Renin is a specific enzyme that is produced in the kidneys. Its functions include monitoring fluid balance and sodium levels. Violations of this balance lead to a sharp increase in blood pressure. Therefore, if hypertension occurs, the patient is prescribed a blood test for renin.
Despite the fact that this enzyme compound is produced by a parenchymal organ, it cannot be considered a true hormone. This is due to the area of influence of this enzyme. It contains only one type of protein. Thanks to this diagnostic test, many serious diseases can be identified.
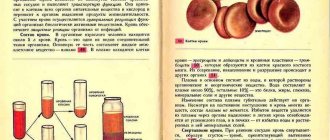
Renin levels depend on blood pressure. The mechanism of influence of this enzyme is complex. Immediately after production, renin enters the blood, resulting in the transition of angiotensinogen to angiotensin I. The latter is then converted into the same substance of the second type. At the same time, the following processes occur: narrowing of blood vessels and activation of the process of aldosterone production. At the last stage, the balance of potassium and sodium is stabilized and blood pressure is normalized.
Aldosterone and renin are related to each other, so doctors often order specific tests to determine their levels at the same time. Data on the obtained ratio are necessary to identify the exact cause of the patient’s ailment.
Active renin results from the synthesis of prorenin. This element is formed in juxtaglomerular cells. The diagnostic scheme must include OAM, liver and kidney tests, ionogram, and biochemical blood test.
Indications for use
An analysis of renin levels in the blood is necessary to determine pathologies accompanied by disruptions in the production of this hormone. Significant reasons for prescribing a laboratory test are:
- potassium deficiency;
- lack of a positive effect when using the usual treatment regimen;
- presence of hypertension in the patient's medical history;
- partial dysfunction of the kidneys and (or) adrenal glands;
- malignant neoplasm in the area of parenchymal organs;
- narrowing of the renal artery.
Interpretation:
- Increased with subsequent secondary aldosteronism: 1. Hypertensive conditions: malignant or severe hypertension, unilateral kidney damage with severe or malignant hypertension, parenchymal renal lesions, renin-secreting tumors, hypertension caused by oral contraceptives, pheochromocytoma.2. Edema normotensive conditions: liver cirrhosis, hepatitis, nephrosis, congestive heart failure.3. Hypokalemic normotensive conditions: juxtaglomerular cell hyperplasia (Barter's syndrome), other nephropathies with loss of sodium or potassium, nutritional disorders with loss of electrolytes. Increase without subsequent secondary aldosteronism: adrenocortical insufficiency, decreased potassium content in the body.
- Decreased without diseases of the adrenal cortex: hypertensive states, essential hypertension with low renin activity; Liddle syndrome-pseudohyperaldosteronism; normotensive conditions - parenchymal kidney diseases, autonomic disorders with hypotension.
Sample result (PDF)
Survey objectives
A clinical test for renin is carried out in order to identify the cause of the factors that provoke the development of the following symptoms:
- sudden change in blood pressure;
- excessive amount of renin in plasma;
- Strong headache;
- convulsive syndrome;
- chronic fatigue;
- arrhythmia;
- muscle fatigue;
- stool disorder;
- disturbance of consciousness.
Renin levels and activity are usually determined by mass concentration and RENP.
Pathogenesis
Aldosterone helps to increase the concentration of sodium in the blood plasma by increasing the reabsorption of this ion from primary urine and reducing the potassium content due to the acceleration of its secretion. As a result of sodium retention, the osmotic pressure of the blood increases and the volume of circulating fluid increases. High sodium content leads to sensitization of the vascular wall and the effects of endogenous pressor substances (catecholamines). The result of these pathophysiological changes is an increase in blood pressure.
An increase in the concentration of aldosterone in the blood causes damage to the myocardium, blood vessels and kidneys. In patients suffering from primary hyperaldosteronism for a long time, aldosterone-dependent myocardial hypertrophy is noted. Although left ventricular hypertrophy is considered a nonspecific manifestation of hypertension of any origin, it has been proven that an increase in myocardial mass in PHA develops earlier and is more pronounced.
With PHA, diastolic myocardial function is impaired to a greater extent than with hypertension of other etiologies. Diastolic overload causes left atrium dilatation. With a prolonged increase in aldosterone concentration, fibrotic changes develop in the myocardium. It has been established that after surgical treatment of aldosteroma and normalization of blood pressure, despite a decrease in myocardial hypertrophy, diastolic myocardial dysfunction may persist.
In patients with PHA, along with nonspecific changes observed in any hypertension (like arteriolosclerotic nephrosclerosis), a specific morphological manifestation of the disease is described - the so-called hypokalemic kidney. The morphological substrate of these changes is interstitial inflammation and sclerosis of the interstitium as a result of damage to the tubular epithelium during hypokalemia and metabolic alkalosis. A hypokalemic kidney can cause renoprival hypertension, that is, the formation of secondary hyperaldosteronism.
Preparing to donate blood
For the analysis to show reliable results, the patient must meet several important conditions. You will have to prepare over a long period of time. He will have to stop taking some medications 30 days before the procedure. These include hormonal contraceptives and medications characterized by hypertensive and diuretic effects. Therefore, when selecting a diagnostic regimen, the doctor must take into account those drugs that were previously prescribed. 24 hours before blood collection, the patient is advised to:
- reduce the intensity of physical activity;
- reduce emotional stress;
- forget about alcohol and fatty foods.
Blood is donated on an empty stomach. Allowed to drink water. Coffee, juice and tea are prohibited. The patient can lie or sit. He must first rest for 30 minutes. Preparation is of great importance. The delivery must take place at a medical facility.
Treatment
Drug treatment
To reduce the risk of surgery and anesthesia, preoperative correction of hypertension and water-electrolyte imbalance is necessary. For this purpose, spironolactone, slow calcium channel blockers, and α1-blockers are used. In case of idiopathic aldosteronism or refusal of surgical treatment, the main drug for effective therapy is spironolactone. The remaining groups of antihypertensive drugs do not have any advantage over each other for the correction of arterial hypertension in hyperaldosteronism. It is not always possible to relieve hypertension and hypokalemia with idiopathic aldosteronism using drug therapy. Indications for unilateral adrenalectomy in such cases include resistance of hypertension to combination antihypertensive therapy, the presence of complications during treatment with high doses of drugs or contraindications to therapy (intolerance, allergies, etc.).
Collection process
The level of renin depends on the state of the central nervous system and the drinking regime. A patient referred for this procedure should limit salt intake. The biological material required for the renin test is taken from the renal or peripheral vein. An X-ray machine may be required during collection. The collected blood is first placed in a tube with EDTA, after which laboratory assistants separate the plasma and freeze the biomaterial (temperature is -20 degrees Celsius).
A negative result does not guarantee the absence of pathology. Therefore, the doctor prescribes additional tests. The need for this is due to the fact that the exact cause of the ailment cannot be determined based on only one diagnostic test. The general scheme includes comprehensive studies, ultrasound, MRI, computed tomography and stress tests.
Diagnosis of primary type hyperaldosteronism is carried out by determining the ratio between aldosterone and renin in a direct way. The required indicator is detected by chemiluminescence immunoassay. It is based on the immunological reaction of blood plasma, the occurrence of which is achieved through the use of phosphors. This is the name given to components that produce light when exposed to ultraviolet light. The result is determined by the level of luminescence.
Arterial hypertension in menopausal women
The regulation of a woman’s reproductive system is associated with certain changes in the hypothalamic-pituitary system during various periods of life: before puberty, from puberty to the cessation of menstruation (reproductive period) and pre- and postmenopausal periods. In turn, the hypothalamic-pituitary system is controlled by the cerebral cortex through neurotransmitters, such as dopamine, serotonin, norepinephrine, opioids, etc. This indicates that the harmonious development of a woman’s reproductive system depends on the clear interaction of a number of regulatory factors, such as neuropeptides, liberins, tropic hormones, which implement normal ovarian function in a certain sequence.
Perimenopause is a period of time in a woman's life when ovarian function begins to decline. This process is accompanied by a change in the duration and quality of the menstrual cycle, spanning 1–2 years after menopause. This period is genetically programmed.
At this time, the production of estrogen by the ovaries, in particular estradiol, decreases, and the level of progesterone decreases. In response to hypoestrogen- and hypoprogesteronemia, the cyclic regulation of the menstrual cycle by the hypothalamic-pituitary system is disrupted. During perimenopause, the production of follicle-stimulating hormone (FSH) begins to increase, and in postmenopause, luteinizing hormone (LH), i.e., hypergonadotropic hypogonadism develops.
The pulsatile secretion of gonadotropin is also disrupted over time, which further aggravates the gonadotropic function of the pituitary gland. Neurotransmitters that are components of the reproductive system do not remain intact during perimenopause. The formation of catecholamines in brain tissue increases, dopaminergic, serotonergic, and opioidergic regulation changes.
The developing deficiency of estrogen and progesterone, changes in regulatory mechanisms on the part of the hypothalamic-pituitary system lead to functional disorders of many organs and systems. The involutionary process, being essentially physiological, already in perimenopause can lead to the aggravation of existing or the development of new pathological conditions in the cardiovascular, metabolic, skeletal and other systems of the body, as well as the mental sphere.
One of the serious pathological conditions may be the development or worsening of arterial hypertension (AH). Hypoestrogenemia and a decrease in progesterone production, affecting various mechanisms of regulation of vascular tone, such as aldosterone, atrial natriuretic peptide, disruption of intracellular ionic homeostasis, changes in the activity of adenosine triphosphatase (ATPase), etc., have an adverse effect on the tone and condition of arterioles.
Increased blood pressure (BP) before middle age is more common in men, while after 50 years - in women (R. G. Oganov, 1997; K. Anastos, P. Charney, RA Charon, E. Cohen, CY Jones, C. Marte, D. M. Swiderski, M. E. Wheat, S. Williams, 1991). This age in women coincides with menopause. This fact alone indicates that estrogens and progestins have protective mechanisms that prevent the development of hypertension. Therefore, an important factor is the effect of these hormones on vascular tone, and in particular on endothelial function.
A study of the role of estradiol in vascular relaxation (SA Kharitonov, RB Logan-Sinclair, CM Busset, EA Shinebourne, 1994; JM Sullivan, LP Fowlkes, 1996) showed that the concentration of nitric oxide in the blood of women during the period of ovulation, when peak secretion occurs estrogen levels are increased. Other authors (JM Sullivan, LP Fowlkes, 1996) note an increase in estrogen synthesis of prostacyclin, which, along with nitric oxide, is a powerful vasodilator. By reducing the flow of calcium through calcium channels of smooth muscle cells, estrogens act similarly to calcium channel blockers, causing a vasodilator effect (F. Grodstein, MJ Stampfer, JE Manson, GA Colditz, WC Willett, B. Rosner, FE Speizer, CH Hennekens, 1996).
All these studies confirm the relaxing effect of estrogens on the vascular wall. Their deficiency can lead to vasoconstriction and increased blood pressure.
No less importance in the disturbance of vascular tone is given to a decrease in the secretion of progesterone, which, like estrogens, suppresses the flow of calcium ions through cell membranes (A. N. Karachentsev, P. V. Sergeev, A. I. Matyushin, 1996).
Along with the above, progesterone, by reducing sodium reabsorption in the renal tubules and increasing natriuresis, has an antialdosterone effect (M. Barbagallo, J. Shan, PK Pang, LM Resnick, 1995).
However, the pathogenetic mechanisms of hypertension in postmenopause are not limited to the cessation of the positive effect of ovarian hormones on vascular tone. The fact is that estrogen deficiency is accompanied by the development of relative hyperandrogenism, which promotes or aggravates the development of insulin resistance. The latter, in turn, is accompanied by hyperinsulinemia, dyslipidemia, increased activity of the sympathoadrenal system (SAS), increases sodium reabsorption in the renal tubules, thereby promoting fluid retention, and, along with increased hypertrophy of vascular smooth muscle cells, creates the prerequisites for the development of hypertension.
Insulin resistance and hyperinsulinemia are simultaneously risk factors for the development of obesity and type 2 diabetes mellitus (DM), which contribute to the worsening of hypertension.
In addition to the mentioned pathogenetic features of hypertension during menopause, there is data that suggests the participation of adrenal mineralocorticoids in the pathogenesis of this disease.
It has been shown that during menopause in women with hypertension, the activity of Na-, K-ATPase decreases, the concentration of sodium in erythrocytes increases, and potassium decreases (O. Ylikorkola, A. Orpana, J. Puolakka, T. Pyorala, L. Viinikka, 1995).
Substances that suppress the activity of Na-, K-ATPase are prostaglandin E2, endothelin, which have a vasoconstrictor effect.
Along with electrolyte disturbances, a change in the ratio between renin and aldosterone towards an increase in the latter was shown (IH Zaragh, 1995).
Thus, the possibility of developing primary idiopathic hyperaldosteronism (IHA) during menopause cannot be excluded in these patients with hypertension. This opinion is confirmed by the presence of salt sensitivity in all women with hypertension in menopause (PJ Nestel, PM Clifton, M. Noakes, R. McArthur, PR Howe, 1993) and the development of bilateral small-nodular hyperplasia of the zona fasciculata of the adrenal cortex (V. A. Almazov, E. V. Shlyakhto, 1999).
Summarizing the above, we can identify several links in the pathogenesis of hypertension that arose during the period of postoperative or physiological menopause.
The main pathogenetic link of this disease is a decrease in the production of ovarian hormones - estrogens and progesterone, as well as a compensatory increase in the production of tropic hormones - FSH, LH, accompanied by a violation of the neurotransmitter function of the hypothalamus with increased activity of noradrenergic tone, a decrease in the opioidergic activity of β-endorphins and the activity of the serotonergic system.
A decrease in progesterone and disruption of dopaminergic regulation can cause the development of IHA.
At the same time, relative hyperandrogenism, which is accompanied by the development of insulin resistance leading to metabolic disorders (hyperinsulinemia, dyslipidemia, increased SAS activity, etc.), “contributes” to the pathogenesis of this type of hypertension. As a result of these disorders, type 2 diabetes may develop, in which vascular disorders worsen due to oxidative stress.
Thus, hypertension during menopause, from a pathophysiological point of view, is a complex cascade of metabolic disorders, which subsequently result in organic vascular damage - micro- and macroangiopathy.
Therefore, knowledge of the mechanisms of development of this pathology in women requires a differentiated approach to the treatment of hypertension in order to prevent cardiovascular pathology, such as acute myocardial infarction or stroke.
Based on the complexity of the pathogenesis of hypertension in this category of women, when prescribing antihypertensive therapy, one should take into account risk factors that aggravate this disease: obesity, often of the abdominal type, insulin resistance with hyperinsulinemia, dyslipidemia, water-electrolyte imbalance, left ventricular hypertrophy - even with "mild" hypertension. All these factors provoke the development of cardiovascular complications.
Before prescribing antihypertensive therapy, it is advisable to conduct 24-hour monitoring of blood pressure and an electrocardiogram, as well as determine the patient’s weight in the morning and evening, recording the difference in indicators in order to determine fluid retention; examine blood glucose on an empty stomach and 2 hours after meals, if necessary, glycated hemoglobin (HbA1c), lipids, electrolytes in the blood and daily urine; in case of sodium retention and/or potassium excretion, determine the level of renin in the blood and aldosterone in daily urine.
Based on the results obtained, clarify the main pathogenetic factors that should be targeted for therapy. In any case, it will not be monotherapy and should be selected individually.
It would seem that the main link in the treatment of hypertension in these women should be hormone replacement therapy (HRT). But numerous literature data contain conflicting instructions regarding the prevention of cardiovascular pathology (O. P. Shevchenko, E. A. Praskurnichy, V. A. Zhukova, 2005), while the effect of HRT on blood pressure in postmenopause is still being discussed. And although the decrease in blood pressure when using HRT is insignificant, this therapy should not be neglected in the absence of contraindications.
In this regard, the safest in terms of the lipid spectrum is femoston, which contains dydrogesterone (Duphaston), which does not have androgenic activity.
To prevent thrombosis and embolism, it is recommended to prescribe cardiomagnyl.
It is known that early diagnosis of hypertension and timely initiation of pathogenetically based continuous treatment are the key to successful prevention of cardiovascular complications.
Along with antihypertensive drugs, lifestyle changes are of great importance: regular physical activity of moderate intensity is necessary (walking for 40 minutes every other day or daily at the maximum tolerated speed); the patient should stop smoking, limit alcohol consumption, reduce the calorie intake of foods, especially those rich in quickly digestible carbohydrates and animal fats, and include more foods containing fiber, calcium, potassium, and magnesium in the diet; Limit table salt intake to 5 g per day.
Reducing calorie intake, reducing salt intake, and exercise can lower blood pressure without the use of antihypertensive drugs. Reducing body weight allows you to stabilize your general condition, reducing risk factors for developing cardiovascular complications.
For this purpose, it is advisable to prescribe the drug metformin (Siofor, Glucophage) 500–1000 mg at night to reduce insulin resistance, as well as body weight. This measure is a prevention of the development of diabetes. A positive result in the described situation can be achieved by prescribing the drug meridia, which affects eating behavior through the neurotransmitters of the hypothalamus (norepinephrine and serotonin).
The choice of an antihypertensive drug for the treatment of hypertension in women during menopause depends on its effect on the main pathogenetic links of the clinical syndrome: insulin resistance, increased activity of the SAS, and the development of primary IHA. It is also important that these drugs do not have a negative effect on metabolism.
In the first row are drugs that have a positive effect on microcirculation - these are calcium channel blockers and angiotensin-converting enzyme (ACE) blockers. The points of application of these drugs are different: in the first case, these are vascular smooth muscle cells, where the relaxing effect is caused by increased sensitivity to bradykinin and nitric oxide, in the second - the endothelium, where the formation of angiotensin II is blocked and the vasodilatory activity of bradykinin is increased. Both are vasodilators, reduce insulin resistance, protect the myocardium in coronary heart disease, inhibit atherogenesis, and have a cardioprotective effect against the background of acute myocardial infarction.
Both groups of drugs, through a decrease in insulin resistance, indirectly reduce the activity of the SAS. The most effective way to reduce blood pressure is a combination of two drugs, preferably long-acting, because these drugs maintain the normal daily circadian rhythm of blood pressure and thereby prevent cardiovascular complications. At the same time, when they are used, there is no “replacement” of one risk factor with another; in addition, they are easily combined with other drugs and do not cause an addictive effect.
As for calcium channel blockers, preference should be given to drugs of the dihydropyridine series, which include nifedipine retard, isradipine, amlodipine, adalat SL, etc. The combination of antihypertensive drugs makes it possible to influence a greater number of etiopathological factors, obtaining an adequate effect with lower doses of drugs.
Of the ACE blockers, the most widely used in the treatment of hypertension in menopausal women is Moex (moexipril). The results of the study showed that the drug is metabolically neutral, combined with HRT, without reducing the positive effect of the latter on bone tissue and reducing the activity of osteoblasts (M. Stempel, WSS Jee, Y. Ma et al., 1995).
In case of fluid retention, confirmed by a decrease in sodium excretion in the urine, anti-aldosterone drugs, such as spironolactone, veroshpiron, can be used; in case of increased potassium excretion, potassium-sparing drugs - amiloride. In the absence of increased urinary potassium excretion in postmenopause, the administration of arifon (indapamide), which is successfully combined with ACE inhibitors, may be effective.
Thus, the period of menopause in women often entails the development of various diseases that require careful examination and treatment.
A significant increase in the life expectancy of postmenopausal women and an increase in its quality depend on the prevention of risk factors for the development of diseases such as obesity, type 2 diabetes, hypertension and their complications. The latter include cardiovascular diseases, often leading to disability and death. Therefore, lifestyle changes and complex pathogenetically based therapy, carried out taking into account all clinical syndromes, can help a woman maintain health and continue to lead an active lifestyle during the postmenopausal period.
Z. I. Levitskaya , Candidate of Medical Sciences, Associate Professor of MMA named after. I. M. Sechenova, Moscow