Symptoms
Pulmonary fibrosis after coronavirus - symptoms are expressed by the following signs:
- development of shortness of breath at rest
- decreased exercise tolerance
- increase in respiratory rate
- fast fatiguability
- the color of the skin of the fingers and nail plates becomes pale with a blue tint
- dry cough
- dizziness
- decrease in saturation - oxygen content in the blood
To confirm the diagnosis, a CT scan of the lungs is prescribed, on which the radiologist will see all the changes that have occurred. Pulmonary fibrosis, symptoms after covid in computed tomography images are expressed:
- areas of decreased transparency, the degree of dullness of which indicates the severity of the lesion
- white areas indicate fluid in the lungs after coronavirus
Based on the totality of signs, doctors determine the scope of drug treatment and further rehabilitation.
What is heart valve disease?
Each heart valve is a complex mechanism that, like gate leaves, opens and closes the flow of blood through the chambers of the heart and from the heart to the aorta and pulmonary artery. Valves allow blood to flow in only one direction.
The human heart consists of four cavities - two atria and two ventricles. Blood enters the atria of the heart through the veins, from the atria to the ventricles, from the ventricles to the large arteries (aorta and pulmonary artery). Along the path of its movement, at the junction of the atria into the ventricles and the ventricles into the arteries, there are heart valves - movable valves consisting of individual elements (cusps). If the heart valve does not work properly, problems with blood flow (in the form of backflow or obstructed blood flow) occur.
The nature of changes in the heart valves can be divided into two groups: - valves that do not close completely (valve insufficiency), which leads to regurgitation (backflow) of blood through the valve in the opposite direction (for example, from the aorta to the left ventricle) and - valves valves that do not open properly (valve stenosis), causing blood flow to become obstructed and restricted.
Valvular heart defects are relatively common, accounting for 20 to 25% of all organic heart diseases in adults. The most frequently detected defects are the mitral valve, the second most common are lesions of the aortic valve. In almost all cases in children and in 90% of cases in adults, the occurrence of the defect is associated with rheumatism. The second most common disease is bacterial endocarditis. Rare causes of the formation of the defect can be systemic lupus erythematosus, scleroderma, rheumatoid arthritis, and in adults - atherosclerosis, coronary heart disease.
Of particular note is a condition that often occurs in healthy people called mitral valve prolapse, or “click syndrome,” “slamming valve syndrome,” “click and murmur syndrome,” “mitral valve aneurysmal bowing syndrome,” “Barlow syndrome,” Engle’s syndrome. and others. Cuffer and Borbillon in 1887 were the first to describe the auscultatory phenomenon of systolic clicks (clicks) of the heart. The term "mitral valve prolapse", which is currently most widespread, was first proposed by J Criley.
The mitral valve blocks the reverse flow of blood from the left ventricle into the left atrium. Prolapse is a condition when the valve leaflets, at the moment of contraction of the ventricle, do not close the hole “tightly”, but bend into the cavity of the atrium, allowing blood to pass in the opposite direction. This is accompanied by a characteristic clicking sound or heart murmur. The amount of blood returning to the atrium can serve as a measure of the severity of the defect.
Depending on when the heart valve defect appeared, primary and secondary prolapse are distinguished: 1. Primary (idiopathic) valve prolapse is congenital, caused by a genetic defect in the structure of the connective tissue that makes up the valve leaflets. 2. Secondary (acquired) heart valve prolapse appears as a result of chest trauma, rheumatism, myocardial infarction and other causes. Today, some experts consider primary mitral valve prolapse to be just a variation of the norm, and not a disease at all.
How long do abnormal changes in the respiratory system last?
Post-Covid pathological changes persist in the lungs for a period of three to six to eight months. The duration is individual in each clinical case and depends on the state of the immune system, the presence of concomitant diseases, early or late treatment.
If even a slight manifestation of symptoms indicating the formation of pulmonary fibrosis appears, it is necessary to visit a doctor and undergo the recommended examination. The earlier treatment and pulmonary recovery are started, the lower the risk of complications.
Causes
In general cases, these include chronic diseases and inflammatory processes. Less commonly, the disease occurs after radiation exposure, trauma, severe allergic reactions, infections and weakened immunity.
However, if we talk about the causes of cardiac fibrosis (what it is is indicated above), it should be noted that in this case the main provoking factor is myocardial infarction, as well as age-related changes in the body.
But even here everything is ambiguous. If, for example, a person is diagnosed with aortic fibrosis, then there is a high probability that this was caused by injuries, infectious diseases and allergies. When it turns out that the mitral valve leaflets are affected, then most likely the prerequisites in this case are rheumatic processes. They negatively affect connective tissue.
Therefore, each case must be considered separately.
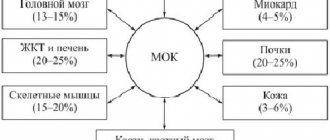
How to avoid complications
Why is pulmonary fibrosis dangerous after coronavirus? With a large area of fibrous growths, not only the lungs suffer. The appearance of foci of calcification in the lungs after coronavirus reduces the volume of inhaled and exhaled air. Complications arise in the functioning of the cardiovascular system - the heart, in order to saturate the organs with oxygen, begins to pump blood faster. Deformation of blood vessels appears, an increase in pressure is observed, and blood clots form.
The consequences from the nervous system are expressed by manifestations of oxygen starvation of the brain: a decrease in cognitive functions, performance, memory problems, rapid fatigue, and the development of a persistent depressive state.
Timely treatment of pulmonary fibrosis after coronavirus gives a favorable prognosis. Further rehabilitation is aimed at eliminating the pathological condition and minimizing the risk of complications.
If the pressure is not like that of an astronaut
— When I try to sleep on my left side, my heart starts to work like a hammer drill - at first I even thought that the neighbors below were crushing the wall. What could it be?
- The description looks like tachycardia or palpitations with an enlarged left ventricle. It is necessary to be examined to determine the exact cause and correct the functioning of the heart. This in itself is not dangerous, but can lead to heart failure and other complications. That is why, in case of hypertension, it is necessary to promptly normalize high blood pressure so that the heart does not increase in size and its functionality is not impaired.
— Please tell me how to protect yourself from heart disease? What examinations need to be completed?
— You need to start by measuring your blood pressure at home. If you feel pain behind the sternum or in the heart area, you need to consult a doctor and get an ECG. You should check a biochemical blood test - cholesterol and its fractions - to see if there is an indirect threat of coronary disease, the cause of which may be atherosclerosis. For a more detailed examination of the heart, the use of echocardiography is effective, allowing you to check the structure of the heart, valve function, contractility and other parameters. Modern methods include CT coronary angiography, which determines the degree of blood flow disturbance. There are methods of functional diagnostics that can be intermediate - the first manifestations of disorders can be checked using stress tests - for example, bicycle ergometry or treadmill, 24-hour ECG monitoring.
— When should you start monitoring your blood pressure?
- If there is evidence, then from childhood. But even if there are no problems, you should undergo an annual medical examination. As a rule, problems begin between the ages of 40 and 45 for men, and after 55 for women. At this age, you need to begin to control the situation - regularly measure your blood pressure. But this does not mean that you cannot get a myocardial infarction in your youth. For example, the risk of developing myocardial infarction in young women is high when two factors are combined - smoking and taking hormonal contraceptives. In addition, early heart attacks and strokes can be a consequence of genetic predisposition, that is, hereditary.
— Everyone knows that smoking is bad for the heart. What can you say about electronic cigarettes?
— Less information has been accumulated on electronic cigarettes, but the trend is the same - atherosclerosis and hypertension develop more often. Among smokers, the mortality rate from cardiovascular diseases is twice as high.
— I am 79 years old and have atrial fibrillation. I’ve been taking three medications for three years, but to no avail...
- You are receiving good treatment. Atrial fibrillation or atrial fibrillation leads to dangerous complications - thrombosis and strokes. The fact that these diseases did not develop is precisely a consequence of three years of use of these drugs. Since you have had atrial fibrillation for more than three years, it is permanent. In this situation, you need to achieve a normal heart rate so that the heart rate is 60 - 70 beats per minute. If, with the help of the prescribed medication, you manage to achieve these numbers, then good, the treatment is correct.
— I wore a holter* for a day, which showed 8568 ventricular extrasystoles. Please tell me what this indicator says?
- You have more extrasystoles than a healthy person should have. This may be due to emotional stress, as well as functional heart diseases. You definitely need to see a cardiologist to determine the exact cause. If the indicator persists, shortness of breath and other ailments may subsequently appear. To make an appointment with me or other doctors at the REAVIZ clinic, call (846) 321-21-21.
Treatment
Every person who is concerned about the topic under consideration is interested in whether fibrosis originating from the left ventricle of the heart can be cured?
If the pathology has not developed so clearly as to lead to regurgitation or stenosis, therapy is not required. You just need to lead a healthy lifestyle, follow a routine, avoid stressful situations, and also regularly see a cardiologist and perform echocardioscopy.
However, in the presence of arterial hypertension, myocardial ischemia, atrial fibrillation, etc., it will be necessary to select therapy according to the nature of the disease.
In the event that cardiac fibrosis is already accompanied by all of the listed symptoms, or even failure has occurred, you will need to take glycosides and diuretics. As a rule, Digoxin (dosed at 0.25 mg) is prescribed, half a tablet twice a day. The course lasts 5 days. Among the diuretics, Indapamide is prescribed, which should be taken 2.5 or 1.5 mg in the morning.
If the pathology is severe, then the treatment of cardiac fibrosis cannot be done without Veroshpiron (50 or 25 mg each), Furosemide (20-80 mg) and Diuvera (5 or 10 mg). All of these medications must be taken in the morning.
Pathology of the heart valves
Another common type of disease. Fibrosis of the heart valves (more precisely, the mitral valve) is a pathology that occurs as a result of rheumatic processes or infections. How is it characterized? The sealed mitral valve leaflet. As a result of fibrosis, it loses its elasticity. Scars often form on the valves.
With this pathology, the valve loses its ability to open the hole located between the ventricle and the atrium, and then close it.
If this condition is not treated in time, diffuse myocardial fibrosis or insufficiency of coronary blood supply may occur.
The symptoms are the same as in the case of other types of pathologies. What about diagnostics? In this case, a more effective method than ultrasound performed for cardiac fibrosis is two-dimensional echocardiography.
This procedure allows you to study the mitral valve in the projection of transverse and longitudinal sections. A two-dimensional image makes it possible to assess changes in the valve structure, detect regurgitation, and also calculate the pressure in the pulmonary artery.
Also, in case of fibrosis of the heart valves, radiography is required. The resulting image demonstrates congested pulmonary roots and pleural lines along the costal and interlobar pleura.
Deviations in IVS fibrosis
Hemodynamic intracardiac disorders begin to manifest themselves 3-5 days after the baby is born.
Diagnosis at such an early age is very difficult. There is no extraneous noise in the heart, since blood pressure is proportional in both ventricular sections.
This effect has a name – neonatal pulmonary hypertension. Over time, the pressure begins to decrease. Then the gradient necessary for diagnostics is created. And the blood begins to circulate from the area of high pressure to the area of low pressure (from left to right).
Due to its pumping through the pathological channel, which occurs under pressure, hypertrophy of the walls of the ventricular cavity occurs. Then the main artery, which connects the heart to the lungs, expands.
The pressure rises rapidly, and a reflex spasm of the lung tissue occurs. Due to the blood discharge of oxygen-depleted fluid, hypoxia occurs in all muscle tissues and organs. The result is oxygen starvation.
Symptoms of the disease
Symptoms of the identified disease vary and appear depending on the degree of damage, stage of development and general condition of the body. The main manifestations of the initial stage of damage to the heart muscle are:
- Severe shortness of breath and slight cough on exertion.
- Fast fatiguability.
- The appearance of hypertension.
If treatment is not started on time, the condition worsens with the addition of more significant symptoms:
- Heart rhythm disturbance.
- Frequent dizziness and tinnitus.
- Heaviness and pain in the chest and right hypochondrium, due to stagnation of blood in the liver.
- Changes in blood pressure.
The development of the disease at different stages of the lesion can take years and the symptoms can be quite varied.
Surgical intervention
It is necessary if the patient is diagnosed with significant cardiac fibrosis. Because pathology of this level leads to stenosis of the valve ring of the 2nd, 3rd and 4th degrees.
As a rule, in these cases, patients are referred for valve replacement surgery or surgical dissection of adhesions, also called commissurotomy.
Such procedures are carried out in different ways nowadays. They can operate on an open heart using a heart-lung machine. Or use intravascular access through peripheral large arteries, which include the femoral, inguinal, etc.
As a rule, modern mechanical prostheses made of synthetic materials are used. Biological ones, made from wild boar valves, are used a little less frequently.
If a patient with cardiac fibrosis has insufficiency of the valve leaflets, surgical repair is performed with sutures on the leaflets that do not close. Or they perform prosthetics.
Diagnostics
Based on all of the above, you can understand what cardiac fibrosis is. This is a pathology that practically does not manifest itself in the early stages, and is later accompanied by symptoms common to this disease, regardless of its type.
Therefore, diagnostic methods are used universally. At the first stage, each patient must pass general clinical urine and blood tests, and also undergo an ECG. However, with their help it is possible to detect only an ischemic or inflammatory process in the myocardium. To make an accurate diagnosis, the following instrumental methods are necessary:
- Ultrasound of the heart. This is the most reliable way to determine the degree of narrowing or valve insufficiency. It also allows you to evaluate the contractile function of the myocardium and the volume of blood that enters the aorta during systole.
- Radiography. Using this method, it is possible to detect myocardial hypertrophy as a reaction to congestion in the lungs, heart overload, as well as calcium deposits on the valves.
- MRI and CT. These methods are used if there is a need for differential diagnosis. Or just before surgery.
With the help of the listed diagnostic measures, it is possible to determine not only how severely developed cardiac fibrosis is. They help detect inflammatory processes and viral infections in the body. This is important, because they complicate the course of fibrosis, and therefore they must be taken into account when prescribing therapy and treated.
Aortic root fibrosis
This is one of the most common types of this pathology. There are some features that distinguish it from other cardiac fibrosis.
The aortic root, subject to pathology, is the reason why the patient’s respiratory function is impaired. The blood is simply not enriched with oxygen. This is why many people experience pale skin, shortness of breath, and blue lips.
Due to the fact that the pumping function of the heart is reduced, the blood vessels are overloaded. This is fraught with overflow of organs with venous blood. As a result, the pressure in the arterioles and venules increases and pathological changes occur.
Over time, heaviness begins to be felt on the right side of the body, swelling appears, the contractile function of the myocardium weakens, and heart failure progresses. However, all types of pathologies are fraught with such consequences - be it fibrosis of the interventricular septum of the heart or the aortic root. To avoid them, the disease must be treated. Otherwise, the heart will lose its compensatory capabilities.
Diagnosis of IVS fibrosis
It’s impossible not to talk about her. Suspicion of fibrosis of the heart septum can be identified during an examination of the baby by a cardiologist. If a specialist detects even the slightest symptoms while listening to a muscle organ, he prescribes additional diagnostics using instrumental means.
This will help avoid complications in the future. Today, the diagnosis of any dysfunction or pathology is carried out comprehensively, using ultrasound and X-ray equipment. Two-dimensional Doppler echocardiography, angiocardiography, etc. may be prescribed.
High-quality diagnostics will help to form an objective and holistic clinical picture, as well as clarify all the hidden nuances of the pathological process.
Since fibrosis of the heart septum in infants is detected at an early stage, it is often possible to refrain from performing surgery. But dynamic monitoring of the child’s condition is necessary. In rare cases, a defective shunt closes spontaneously, this happens between 1 and 4 years.
In other situations, conservative therapy or surgical correction is indicated.