traditional medicine for recovery after a right-sided stroke. Home remedies are based on natural ingredients and help enhance the effects of medications and physical therapy.
The most effective folk remedies for stroke on the right side are the following recipes:
- Alcohol tincture of fir cones. To prepare, you will need to pour 6 cones with vodka, close tightly and leave to infuse in a dark place for 7 days. Then take the medicine 3 times a day, a teaspoon.
- Onion juice with honey. Mix onion juice and honey in equal proportions and consume a tablespoon every day on an empty stomach.
- A decoction of pine needles and lemon. Pour 5 large spoons of chopped pine needles into 500 ml of water, boil for a few minutes, then strain. Finely chop half a lemon and add to the broth. Let the drink brew for 3-4 hours. You can take the decoction about 100 ml 3 times a day.
Emotional and mental stress
These disorders are quite difficult to eliminate even with the help of a competent psychologist or psychotherapist, since a person perceives reality completely differently. His attitude towards himself as a “burden” for loved ones, a sense of his own inferiority - all this leads to the development of deep depression and apathetic states. In other cases, the patient shows aggressiveness towards himself and the people around him.
Also not least is the fear of a possible future, the likelihood of remaining bedridden for life, and the fear of death from a second stroke.
Establishing diagnosis
First of all, the diagnosis of TIA consists of identifying cerebral and focal symptoms, as well as their subsequent regression after some time. As already mentioned, if the developed symptoms do not disappear within 24 hours, then one can safely suspect the development of a stroke.
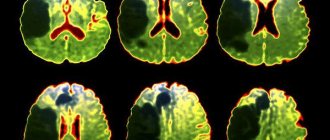
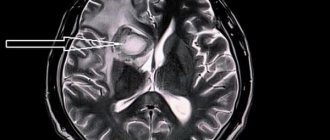
Differential diagnosis can be made between stroke and TIA on the first day of disease development using computed tomography. When a stroke develops, the image can reveal the presence of an ischemic zone (penumbra) in the nervous tissue. If there is a transient ischemic attack, then there may be no changes in the image.
Lumbar puncture, which is used to differentiate ischemic disorders and hemorrhages, in the event of an ischemic attack will not provide reliable data necessary for making a diagnosis. A fairly informative study is ultrasound of the BCA, which allows one to determine the presence of stenosis in the brachiocephalic arteries.
If there are signs of focal lesions and general cerebral symptoms, treatment should be started immediately.
Appendix A1. Composition of the working group
| Krylov Vladimir Viktorovich | Academician of the Russian Academy of Sciences, Director of the Clinical Medical Center of the Moscow State Medical and Dental University named after. A.I. Evdokimova, head of the department of emergency neurosurgery at the Research Institute of Emergency Medicine named after. N.V. Sklifosovsky, Head of the Department of Neurosurgery and Neuroresuscitation, Moscow State Medical and Dental University. A.I. Evdokimova |
| Dreval Oleg Nikolaevich | Doctor of Medical Sciences, Professor, Head of the Department of Neurosurgery of the Russian Academy of Postgraduate Education of the Ministry of Health of the Russian Federation |
| Dzhindzhikhadze Revaz Semenovich | Candidate of Medical Sciences, Associate Professor of the Department of Neurosurgery of the Russian Academy of Postgraduate Education of the Ministry of Health of the Russian Federation |
| Lazarev Valery Alexandrovich | Doctor of Medical Sciences, Professor of the Department of Neurosurgery of the Russian Academy of Postgraduate Education of the Ministry of Health of the Russian Federation |
| Dashyan Vladimir Grigorievich | Doctor of Medical Sciences, Professor of the Department of Neurosurgery and Neuroresuscitation, Moscow State Medical and Dental University. A.I. Evdokimova |
| Nikitin Andrey Sergeevich | Candidate of Medical Sciences, assistant at the Department of Neurosurgery and Neuroresuscitation, Moscow State Medical and Dental University. A.I. Evdokimova |
| Petrikov Sergey Sergeevich | Doctor of Medical Sciences, Professor of the Russian Academy of Sciences, Deputy Director of the Research Institute of Emergency Medicine named after. N.V. Sklifosovsky, professor of the department of neurosurgery and neuroreanimation of the Moscow State Medical and Dental University named after. A.I. Evdokimova |
Classification
TIAs with a clinical picture of vascular damage in the vertebrobasilar area account for about 70% of diagnosed attacks. Taking into account the duration of the attack, mild, moderate and severe forms are distinguished. In the first case, an ischemic attack lasts up to 10 minutes, in the second - up to several hours with the elimination of symptoms after the attack, in the third - several hours with the persistence of residual symptoms after the end of the attack. The diagnosis of TIA is made if the duration of the attack does not exceed 24 hours, and the neurological and autonomic disorders are reversible.
Prevention
To prevent pathology, doctors recommend leading a healthy lifestyle and eliminating provoking factors. Risk factors include consumption of salty, fatty foods, low physical activity, excess weight, habits that are harmful to blood vessels and health in general - smoking, abuse of alcoholic beverages.
Ischemic attacks are the first signs of serious disturbances in the functioning of the blood flow system and the entire body. More than 30% of people who have suffered an attack are subsequently diagnosed with a cerebral infarction or stroke. At the initial stages of development, the pathology is treatable. Based on the diagnostic results, the doctor will determine the cause of the disorders and prescribe a course of treatment.
Causes
Ischemic stroke on the left side can be provoked by the following unfavorable factors:
- hypertonic disease;
- various kidney diseases;
- pathological changes in the endocrine system (very often the development of a stroke for this reason ends in paralysis of the left side of the human body);
- cerebral atherosclerosis;
- excess body weight;
- increased sugar or cholesterol levels;
- inactive lifestyle;
https://youtube.com/watch?v=ntLFPLBSMGg
- abuse of bad habits (tobacco smoking, alcohol addiction);
- periodic and excessive physical activity;
- diseases of the blood vessels that arose due to the victim’s retirement age;
- hereditary predisposition to stroke or diseases that provoke it.
Analysis of the letter: Stroke in bLSMA of ischemic type
Greetings, dear guests and readers of my blog. Today there will be an analysis of another case written by Natalya in this question-answer section.
insultu-net.ru
Good afternoon I hope very much for your help. My father had an ischemic stroke two weeks ago, age 67 years. Diagnosis after examination: acute cerebrovascular accident in the LSMA basin of ischemic type, dysarthria, right-sided pyramidal insufficiency. According to the ECG: upon admission: sinus rhythm, heart rate 65, horizontal position of the EOS, HF, diffuse changes in the myocardium, decreased blood supply to the anterolateral sections, ECG three days later: sinus bradycardia and improved nutrition of the anterolateral sections.
On MRI: a zone of pathological signal is visualized, characteristic of an ischemic lesion of an irregular oval shape, measuring 39 by 32 mm, without perifocal edema of the brain substance. Speech, writing, and reading are impaired. He is aggressive and doesn’t really understand what happened to him, swears as best he can, has very incoherent speech, confuses words, letters, everyday skills, everything is fine.
The situation is complicated by the fact that the parents live in the far Moscow region and the situation with the doctors is a bit tense. If possible, please comment. Thanks in advance!! I am attaching the discharge summary and treatment using the links.
Natalya, hello. I have read the documents attached to the letter. The stroke itself (“Diagnosis after examination: stroke in the bLSMA of the ischemic type”) that your father had on August 10, 2015, from the data indicated in the discharge summary, is more related to a stroke of moderate severity. Neurological deficits are not expressed to a degree that can render a person bedridden.
The size of the infarction is not large, apparently cortical or subcortical (the specific location of the lesion is not indicated anywhere in the documents), because the functions of the cortex were more affected (reading, writing, dysarthria again..). One of the biggest problems with this arrangement is a violation of mental functions; coupled with aggression, this can complicate the recovery process, mainly due to the patient’s failure to follow recommendations (taking medications).
Mild hemiparesis will most likely recover within the first month. Now the most important thing is to complete the course of recommended treatment in full and not allow blood pressure surges, because most likely the stroke itself occurred against the background of one of these surges.
If he is taking treatment, then he should try to complete the full course of taking the medications specified in the recommendations. One thing that confuses me is the number of medications prescribed, perhaps not all at once, but in courses... Because if you take it all at once, then disgust with refusal of all treatment can occur even in a healthy person. As for aggression, he needs to take atarax prescribed by a doctor, and if the aggressive background persists, then he can additionally consult with a psychiatrist to adjust the treatment.
And so, I think that not all is lost and we can assume a relatively good restoration of lost functions. As for aggression - 50/50, it is difficult to say with certainty the timing and prospects in the future.
Features of rehabilitation and recovery after stroke
After the blood supply to the brain is restored and the threat to life is eliminated, the patient who suffered from a left-sided stroke begins the rehabilitation process. It begins in the hospital a few days after leaving the acute phase, and continues at home and in specialized centers.
Depending on which body functions are to be restored, the patient is prescribed the following procedures and manipulations:
- therapeutic exercises - in the first days after an attack, performing passive exercises with the help of medical personnel or relatives; subsequently – increasing the load and performing exercises independently, working on simulators;
- massages of the paralyzed part of the body - classic, acupressure, manual;
- physiotherapeutic procedures and therapeutic baths - help restore the connection between neurons;
- classes with a speech therapist are necessary in the early stages of rehabilitation; subsequently, according to a specialist’s program, the patient can restore speech independently;
- the use of non-traditional techniques (acupuncture, hirudotherapy) - to restore sensitivity to paralyzed parts of the body;
- training in writing, reading, perception and analysis of information - carried out by specialists or relatives;
- working with a psychologist helps reduce depressive mood and gain confidence in one’s own strength.
An integral condition when undergoing a rehabilitation course is periodic drug treatment on the recommendation of a rehabilitation physician, correction of the daily and nightly sleep patterns, and adherence to a diet. Only an integrated approach will help restore lost skills and return, if not completely, then at least partially to normal life.
Rehabilitation period
How long a person can live after a stroke depends on various factors. An important role is played by the patient’s attitude, as well as the support of his relatives.
Great attention is paid to the timeliness of providing qualified assistance
The rehabilitation period begins after therapeutic treatment. Sometimes surgical intervention is required - in cases of hemorrhage in the brain.
What the recovery process will be depends on the degree of damage to the brain and which areas were involved. Sometimes a person will have to learn to speak again, to understand this world.
Rehabilitation measures:
- massages;
- therapeutic and health-improving physical education;
- baths;
- speech therapy classes;
- speech restoration;
- teaching writing skills.
Unfortunately, a patient will not be able to completely return to his former life after a stroke, regardless of its form. But his relatives are able to provide him with comfort and at least partially restore his lost skills.
If motor function has been affected as a result of damage to the left hemisphere, the patient will be given a massage, including manual massage, to restore sensitivity to the paralyzed part of the body. As a rule, it is better to entrust this to a specialist.
Therapeutic baths help restore neural connections. As already mentioned, the patient’s mood itself is also important.
It is important to work on yourself at different stages of recovery, to master primitive skills again
In case of speech impairment, sessions with a speech therapist are recommended. Working with a psychologist will also help. In some cases, even specialized doctors recommend resorting to alternative medicine methods.
- How long does it take for the liver to recover after hepatitis?
- How much valerian to take to calm down the pills?
- How long do people with diabetes live without treatment?
A left-sided stroke, just like a right-sided stroke, is a rather dangerous disease. If a person survives, the rehabilitation period can drag on for years. And the duration and quality of life will depend on the care, the mood of the patient himself and the effectiveness of drug therapy. In any case, brain damage has its consequences, which negatively affect all areas of life. In almost 100% of cases, stroke survivors become disabled. Be healthy!