I wonder how a baby feels in the womb? If you take into account only the subjective and emotional feelings of the mother, it is quite difficult to find out the truth. Fortunately, there are special types of examinations that allow you to monitor the development of the fetus, one of them is cardiotocography .
In our clinic you have the opportunity to undergo a full diagnosis and consult with the country's leading specialists, including candidates and doctors of medical sciences, professors. Our expert ultrasound equipment Voluson 10 (only a few clinics can boast of this) is indispensable for diagnosing fetal development, identifying congenital anomalies and malformations (such as heart defects, cleft lip, etc.), early detection of tumors and other serious pathologies.
Modern diagnostics of fetal development includes the following methods:
- Ultrasound examination (ultrasound of the fetus) - helps to see the structure of the child’s organs and body, estimate its approximate weight;
- Doppler ultrasound method - shows the state of fetal blood flow;
- Cardiotocography – allows you to evaluate and record the child’s heartbeat.
1 ultrasound scanner Voluson 10
2 Cardiotocography (CTG)
3 Cardiotocography (CTG)
What is cardiotocography?
This safe and highly effective diagnostic method allows you to assess the condition and development of the fetus by the nature of its heartbeat.
The study takes into account heart rate depending on uterine contractions, fetal activity and exposure to external stimuli. CTG is a mandatory component of comprehensive prenatal screening, along with ultrasound and Doppler sonography of the fetus. The results of the study can seriously affect the management of pregnancy and childbirth itself.
CTG, in addition to heart rate (HR), also records uterine contractions (this is done using a special strain gauge).
Using cardiotocography, you can see signs of oxygen deficiency (hypoxia) of the fetus. Oxygen deficiency is very dangerous because it can lead to delayed fetal development and increases the risk of various disorders during childbirth and the postpartum period.
The study is absolutely safe for a pregnant woman and her child.
Listening to your baby's heartbeat
You can listen to the rhythm and frequency of the embryo’s heartbeat using medical equipment as early as the 3rd week.
- At 6-8 weeks - heart rate varies between 110-130 beats/min.
- From 8 to 11 weeks – indicators reach up to 190 beats/min.
- From 11-12 weeks they remain stably at 140-160 beats/min.
When assessing the baby's heart rate, both the timing of pregnancy and the general condition of the mother are taken into account. After all, all this in its entirety will determine the frequency, intensity of the heartbeat, and the development of the child’s cardiovascular system.
Operating principles of cardiotocography
Features of the study:
CTG is best performed at around 32 weeks. In the earlier stages of pregnancy, it is quite difficult to examine the baby’s heartbeat.
For up to 30 weeks, cardiotocography is used if the doctor cannot find the point at which the fetal heart can be heard. In these cases, the device can be more sensitive and accurate than the human ear.
The recording time is from 30 to 90 minutes, which is associated with periods of sleep and wakefulness of the fetus. CTG is done during the active phase. Data is provided in the form of graphs, which are recorded on paper tape.
Before the examination, the woman needs to rest, get enough sleep, and eat lightly.
Immediately before the procedure, a gel is applied to the working sensor, which enhances the conductivity of impulses.
During labor, CHT is used to examine uterine contractions and the fetal heart rate.
Important! An experienced specialist should analyze the results; only he will be able to distinguish normal from pathology.
At the MedicCity clinic, cardiotocography is performed using modern high-precision ultrasound equipment, which allows the gynecologist to get a clear picture of the condition of the fetus and apply the correct tactics for managing pregnancy and childbirth. In some cases, based on cardiotocography data, the doctor may recommend hospitalization to the woman.
1 Cardiotocography in MedicCity
2 Cardiotocography in MedicCity
3 Cardiotocography in MedicCity
Recommendations for clinical use for obstetricians and gynecologists
Intrapartum fetal heart rate monitoring: terms, description and basic principles of management
This Practice Bulletin was developed by the ACOG Committee on Practice Bulletins in collaboration with George A. Macones, MD. This information is intended for medical practitioners to make decisions when providing obstetric and gynecological care. These recommendations are not binding as the only correct method of treatment or procedure. Their use in practice may be determined by the needs of the individual patient, available resources, and limitations specific to the health care setting or type of clinical practice.
Rice. 1 Fetal monitor Avalon FM20
American College of Obstetricians and Gynecologists (ACOG)
In most recent years for which data are available, approximately 3.4 million fetuses were monitored in the United States (85% of the approximately 4 million live births), making it the most common obstetric procedure. Despite the widespread use of this research method, there is debate about the effectiveness of monitoring the condition of the fetus, the variability of results between different and single researchers, terminology, interpretation systems and control algorithms. Moreover, it is obvious that when using fetal monitoring, the number of deliveries by cesarean section increases compared to vaginal births. The purpose of this document is to review the terminology used to assess fetal heart rate, review evidence on the effectiveness of fetal monitoring, identify the advantages and disadvantages of fetal monitoring, and describe a system for classifying monitoring data.
A combination of factors such as prenatal complications, insufficient blood supply to the uterus, dysfunction of the placenta and complications during childbirth can lead to an unfavorable outcome. Factors such as hypertension, impaired fetal development and premature birth create the preconditions for an unfavorable birth outcome; they are also the cause of a small number of asphyxial injuries. As a result of studies of normal pregnancies with fetal asphyxia, 63% of those studied were not at risk.
The fetal brain controls the heart rate through a combination of impulses from the sympathetic and parasympathetic nervous systems. Therefore, fetal heart rate monitoring can be used to determine the level of oxygen supply to the fetus. In 1980, 45% of pregnant women took part in the study. In 1988 - 62%. In 1992 - 74% and 85% in 2002. Despite the frequent use of fetal monitoring, limitations of this method include poor intra- and inter-observer reliability, uncertain efficacy, and a high false-positive rate.
Fetal heart rate monitoring can be done either invasively or non-invasively. Most monitors use a Doppler device to measure heart rate non-invasively using an automated system for interpreting and counting Doppler signals. Invasive monitoring of fetal heart rate is carried out using special electrodes, which are a spiral-shaped wire that is placed on the fetal skull or other presenting part of the fetus.
Guidance on terminology and interpretation of fetal heart rate monitoring results.
In April 2008, the National Institute of Child Health and Human Development. Eunice Kennedy Schriever, the American College of Obstetricians and Gynecologists and the Society of Maternal-Fetal Medicine organized a conference on automated fetal heart rate monitoring. In 2008, a conference brought together various groups of researchers, both experts and interested individuals, to develop three main objectives:
1) review and update of terminology for the classification of fetal heart rate graphs adopted in previous workshops;
2) evaluate the current classification system for interpreting specific fetal heart rate charts and create recommendations for such systems for use in the United States;
3) creation of recommendations on the main areas of research in the field of monitoring the condition of the fetus.
For a full clinical interpretation of the monitoring results, it is necessary to determine and study uterine contractions, the maximum permissible values and variability of the baseline fetal heart rate curve, the presence of accelerations, periodic or episodic decelerations, as well as changes in these parameters over time. The number of reference conditions and factors used to interpret heart rate in the United States is central to the proposed system of terminology and interpretation. Two of these conditions are the most important. First, the terminology framework was originally developed for the visual assessment of fetal heart rate graphs, but it needs to be compatible with computerized data interpretation systems. Second, the terminology should be suitable not only for intrapartum examinations, but also for prenatal examinations.
Uterine contractions are defined as the number of contractions during 10-minute periods averaged over 30 minutes. Contraction frequency alone is a partial assessment of uterine activity. Other parameters such as contraction duration, intensity, and relaxation time between contractions are also important in clinical practice.
The terminology below is used to describe the activity of the uterus:
- Normal: 5 contractions or less over 10 minutes every 30 minutes.
- Tachycardia: more than 5 contractions within 10 minutes of a 30-minute interval.
Parameters of uterine contraction:
- The terms "hyperstimulation" and "hypercontraction" are not defined and should be excluded from the terminology base.
- Tachycardia is always defined as the presence or absence of deceleration of the corresponding fetal heart rate curve.
- The term "tachycardia" refers to both spontaneous and artificially induced contractions of the uterus. The actions of medical personnel when tachycardia occurs may be different, depending on the type of contraction: spontaneous or stimulated.
Table 1 summarizes the EFM terms and definitions developed in 2008 by the National Institute of Child Health and Human Development Working Group. Deceleration is considered recurrent if it occurs during at least half of the uterine contraction.
Classification of fetal heart rate graphs
Many different systems for interpreting fetal monitoring results are used around the world and in the United States (4–6). Based on a thorough study of existing criteria, it is recommended to use a three-level system to classify fetal heart rate graphs (see table). It is important to understand that fetal heart rate graphs provide information about the current acid-base status of the fetus. The classification of fetal heart rate curves serves to assess the condition of the fetus at a given time; schedules can and will change. Depending on the clinical setting and analysis methods used, fetal heart rate curves may vary between categories.
Category I: Normal fetal heart rate curves. The fetal heart rate graph of category I shows, with a high degree of probability, the normal acid-base state of the fetus at the time of the examination. Category I fetal heart rate graphs can be obtained in a standard manner; no additional steps are required.
Category II: Uncertain fetal heart rate curves. Category II fetal heart rate graphs are not indicators of a violation of the acid-base status of the fetus, and there is still no clear understanding of the classification of such curves as Category I or Category III. Category II fetal heart rate curves should be checked and further monitored and then re-checked, taking into account all clinical conditions. In some cases, when Category II heart rate curves are obtained, it is necessary to perform additional tests to check the condition of the fetus or intrauterine resuscitation measures.
Category III: Abnormal fetal heart rate curves. Category III fetal heart rate charts show the abnormal acid-base status of the fetus at the time of the examination. Category III fetal heart rate curves should be urgently checked. Depending on the clinical setting, actions to correct abnormal fetal heart rate include, but are not limited to, administering supplemental maternal oxygen, changing maternal position, stopping labor, and increasing blood pressure if maternal hypotension occurs. If these methods do not help, then delivery is necessary.
Table 1. Terms and definitions for automated fetal monitoring
| Schedule | Description |
| Base curve |
— Repeated or episodic changes — Periods of significant changes in heart rate — Segments of the curve that differ by more than 25 beats per minute
|
| Fetal heart rate variability |
|
| Acceleration |
|
| Bradycardia at the height of uterine contraction |
|
| Bradycardia at the beginning of uterine contractions |
|
| Bradycardia during umbilical cord contraction |
|
| Long Slowdown |
|
| Sinusoidal rhythm |
|
Three-level fetal heart rate interpretation system
Category I
Category I fetal heart rate curves include all of the following elements:
- Fetal heart rate range: 110 - 160 beats per minute (bpm)
- Fetal heart rate variability: average
- Bradycardia at the height of uterine contraction or during umbilical cord contraction: absent
- Bradycardia at the beginning of uterine contraction: presence or absence
- Accelerations: presence or absence
Category II
Fetal heart rate curves of category II include all graphs of curves that are not included in category I or category II. They represent a significant group that may be encountered in clinical practice. Examples of category II fetal heart rate curves: Initial frequency
- Bradycardia is not accompanied by a lack of change in the baseline curve.
- Tachycardia
Variability in the baseline fetal heart rate curve
- Minimal change to the base curve.
- No change in the base curve is accompanied by periodic slowdowns.
- Noticeable change in the baseline curve.
Acceleration
- Absence of artificially induced heart rate accelerations after fetal stimulation.
Intermittent or episodic slowdowns
- Intermittent bradycardia during umbilical cord contraction is accompanied by minimal or slight change in the baseline curve.
- The period of prolonged deceleration is 2 minutes or longer, but not more than 10 minutes.
- Periodic bradycardia at the height of uterine contraction with a significant change in the baseline curve.
- Bradycardia during umbilical cord contraction is also characterized by other signs, such as a slow return to the baseline curve, "spikes" or "shoulders".
Category III
Category III fetal heart rate curves include:
- No change in the baseline heart rate curve and any of the following:
— Periodic bradycardia at the height of uterine contraction — Periodic bradycardia during umbilical cord contraction — Bradycardia
- Sine curve
Tips for viewing automated fetal heart rate monitoring results
When using a fetal monitor during labor, the nursing staff or doctor should check the readings regularly. If the patient has no complications, then the fetal heart rate curve should be checked approximately once every 30 minutes during the first stage of contractions, and every 25 minutes during the second stage. The appropriate frequency of monitoring for patients with complications (eg, fetal impairment, late-onset toxicosis (preeclampsia)) is every 15 minutes during the first stage of labor and every 5 minutes during the second stage. The medical institution should periodically produce a report that graphic recording of the fetal heart rate was carried out. Fetal heart rate traces, as part of the patient's medical record, should be labeled and available for review as needed. It is advisable to store fetal heart rate curves in digital format in the form of microfilm, without the possibility of re-recording or editing the files.
Clinical conclusions and recommendations
1) How effective is intrapartum automated fetal heart rate monitoring?
The effectiveness of automated fetal monitoring (EFM) during labor is measured by its ability to reduce the risk of complications such as neonatal convulsions, cerebral palsy, or intrapartum fetal death, while reducing the need for obstetric surgery such as vaginal birth or cesarean section. There are no data from randomized clinical trials to compare the benefits of fetal monitoring with other methods of monitoring during labor. Therefore, the benefits of EFM are determined from reports that compare this method with intermittent auscultation.
Based on the results of a meta-analysis combining data from randomized clinical trials aimed at comparing observation methods, the following conclusions were made:
- Fetal monitoring increased the total number of cesarean deliveries (risk ratio [RR], 1.66; 95% confidence interval [CI], 1.30 to 2.13) and cesarean deliveries with abnormal heart rate compared with intermittent auscultation. or acidosis, or both (RR. 2.37; 95% CI, 1.88 - 3.00).
- Use of EFM resulted in an increased risk of using vacuum and forceps during vaginal delivery (RR, 1.16; 95% CI, 1.01 to 1.32).
- EFM did not reduce perinatal death (RR, 0.85; 95% CI, 0.59 to 1.23).
- EFM use was associated with an increased risk of neonatal convulsions (RR, 0.50; 95% CI, 0.31 to 0.80).
- The use of monitoring did not reduce the risk of developing cerebral palsy (RR, 1.74; 95% CI, 0.97 - 3.11).
The expectation that uncertain fetal heart rate curves can predict the development of cerebral palsy is unreasonable. Positive predictive value of indeterminate heart rate curves in determining the presence of cerebral palsy in selected 2,500 g neonates. and more is 0.14%. This means that out of 1,000 fetuses with uncertain heart rate curves, only one or two will have cerebral palsy. The relative number of false positive findings during monitoring to predict the presence of cerebral palsy is extremely high, more than 99%.
Available data, although limited in number, suggest that the use of automated monitoring does not reduce the risk of developing cerebral palsy. Some studies suggest that cerebral palsy does not change over time, despite the widespread use of fetal monitoring. The main explanation for why the prevalence of cerebral palsy has not decreased due to EFM is that 70% of cases occur before the onset of labor; and only 4% of encephalopathy cases can be completely attributed to intrapartum events.
Whereas, the available data do not clearly demonstrate the benefit of observational monitoring (EFM) over intermittent auscultation, even when the EFM technique is used in patients without complications. For technical reasons, it is impossible to provide recommendations here on how often auscultation of the heartbeat should be performed. One prospective study found that auscultation schedule was followed in only 3% of cases. The main reason for the violation of periodic auscultation is the frequency of testing and compliance with all the required conditions for such registration.
The method of intermittent auscultation is not suitable for all pregnant women. Most clinical trials comparing fetal monitoring with intermittent auscultation have excluded participants at high risk for adverse pregnancy outcomes, in which case the relative safety of intermittent auscultation is questionable. When giving birth to women at high risk of complications (for example, potential fetal impairment, late toxicosis and type I diabetes), it is necessary to continuously monitor the patient using a fetal monitor.
There are no comparative data to determine the optimal frequency of intermittent auscultation in the absence of risk factors. The only method is to record and evaluate the fetal heart rate every 15 minutes during the active phase of the first stage of contractions and at least every 5 minutes during the second stage.
2) What is the variability within and between reviewers when assessing the results of intrapartum fetal monitoring?
There is great interobserver and interobserver variability in the interpretation of fetal heart rate curves. For example, when three obstetricians studied 50 cardiotocograms, their opinions coincided only in 22% of cases. Two months later, during a re-examination of the same 50 graphs, doctors interpreted 21% of the curves differently than when they were first assessed. In another study, 5 obstetricians separately interpreted 150 cardiotocograms. Obstetricians identified approximately 29% of cases identically, indicating poor interobserver agreement.
The interpretation of cardiotocograms is most often consistent when normal curves are presented for study. When interpreting curves, a known birth outcome may change the investigator's opinion of the plot. When assessing identical intrapartum curves, the researcher is more inclined to look for signs of fetal hypoxia and criticize the actions of the obstetrician if the birth had an unfavorable outcome. Therefore, repeated interpretation of fetal heart rate curves, especially when the outcome of labor is known, may be unreliable.
3) When should a preterm fetus be monitored?
The decision to monitor such a fetus requires a discussion between the obstetrician, pediatrician, and patient about the likelihood of whether the premature baby will survive or die (depending on gestational age, estimated fetal weight, and other factors), and a decision about the type of delivery must be made. If a patient is undergoing a cesarean section to save a premature baby, continuous monitoring is required rather than periodic listening. The earliest stage of pregnancy at which this procedure can be performed may vary.
Uncertain fetal heart rate curves may appear in up to 60% of women in early labor, with the most common abnormality being slowing and bradycardia, followed by tachycardia and little or no change in the baseline curve. For early births, bradycardia during umbilical cord contraction is more typical (55-70%) than for full-term births (20-30%). If an abnormal heart rate is present, intrauterine resuscitation, additional tests to check the condition of the fetus, and obstetrics in an acceptable manner are required.
4) What medications can affect fetal heart rate?
The fetal heart rate pattern may be affected by medications administered during the intrapartum period. Most often, these changes are temporary, but sometimes they can lead to the need for intervention by an obstetrician.
Epidural analgesia in combination with local anesthetics (eg, lidocaine, bupivacaine) can lead to blockade of the sympathetic nervous system, a decrease in maternal blood pressure, temporary uteroplacental insufficiency and changes in fetal heart rate. Parenteral anesthetics may also affect fetal heart rate. Randomized clinical trials comparing epidural analgesia with 0.25% bupivacaine and intravenous mepiridine showed that waveform variability was reduced and the increase in fetal heart rate was significantly lower with parenteral analgesia than with local analgesia. The degree of deceleration and the number of caesarean sections delivered when obtaining “unsatisfactory” fetal heart rate curves were similar for both groups. A systematic study of randomized and observational clinical trials also found that the rate of caesarean section deliveries resulting in “unsatisfactory” fetal heart rate curves was the same for patients who did and did not receive epidural analgesia during labor.
The question of the effect of joint spinal-epidurial analgesia during labor has aroused interest. In an intention-to-treat analysis, 1,223 parturients were randomly assigned to receive spinal epidural analgesia (10 µg sufentanil injected into the spinal cavity, followed by epidural bupivacaine, followed by fentanyl) or intravenous mepiridine (50 mg on demand, maximum 200 mg). mg per 4 hours) revealed that significantly more cases of bradycardia and emergency cesarean section due to abnormal fetal heart rate were observed in the group selected for spinal epidural anesthesia. However, the birth outcome was not significantly different between the two groups. There are some methodological inaccuracies in this study. Another randomized controlled trial compared the occurrence of abnormal changes in fetal heart rate during labor in women receiving combined spinal epidural anesthesia (n=41) and epidural anesthesia (n=46). In this study, abnormal changes in fetal heart rate were most often observed in the spinal epidural anesthesia group. Additional studies are needed to determine the safety and effectiveness of spinal epidural anesthesia.
Other drugs that affect fetal heart rate have also been studied (see Table 2). It should be noted that the comprehensive inverse analysis showing a decrease in variability due to the use of magnesium sulfate relates only to early pregnancy and not to changes in magnesium sulfur levels. Research results show different effects of magnesium on the fetal heart rate curve. Some studies show no significant effect; others note small changes in the baseline fetal heart rate curve. However, the reported adverse effects on fetal monitoring should be avoided when using magnesium alone.
A transient sinusoidal heart rate pattern occurred in 75% of patients given butorphanol during labor and was not associated with a risk of adverse outcome. When the fetus was exposed to cocaine, there were no characteristic changes in the heart rate curve, despite the fact that frequent uterine contractions occurred without artificial stimulation. As a result of computer analysis of cardiotocograms and a randomized clinical trial comparing the effects of mepiridine and nalbuphine for intrapartum anesthesia, it was found that there was a decrease in the likelihood of two 15-second accelerations within a 20-minute interval. In the prenatal period, the use of morphine leads to a slowdown in the fetal respiratory movements and a decrease in the number of accelerations in its heart rate.
The effect of corticosteroids used to increase fetal lung maturity during early labor on heart rate has been studied (see Table 2). Among twins and only children, betamethasone use temporarily reduced heart rate variability, which returned to baseline after four to seven days. The use of betamethasone may also lead to a decrease in the number of fetal heart rate accelerations. These changes were not associated with obstetric surgery or risk of adverse outcome. The biological mechanism of this phenomenon is not known. Computer analysis of cardiotocograms shows that the use of betamethasone does not affect the variability of fetal heart rate.
5) What indicators of fetal monitoring correspond to the normal acid-base balance of the body?
The presence of increases in heart rate indicates that there is no change in the acid-base state of the fetus. Data regarding the impact of fetal heart rate variability on birth outcomes are sparse. Results from an observational study indicate that small changes in fetal heart rate are inextricably linked to umbilical cord pH levels greater than 7.15. One study showed that during bradycardia at the height of uterine contraction or umbilical cord contraction, the umbilical cord pH will be above 7.00 in 97% of cases, provided that the fetal heart rate curves are characterized by normal variability. In another retrospective study, normal variation in fetal heart rate was observed in most cases with an unfavorable birth outcome. These studies are limited because they do not take into account other parameters of the heart rate curve, such as the presence of accelerations or decelerations. However, in most cases, a normal change in fetal heart rate confirms optimal fetal health and the absence of metabolic acidemia.
How is CHT performed?
To obtain accurate data during cardiotocography, a woman must be in the correct position: half-sitting or lying on her left side. If the expectant mother lies on her right side, the uterus may press on the inferior vena cava, which will lead to complications.
Before starting the examination, the doctor listens to the pregnant woman’s belly with a stethoscope and finds the point where the baby’s heartbeat can best be heard. It depends on how the baby turned in the womb. It is best to perform CTG within 2-3 hours after the patient has eaten. To avoid obtaining erroneous data, cardiotocography should not be done earlier than an hour after intravenous administration of glucose to the expectant mother.
How to listen to the fetal heartbeat at home
Future parents can monitor how the fetal heart beats at home, without resorting to the help of doctors and complex equipment. In practice, there are several ways to do this at home.
- First of all, get a stethoscope - this is what is available to everyone today; it can be easily purchased at any pharmacy. But the main thing to remember here is that you can listen to the heartbeat with such a device no earlier than the 25th week of pregnancy.
- Fetal Doppler is a special detector that responds to the fetal heartbeat, working on the principle of ultrasound. Listening headphones are often included with a special sensor - with its help you can distinguish the beats of a small heart from 8-12 weeks.
- And, probably, the easiest and most accessible way for everyone to hear the baby’s heartbeat is to simply put your ear to the pregnant woman’s belly. In this case, the heartbeat can be distinguished no earlier than 29-30 weeks of pregnancy.
If, while using this or that method of listening to the fetal heartbeat at home, certain results confuse you, it is best to seek help from a doctor.
In what cases is CTG performed?
Cardiotocography is performed to identify pathologies of fetal development at an early stage of pregnancy. The study is carried out in the following cases:
- with unfavorable pregnancies in the past (miscarriages, frozen pregnancies, various chromosomal pathologies in the fetus);
- with gestosis in a pregnant woman (this disease can lead to impaired blood supply to the fetus);
- in case of Rh conflict;
- with high or low water;
- if the expectant mother has chronic diseases (overweight, hypertension, diabetes, heart disease, kidney disease, liver disease);
- changes in the rhythms of fetal behavior (if the child was very active during the day and suddenly calmed down, then perhaps the fetus is experiencing some kind of discomfort);
- in post-term pregnancy;
- if a woman does not stop smoking or drinking alcohol during pregnancy;
- if a pregnant woman falls ill with ARVI, influenza or other acute diseases.
1 ultrasound scanner Voluson 10
2 Cardiotocography (CTG)
3 Cardiotocography (CTG)
Listening to a baby's heartbeat in a medical facility
- Ultrasound is the first of many methods for listening to the frequency and intensity of fetal SB. Allows you to assess not only SB, but also the general condition of the fetus and placenta.
- Auscultation is listening to the heartbeat using a stethoscope. Allows you to listen to the baby’s heartbeat from 28-29 weeks. It is important to remember that in some cases this diagnostic method is not possible. For example, with a large weight of the pregnant woman herself, a small/large amount of amniotic fluid, and so on.
- Cardiotocography, or CTG for short, is an informative, modern method. The method works on the principle of ultrasound equipment, when with the help of special sensors it is possible to accurately determine the frequency and intensity of the fetal heartbeat, uterine contractions and other necessary physiological indicators.
- Echocardiography is used at 18-28 weeks of pregnancy - it is used to diagnose the general condition of the blood flow and the structure of the child’s cardiovascular system. It is prescribed if a woman has previously given birth to children with heart defects, or if she herself has a history of heart muscle defects. It is also indicated in cases where the mother has suffered an infectious disease during pregnancy, and if the woman in labor was 38 years or older at the time of pregnancy and has been diagnosed with diabetes.
All these methods for diagnosing and listening to fetal SB are used in medical institutions. But parents can hear their child’s heartbeat at home, without visiting a medical facility.
What problems are diagnosed using cardiotocography?
Cardiotocography is an additional examination method. Therefore, it is impossible to make an accurate diagnosis based only on its results. However, with the help of CTG it is possible to detect the development of various fetal pathologies, including the following disorders:
- heart rhythm disturbance;
- hypoxia;
- pressing or entwining the umbilical cord.
If CTG reveals abnormalities in the condition of the fetus, additional ultrasound and Doppler sonography are performed.
Electronic fetal monitoring
This is an advanced technique with which serious complications are determined: cerebral palsy, intrauterine death, cardiac dysfunction. Fetal monitoring is carried out as follows: the woman in labor, lying on her back, has belts with sensors placed on her stomach. One device records the fetal heartbeat, and the second - the duration and intensity of uterine contractions. Sensors are connected to the monitor.
In some cases (for example, serious danger to the fetus), an internal examination is used. Its essence is as follows: the electrode is inserted through the cervix and placed on the baby’s head. With such an examination, the doctor receives the exact data necessary to assess the current situation. Internal monitoring is used after rupture of membranes. The cervix should also be dilated (at least 1 cm).
External electronic monitoring lasts about half an hour. Innovative devices are used in clinics. For example, these could be Avalon fetal monitors. This is technological equipment with the best characteristics. It is distinguished by functionality, long service life, and ease of use.
Fetal monitoring is an advanced technology used in medical institutions equipped with the latest technology. Therefore, we need to take a closer look at its features and advantages.
Prevention and treatment of fetal bradycardia
Women with chronic diseases of the cardiovascular, endocrine, digestive systems, obesity, and mental disorders are prone to bradycardia. Risk factors also include:
- Constant emotional stress - for example, due to stressful work, an unhealthy family environment (including physical and sexual abuse);
- Physical discomfort - in particular, regular heavy lifting, playing sports, working or living in a highly toxic environment, eating disorders;
Treatment of this disease depends on its intensity, the risk to the health of the mother and fetus, and the causes of its occurrence. The main goal of therapy is to eliminate the provoking factor, reducing the danger for the woman and the unborn child:
- For mild bradycardia, the doctor prescribes preventive measures - walks in the fresh air, low-intensity physical exercise, taking mineral and vitamin complexes, dietary nutrition, etc. In this case, the expectant mother does not remain in hospital for treatment, but only undergoes regular examinations.
- Severe bradycardia can lead to pregnancy loss, so the patient is admitted to a hospital inpatient care. The doctor prescribes treatment for the underlying maternal disease causing the pathology, and at the same time stimulates placental blood flow to reduce or eliminate fetal hypoxia. However, even if these problems are resolved, the woman remains under observation until the end of the pregnancy. Usually in such cases a caesarean section is prescribed, since the child may simply not survive a natural birth.
Early detection of fetal bradycardia is the key to successful treatment of this disease. Therefore, all pregnant women, even if they are not at risk and do not have visible symptoms of pathology, are recommended to regularly visit an obstetrician-gynecologist and undergo medical examinations.
Diagnosis of bradycardia in the fetus
If the mother herself has no problems identifying heart rhythm disturbances, then in the case of fetal bradycardia the situation is more complicated. Pathology can only be detected by observing the fetus itself. The following methods are used for this:
- Auscultation. This is listening to the fetal heartbeat using a stethoscope. It is carried out externally through the mother's abdominal wall. This is the simplest, but also the least reliable method of diagnosis, since the readings are influenced by the presence of a woman’s fat layer, as well as the motor activity of the fetus.
- Ultrasound. Ultrasound examination allows not only to hear the fetal heartbeat, but also to visualize the embryo itself. Ultrasound can be performed abdominally (through the peritoneum) or transvaginally (with a probe inserted into the vagina). In this case, the doctor receives data on the nature and intensity of the fetal motor activity, the frequency of its breathing and heart contractions.
- CTG (cardiotocography). This is one of the most accurate ways to diagnose bradycardia in the fetus in later stages. It consists of recording the embryo's pulse and comparing it with the frequency of contractions of the mother's uterus. The assessment occurs on a 10-point scale: with 8-10 points, no pathology is detected, with 6-8, a mild anomaly is diagnosed, and with less than 6 points, a severe form is diagnosed. The advantage of CTG is the possibility of using this method if the mother has endocrine and cardiovascular disorders.
- ECG (electrocardiography). This method involves recording electrical impulses from the fetal heart, often in combination with recording heart sounds (phonocardiography). The received data is displayed in real time in the form of a cardiogram - linear graphs on paper tape. Bradycardia is indicated by the presence of a P wave and increased T-P and T-Q intervals.
Depending on the severity of the disease, some of these tests are performed or they are used in combination. The doctor gives a referral to undergo them, focusing on the mother’s condition, her age, whether she had similar problems in previous pregnancies, etc.
Take the first step
make an appointment with a doctor!
Ultrasound of the fetal heart in the II-III trimesters of pregnancy
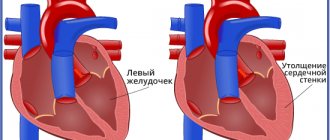
In the second and third trimesters, during an ultrasound, not only the heart rate is studied, but also the detailed structure and location of the heart to exclude its congenital malformations.
In the II-III trimesters of pregnancy during ultrasound:
- the location of the heart in the chest is examined (the heart is located on the left and occupies approximately 1/3 of the chest during a transverse scan),
- heart rate (normal - 140-160 beats per minute),
- the nature of the contractions (rhythmic or non-rhythmic).
Heart rate in the later stages depends on many factors (fetal movements, physical activity of the mother, exposure to various factors on the mother: heat, cold, various diseases).
With a lack of oxygen, the heart rate first compensatory increases above 160 beats per minute (this condition is called tachycardia), and then, as the fetal condition worsens, it becomes below 120 beats per minute (bradycardia).
To identify cardiac malformations, a so-called “four-chamber slice” is examined. This is an ultrasound image of the heart in which you can see all four chambers of the heart at the same time - two atria and two ventricles. A conventional four-chamber ultrasound of the heart can detect approximately 75% of heart defects. According to indications, an additional study is performed - echocardiography of the fetus.