The value of normal hematocrit in humans
The body of a healthy adult contains approximately 4.5-5 liters of blood. It contains formed elements and cells - red blood cells, platelets, leukocytes, as well as a liquid part called plasma.
Some blood components, for example, red blood cells, do not have all the necessary components of a human cell, losing them during the maturation process. Therefore, red blood cells and platelets are called blood cells, not cells.
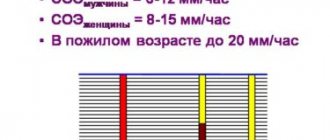
In different categories of patients, the normal values of various parameters of the blood tested will differ. So, for most men, the hematocrit will be higher: 40-41%, and in some cases it can reach up to 51%, which is due to its slower renewal.
In healthy women, the hematocrit usually ranges from 36 to 42%. This is due to physiological features - due to regular menstrual bleeding, blood is renewed more often to replenish its volume. During pregnancy, from the 20th week, the indicator begins to decrease, which is also not considered a deviation.
In children, hematocrit differs at different age periods:
- 44-62% for newborns;
- 32-43% for babies up to three months;
- 36-43% for children under one year of age;
- 35-47% (up to 52% for boys) - in the first ten years.
In subsequent years, the hematocrit norm depends on gender and practically corresponds to the values of an adult.
Preparation
Donating blood for a general analysis does not require special preparation, but to identify an adequate clinical picture of the formed elements and hematocrit, it is recommended to adhere to the following rules:
- Blood donation is performed on an empty stomach;
- stopping smoking in the morning on the day of the test (blood is donated in the morning);
- refusal of physical activity the day before and on the day of delivery of the biomaterial;
- prohibition of taking anticoagulants, antiplatelet agents and other drugs that affect the blood coagulation system 3 days before the study;
- abstaining (if possible) from stress and emotional experiences on the eve of the study;
- refusal to carry out diagnostic procedures (x-ray, ultrasound and other studies) the day before donating blood.
Sources:
- A.A. Kishkun, Doctor of Medical Sciences, Prof. Guide to laboratory diagnostic methods, - GEOTAR-Media, 2007.
- Mandy Flannery O'Leary, MD, MPH, FCAP. Hematocrit. — Laboratory Medicine, Medscape, 2014.
- Andrew S Artz, MD, MS. Anemia in Elderly Persons. - Hematology, Medscape, 2015.
Methods for determining hematocrit
The indicator is determined as a percentage by calculating the amount of formed elements in whole blood. It is calculated using special instruments or manually.
Centrifugation using the Wintrobe method
The blood is exposed to centrifugal force for 10-30 minutes. The formed elements are heavier than plasma, so they settle to the bottom of the test tube. The hematocrit is determined by the ratio of sediment to the total volume of biomaterial.
Calculation of the indicator using the formula
The ratio of the number of red blood cells to the total blood volume can be calculated mathematically. To do this, the following indicators are required:
- total hemoglobin concentration (ctHB);
- red blood cell count (RBC);
- mean erythrocyte volume (MCV);
- mean erythrocyte hemoglobin concentration (MCHC).
The hematocrit number (HCT) is determined by one of the formulas:
- HCT (%)=(ctHB (mmol/l)*0.0485+0.0083)*100
- HCT (%)=0.1*MCV*RBC
- HCT (%)=ctHB/MCHC*100
Direct blood cell counting method
In a given volume of biomaterial, visible blood elements are counted manually or using hematological analyzers. The method is highly accurate, and the measurement process does not take much time - no more than five minutes, but the equipment required is very expensive.
Manual counting method
Blood collected using an anticoagulant is placed in a dry, clean tube and allowed to settle. In this case, the formed elements that have greater weight settle to the bottom of the container, and the light plasma rises to the top, forming two fractions of red and yellow colors, respectively. The hematocrit indicator can be determined by the divisions on the test tube. This method is the least accurate, its error is up to 20%, so it is currently not used in laboratories.
Micronutrients for the hematopoietic system
Hematopoiesis - that is, hematopoiesis - is a set of stages in the transformation of a stem cell into one of the elements that make up the blood. Let us repeat that the role of vitamins B6, B9 and B12 and iron in these processes is a priority, and jumps in hct levels always one way or another lead to the conclusion about a lack of these substances.
In addition to these four, attention should be paid to other nutritional compounds.
- Vitamin E is a fat-soluble form and can accumulate in any tissue, but mainly in fat. Protects red blood cell membranes from damage due to oxidative stress;
- Vitamin C – adds iron to the process of hemoglobin synthesis, starting with the formation of red blood cells in the red bone marrow;
- Vitamin A (retinol) – helps transfer iron from “reserves”;
- Vitamin B2 (riboflavin) – helps not to remove the necessary iron prematurely through the genitourinary system;
- Vitamin D2 (ergocalciferol) - helps transport iron from storage cells to the red bone marrow, where hemoglobin is produced in the red blood cell;
- Copper - helps iron oxidize to the level of digestibility (ferrous);
- Omega 3 and Omega 6 fatty acids stimulate and regulate the formation of new cells in the process of erythropoiesis (the formation of red blood cells).
Often, if hct tests are questionable, you can turn to an additional blood test for vitamins and microelements that are involved in hematopoiesis. Based on detailed data, we can talk about developing a personal complex of micronutrients that will meet the needs within the framework of the individual characteristics of the body.
When is a hematocrit test performed?
Most often, hematocrit is determined as part of a general (clinical) blood test. Therefore, at present this parameter of a clinical blood test is not prescribed separately. The hematocrit level changes when:
- disorder of the blood coagulation system;
- dehydration;
- anemia or polycythemia;
- bleeding.
Assessing the hematocrit level is important when determining indications for the need for blood transfusion or the effectiveness of blood transfusion, during hemodialysis, and some operations. To determine the hematocrit number, venous or capillary blood is taken.
Indications and preparation for analysis
Indications for hematocrit analysis are symptoms indicating the development of anemia or other diseases of the blood or hematopoietic system. These include:
- Pale or jaundiced skin
- Enlarged spleen, liver
- Changes in the size of lymph nodes
- Digestive disorders
- Skin and hair problems (rashes, ulcers on mucous membranes, hair loss or brittleness)
In addition to identifying anemia, the analysis allows us to identify other diseases, for example, polycythemia (a chronic disease in which the bone marrow produces an excess amount of red blood cells) of various origins. This study is also used when it is necessary to assess the need for blood transfusion and calculate the required volume of transfusion.
No special preparation is required for the hematocrit test. It is necessary to follow the standard rules for conducting a general blood test:
- Blood is drawn early in the morning.
- You should not eat food 6-10 hours before the test.
- Avoid alcohol 2-3 days before the procedure.
Patients who smoke are advised to abstain from smoking for at least 2-3 hours before blood collection. If these recommendations are not followed, the analysis may give unreliable results. This is due to the fact that the composition of the blood is subject to strong fluctuations depending on the action of various environmental factors.
Increased hematocrit
An increase in hematocrit occurs with an increase in the number of blood cells - polycythemia - and a lack of fluid in the body. An increase in the indicator may indicate serious diseases accompanied by blood thickening and thrombotic complications.
Causes
Hematocrit increases due to stress, taking corticosteroid drugs and diuretics, traumatic shock accompanied by intense pain, as well as when climbing to high altitudes, smoking, or playing sports using anabolic steroids to gain muscle mass.
An increase in the indicator may indicate the following diseases:
- dehydration due to vomiting, profuse diarrhea, overheating or heat stroke, excessive sweating, insufficient fluids;
- heavy bleeding in the midst or immediately after it stops;
- pathologies accompanied by a decrease in blood plasma volume, for example, peritonitis, thrombosis, diabetes, burn disease;
- renal dysfunction - hydronephrosis, oncology, polycystic disease;
- vitamin B12 or iron deficiency anemia;
- leukemia;
- erythrocytosis;
- defects and coronary heart disease, heart failure;
- intestinal obstruction;
- bronchial asthma, pulmonary emphysema, obstructive bronchitis.
Symptoms
An increase in blood viscosity leads to thrombus formation. The latter can manifest itself in the form of tingling or various pains and numbness in the limbs. If the cause of increased blood viscosity is not determined in time, serious complications such as myocardial infarction, stroke, gangrene and even death may develop.
Treatment
Treatment is carried out not for the changed hematocrit level itself, but for the conditions or diseases that caused these changes. In some situations, when serious causes for a slightly changed hematocrit level have been excluded, no treatment is required. But usually such situations are short-lived, in the case of physiological reasons for changes in hematocrit levels.
Why is it rising?
The reasons for increased hematocrit may be the following:
- dehydration (dehydration), which can occur with diarrhea, severe vomiting, increased sweating, diabetes;
- malignant blood diseases, such as leukemia;
- erythremia (primary erythrocytosis);
- secondary erythrocytosis;
- neoplasms in the kidneys, in which the formation of erythropoietin increases;
- hydronephrosis and polycystic kidney disease;
- congenital heart defects;
- hemoglobinopathy;
- pulmonary failure;
- a decrease in the volume of the liquid part of the blood as a result of pathological conditions such as burn disease, peritonitis, shock and others;
- taking diuretics;
- taking corticosteroid drugs;
- intestinal obstruction;
- oxygen starvation (when high above sea level, in smokers), during which the body begins to produce more hemoglobin in order to increase the transfer of oxygen to the cells.
This is how blood hematocrit is determined
Decreased hematocrit
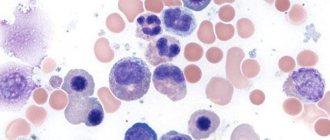
A decreased hematocrit occurs when the number of red blood cells or their size decreases - erythrocytopenia. The cause may also be the accumulation of water in the body when the blood becomes thinner - hyperhydration, as well as hyperproteinemia or the accumulation of proteins in the plasma, which contributes to fluid retention.
Causes
A decrease in hematocrit is facilitated by prolonged immobility, fasting or a strict diet, taking anticoagulants and antiplatelet agents, and intravenous infusions in large volumes; heavy drinking, chronic alcoholism, excessive salt intake, menstruation in women.
Also, a downward change in the indicator may indicate the following pathologies:
- iron-, B12- or folate-deficiency anemia;
- severe bleeding;
- impaired hemoglobin production in sickle cell anemia;
- fibrous degeneration of the liver - cirrhosis;
- disruption of the urinary system;
- hemolysis of erythrocytes - destruction of red blood cells due to hereditary mutation, autoimmune processes or toxic effects on blood cells;
- malaria, typhoid fever;
- oncological diseases of the bone marrow or its metastatic lesions from other organs;
- an increase in the amount of protein in plasma due to vomiting, diarrhea, blood cancer and other conditions.
During pregnancy, a decrease in hematocrit can be observed in the case of toxicosis, a very young age of the mother, multiple pregnancies, a short period of time between pregnancies, and also after the 20th week of gestation due to a physiological increase in fluid in the body.
Symptoms
A decrease in hematocrit in the blood is accompanied by hypoxia of various organs, since it is the red blood cells that normally carry oxygen throughout the body. This condition is manifested by the following symptoms:
- fast fatiguability;
- general weakness;
- drowsiness;
- increased heart rate and breathing;
- feeling of lack of air;
- headache, dizziness;
- decreased memory and concentration;
- hair loss;
- marbling or pallor of the skin.
Blood chemistry
A laboratory blood test that gives an idea of the condition of internal organs and their functionality. Allows you to evaluate metabolism and find out about the lack of microelements in the body.
Due date and how to prepare
A biochemical blood test is taken in the morning on an empty stomach from a vein. You should not eat 12 hours before the test. You can only drink clean water, but drinks, including tea, coffee and any others, are not allowed. 24 hours before the test you must give up alcohol, smoking and physical activity.
Metrics collected
- Glucose
- blood sugar level; - Urea
is a parameter important for assessing kidney function; - Cholesterol
is an element that determines the risk of cardiovascular diseases; - LDL cholesterol
is an element that determines the risk of cardiovascular disease; - HDL cholesterol
is an element that determines the risk of cardiovascular disease; - Residual blood nitrogen
is a parameter important for assessing kidney function; - Atherogenicity coefficient (Ka)
- shows the risk of developing atherosclerosis; - Total bilirubin
is an indicator that may indicate the presence of jaundice; - Total protein
is an indicator that allows you to evaluate liver function; - AST (AST)
is an indicator that allows you to evaluate the work of the heart; - AlAt (ALT)
is an indicator that allows you to evaluate liver function; - Lipase
is an indicator that allows you to evaluate the functioning of the pancreas; - Amylase
is an indicator that allows you to evaluate the functioning of the pancreas; - Gamma-GTP
is an indicator that allows you to evaluate liver function; - Antistreptolysin-O
is an indicator that is used in the diagnosis of rheumatism; - Rheumatic factor
is an indicator that is used in the diagnosis of autoimmune diseases; - CRP (C-reactive protein)
is an indicator that can indicate inflammation in the body; - Alkaline phosphatase
is an indicator of many different diseases and health problems; - Albumin
is a protein that performs many functions in the body; - General lipids
are fats that perform structural and regulatory functions in the body; - Triglycerides
are fats that perform structural and energy functions in the body; - Phospholipids
- an indicator that assesses the metabolism of fats in the body, indicating liver and kidney diseases, and indirectly diabetes mellitus; - Protein fractions
are indicators that may indicate inflammatory processes, infectious and other diseases in the body; - Calcium
is an important element for the nervous and cardiovascular systems; - Potassium
is an element that normalizes heart rhythm and regulates water balance; - Sodium
is an element that regulates the volume of extracellular fluid; - Chlorine
is an element that regulates the acid-base balance of the blood; - Iron
is an element important for binding, transporting and transmitting oxygen throughout the body.
Decoding the results: norm and deviation
The normal values of the blood parameters studied in each laboratory are different and depend on the gender, age and condition of the patient. Only a doctor can make a correct interpretation of the blood test results and make a diagnosis, taking into account all aspects of the patient’s health. Below are frequently examined blood parameters, their normal values, and what a deviation from the norm may indicate in the general case, and not in the specific case. To obtain an individual interpretation and diagnosis, you should consult a doctor.
Glucose
Norm
: 3.33 - 6.38 millimoles per liter;
Deviation
: May indicate diabetes mellitus or hypoglycemia.
Urea
Norm
: 2.5 - 8.3 millimoles per liter;
Deviation
: May indicate a kidney problem.
Cholesterol
Norm
: 3.6 mmol/l - 7.8 mmol/l;
Deviation
: may indicate obesity, endocrine disorders, genetic diseases and others.
LDL cholesterol (bad cholesterol)
Norm
: 2.02 - 4.79 mmol/l (men), 1.92 - 4.51 mmol/l (women);
Deviation
: Excess may indicate liver disease, kidney disease, obesity and other diseases.
HDL cholesterol (good cholesterol)
Norm
: 0.72 - 1.63 mmol/l (men), 0.86 - 2.28 mmol/l (women);
Deviation
: A decrease may indicate various diseases and poor nutrition.
Residual blood nitrogen
Norm
: 14.3 - 28.6 mmol/l;
Deviation
: May indicate a kidney problem.
Atherogenic coefficient (Ka)
Norm
: 14.3 - 28.6 mmol/l;
Deviation
: May indicate a kidney problem.
Total bilirubin
Norm
: 8.5 - 20.55 µmol/liter;
Deviation
: May indicate liver problems and jaundice.
Total protein
Norm
: 48 - 73 grams per liter (newborns), 47 - 72 grams per liter (children up to one year old), 61 - 75 grams per liter (from 1 to 4 years), 52 - 78 grams per liter (from 5 to 7 years) , 58 - 76 grams per liter (from 8 to 15 years), 65 - 85 grams per liter (adults);
Deviation
: May indicate liver problems or nutritional deficiencies.
AsAt (AST)
Norm
: 10 - 38 IU/l;
Deviation
: May indicate problems with the heart.
AlAt (ALT)
Norm
: 7 - 41 IU/l;
Deviation
: May indicate liver problems.
Lipase
Norm
: 0 - 190 units per 1 ml of blood (adults), 0 - 130 units per 1 ml of blood (children);
Deviation
: may indicate problems with the pancreas.
Amylase
Norm
: less than 53 U/l;
Deviation
: may indicate problems with the pancreas.
Gamma-GTP
Norm
: 15 - 106 µmol/l (men), 10 - 66 µmol/l (women);
Deviation
: may indicate problems with the liver and a number of other diseases.
Antistreptolysin-O
Norm
: less than 200 units;
Deviation
: May indicate rheumatism.
Rheumatic factor
Norm
: less than 14 IU/ml;
Deviation
: May indicate autoimmune diseases.
CRP (C-reactive protein)
Norm
: 0 - 10 mg/l;
Deviation
: May indicate inflammation in the body.
Alkaline phosphatase
Norm
: 20 - 140 IU/l;
Deviation
: Can indicate many different diseases and health problems.
Albumen
Norm
: 35 - 52 g/l;
Deviation
: Can indicate many different diseases and health problems.
General lipids
Norm
: 4 - 8 g/l;
Deviation
: Can indicate many different diseases, aging and diets.
Triglycerides
Norm
: 0 - 2.25 mmol/l;
Deviation
: may indicate pathology of internal organs.
Phospholipids
Norm
: 2.52 - 2.91 mmol/l;
Deviation
: may indicate liver and kidney diseases, and indirectly diabetes mellitus.
Protein fractions
Norm
: total protein 65 - 85 g/l;
Deviation
: may indicate inflammatory processes, infectious and other diseases in the body.
Calcium
Norm
: 2.15 - 2.50 mmol/l;
Deviation
: can lead to diseases of the nervous and cardiovascular systems and others.
Potassium
Norm
: 3.5 - 5.5 mmol/l;
Deviation
: can lead to diseases of the cardiovascular, muscular system and others.
Sodium
Norm
: 136 - 145 mmol/l;
Deviation
: may indicate a malfunction of the kidneys, liver, endocrine system and other body systems.
Chlorine
Norm
: 98 - 107 mmol/l;
Deviation
: may indicate metabolic disorders and other diseases.
Iron
Norm
: 8.95 - 30.43 µmol/l;
Deviation
: Can lead to disruption of various body functions.
When to take it
A biochemical blood test must be taken:
- As prescribed by a doctor;
- As part of routine medical examinations and examinations;
- To assess the functioning of internal organs and the functionality of the body;
- To determine the need for microelements;
- For information about metabolism;
- After suffering from infectious or somatic diseases.
Serological blood test
A laboratory blood test that involves the interaction of antibodies and antigens. It is carried out to identify infectious diseases and the stage of the infectious process.
Due date and how to prepare
A hormonal blood test is taken in the morning on an empty stomach from a vein.
Serological blood test methods
- To confirm the diagnosis, an antigen corresponding to the suspected disease is added to the blood serum, and if there is a reaction, then there are antibodies to the disease and the patient is sick.
- To determine the type of infection, antibodies of the expected type are added to the serum, and if there is a reaction, then there is an infection in the blood that corresponds to the added antibodies.
What is the result of a serological blood test?
The analysis provides an answer to whether there is a suspected infection in the human body.
When to take it
- when prescribed by a doctor;
- if you suspect a certain infection;
- to prescribe the correct treatment.