Furosemide is a prescription drug that is available at an affordable price. It is an effective diuretic. The drug belongs to the group of loop diuretics. These drugs remove fluid from the body, affecting the filtration ability of the kidneys. Due to the presence of contraindications and the high risk of adverse reactions, the drug should be taken only as prescribed by a doctor.
Furosemide: components and release form
The drug is produced in three forms. The active ingredient in them is furosemide. The most common are round or flat-cylindrical, white or slightly yellowish tablets. They have a chamfer and a risk. Furosemide tablets, the instructions indicate this, contain, in addition to 40 mg of the active ingredient of the same name, auxiliary components: corn and potato starch, cellulose, lactose, etc.
The tablets are placed in blister packaging, for the production of which polyvinyl chloride film and aluminum foil are used. You can also purchase them in plastic polymer jars. In any form, the tablet product, together with instructions for use, is packaged in cardboard boxes.
In addition, you can purchase the drug in other forms:
- In ampoules of 2 ml. They contain 20 mg of active substance. The drug is administered intravenously in cases where it is not possible to use tablets. For example, the need for this may arise in urgent situations. Sometimes intramuscular administration is prescribed, but the effectiveness of the drug decreases.
- In granules for preparing a suspension. This form is used to treat children.
Indications
Furosemide, the instructions focus on this, is prescribed primarily to relieve edema that occurs against the background of the following pathologies:
- Heart and kidney failure.
- Nephrotic syndrome.
- Liver pathologies.
- Arterial hypertension.
- Hypertensive crisis.
Furosemide is also indicated for burns; the instructions for use indicate this. The medicine is prescribed if severe toxicosis occurs in the second and third trimester of pregnancy. It is very often accompanied by swelling and other severe symptoms.
Contraindications
It is important to know what furosemide is used for, and to understand what contraindications exist. This will avoid dangerous consequences when using it. It is advisable to consult a doctor before starting to use furosemide; the instructions for use of the tablets emphasize many conditions where caution is necessary. In particular, these are:
- Anuria. With its development, pathological changes in the organs of the urinary system lead to the fact that urine does not enter the bladder.
- Oliguria. This pathology is characterized by a decrease in daily urine production for various reasons.
- Glomerulonephritis. This serious kidney disease is associated with damage to the glomeruli, often due to infection.
- Hyperuricemia. This pathology is characterized by an increased concentration of uric acid in the blood.
You should stop using the drug if you are hypersensitive to the active substance. The drug is not prescribed in the first trimester of pregnancy, since the active substance crosses the placenta. The drug should also be discontinued during lactation, as it suppresses the production of breast milk.
There are also a large number of relative contraindications. In particular, these are diabetes mellitus, low blood pressure, pancreatitis, diarrhea, etc. There are other contraindications that are indicated in the instructions for use.
Material and methods
A study of the effectiveness and safety of combinations of antihypertensive drugs was carried out in the emergency department of polyclinic No. 17 - the clinical base of the department of emergency medical care of Northwestern State Medical University named after. I.I. Mechnikov.
The study included patients who applied for emergency medical care due to increased blood pressure without the development of hypertension and patients with uncomplicated hypertension.
The study did not include patients under 18 years of age, patients with life-threatening emergencies, patients with contraindications to any of the 4 medications used, and patients who, before the arrival of the EMS team, took any medications that affect blood pressure.
The study used moxonidine (Physiotens, Abbott), furosemide (Lasix, Aventis, Sanofi), captopril (Capoten, Akrihinn), nifedipine (Cardoflex, Egis).
The effectiveness and safety of combinations of 0.4 mg moxonidine with 10 mg nifedipine were compared; 0.4 mg moxonidine with 40 mg furosemide; 25 mg captopril with 10 mg nifedipine; 25 mg captopril with 40 mg furosemide.
Combinations of drugs were prescribed using a table
Table 1. Characteristics of patients Note: AH—arterial hypertension, HF—heart failure, AMI—acute myocardial infarction, ACVA—acute cerebrovascular accident. random numbers.
A total of 389 patients were included in the study. The vast majority of patients were women (78%). Average age: 70.4±0.6 years. Duration A.G. — 21.5±0.5 years. Initial systolic blood pressure (SBP) was 197.4±0.9 mmHg, diastolic blood pressure (DBP) was 107.5±0.6 mmHg.
Depending on the prescribed combinations of antihypertensive drugs, patients were divided into four groups. The characteristics of patients in the groups are presented in Table. 1.
As can be seen from table. 1, there were no significant differences between the groups for all of the listed characteristics. Blood pressure was measured using the Korotkoff method. In each case, measurements were carried out 2 times, taking into account the minimum values. Registration of A.D. were carried out before prescribing medications and after taking medications every 10 minutes during the first 30 minutes of the study, and longer if indicated.
A reduction in blood pressure of no less than 15%, but no more than 25% of the initial value was considered effective and safe, subject to complete disappearance or significant reduction in the severity of complaints [9, 10].
For the primary assessment of the effectiveness of self-help, we compared the annual number of calls for emergency medical services due to increased blood pressure before patients received self-help recommendations and one year after these recommendations were received. To do this, we conducted a continuous sample of emergency medical service call cards for 500 patients with increased blood pressure. Due to the fact that information about 2 patients was incomplete, these cards were excluded from further processing.
Statistical processing of the results was carried out using the application package Statistica for Windows 8.0.550. Checking the empirical law of distribution of variables showed agreement with the theoretical law of normal distribution according to Shapiro-Wilks ( p
>0.05), therefore, to describe numerical characteristics and quantitative characteristics, the arithmetic mean and the mean square error of the mean were used.
P
was taken as the threshold level of statistical significance [11].
Side effects
Side effects when taking the drug can be observed from various systems. The most common disorder of the digestive system is manifested by:
- Dry mouth.
- The occurrence of a strong feeling of thirst
- Nausea and vomiting.
- Diarrhea or constipation.
Dangerous side reactions are allergic reactions. Failures of the cardiovascular system also pose a threat to health. In rare cases, temporary disturbances in vision and hearing are noted during treatment. Headaches, dizziness, and muscle weakness may also occur. In case of any negative reactions, the drug should be discontinued.
First aid kit for hypertension: drugs for hypertensive crisis
Home — For the public
- Map of medical organizations
- Vaccination
- Clinical examination
- Fluorography
- Addresses and opening hours of clinics
- Emergency rooms
- Oncology
- Where to take an HIV test
- Healthy child's office
- Services
- Prevention of CVD
- Disease Prevention
- World Patient Safety Day
- Newspaper "Medical News"
- specialist
- School of Health
— Disease prevention
- HIV infection
- All about vaccination
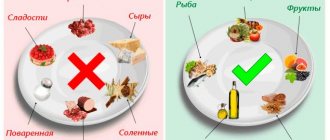
- All about proper nutrition
- Hepatitis
- Flu
- Dementia
- Schoolchildren's health
- STD
- Tick-borne encephalitis
- Whooping cough
- Measles
- Legionellosis
- Meningococcal infection
- Oncology
- Acute intestinal infection
- Pediculosis
- First aid
- Pneumococcal infection
- Pneumonia
- Prevention of rabies
- Dependency Prevention
- Rotavirus infection
- Diabetes
- Cardiovascular diseases
- Injuries
- Tuberculosis
- Tularemia
- Physical activity
- Obstructive pulmonary disease
- Exotic infections
- Ecology
- Why is swimming in ponds dangerous?
— Cardiovascular diseases — First aid kit for hypertension
People suffering from high blood pressure have a high risk of developing complications such as heart attack, stroke and other dangerous diseases. In order to provide the necessary assistance in a timely manner if the condition worsens, you must have a first aid kit with the necessary medications. What should such a first aid kit contain?
1.
Medicines prescribed by a doctor
Treatment of patients with arterial hypertension is individual. Therefore, you must always carry with you the medications prescribed by your doctor. Remember that medications should always be taken at the same time of day. Do not stop taking medications if your blood pressure levels become normal.
2. Symptomatic
remedies (they alleviate the condition of a sick person)
People with arterial hypertension often suffer from symptoms such as headache, spots before the eyes, weakness, sleep disturbances, psycho-emotional disorders (anxiety, irritability, etc.). Therefore, your first aid kit should contain products that alleviate these symptoms:
- Sedatives for various manifestations of psycho-emotional disorders (valerian, motherwort, etc.).
Please note that these medications can cause side effects, so do not overuse them. Better yet, consult your doctor in advance.
3. Means for stopping a crisis
A crisis is an acute sharp increase in blood pressure. It is often accompanied by a sharp headache, severe weakness, confusion, nausea and vomiting. It is against the background of a crisis that conditions such as acute coronary syndrome and acute myocardial infarction, transient ischemic attacks, ischemic and hemorrhagic strokes arise. Therefore, the home medicine cabinet of a hypertensive patient should contain drugs that stop the crisis, for example:
- captopril taken under the tongue (usually 12.5-25 mg; effect within 10-20 minutes)
- Moxonidine is taken under the tongue (0.2-0.4 mg, effect within 10-20 minutes)
IMPORTANT: A specific drug to relieve a hypertensive crisis or a rise in blood pressure must be prescribed to you by your attending physician, taking into account existing contraindications and concomitant diseases!
Don't forget that our lives are unpredictable, so it's better to always be alert and have everything you need for this.
Dosage according to instructions
The dosage of the drug for the treatment of various pathologies is selected individually. It is recommended to use the minimum doses of the drug that allow you to achieve the desired result. The tablets are swallowed on an empty stomach. When taking them, you need to drink enough water.
According to the instructions, the maximum daily dose for adult patients is 1500 mg. The amount of medication to be taken by a specialist is determined based on an analysis of the body’s diuretic response. When treating edematous syndrome, which is provoked by various pathologies, the initial dose is 20-80 mg/day. It is divided into 2-3 doses. Subsequently it can be increased. For patients on hemodialysis, the dosage may be increased to 1500 mg/day.
The daily dosage for the treatment of children is 1-2 mg/kg body weight. If necessary, the amount of the drug can be increased to 6 mg/kg, but the medicine should be taken at intervals of at least 6 hours. The duration of treatment depends on the indications. It must be agreed with the doctor.
The effectiveness of the drug may change when interacting with other drugs. This must be taken into account when using it. Overdose is also dangerous. It can provoke negative reactions in the body that pose a threat to life.
Furosemide
Combinations not recommended
— Chloral hydrate
- Intravenous infusion of furosemide within a 24-hour period after administration of chloral hydrate may lead to skin flushing, profuse sweating, anxiety, nausea, increased blood pressure and tachycardia. Therefore, the use of furosemide in combination with chloral hydrate is not recommended.
— Aminoglycosides
- slowing down the excretion of aminoglycosides by the kidneys when used simultaneously with furosemide and increasing the risk of developing ototoxic and nephrotoxic effects of aminoglycosides. For this reason, the use of this combination of drugs should be avoided, except in cases where it is necessary for health reasons, in which case an adjustment (reduction) of maintenance doses of aminoglycosides is required.
Combinations that should be used with caution
— Ototoxic drugs
- furosemide potentiates their ototoxicity. Such drugs can be used simultaneously with Furosemide only for strict medical indications, since combined use can lead to irreversible damage to the hearing organ.
— Cisplatin
- when used simultaneously with furosemide, there is a risk of ototoxicity. In addition, the nephrotoxic effect of cisplatin may be enhanced when furosemide is used for forced diuresis during treatment with cisplatin, unless furosemide is used in a low dose (for example, 40 mg in patients with normal renal function) and without combination with appropriate hydration of the patient.
— Sucralfate
- a decrease in the absorption of furosemide when taken orally and a weakening of its effect (furosemide and sucralfate when taken orally should be taken at least two hours apart).
— Lithium salts -
under the influence of furosemide, the excretion of lithium is reduced, due to which the content of lithium in the blood serum increases, which increases the risk of its toxic effects, including cardiotoxic and neurotoxic effects. Therefore, when using this combination, monitoring of lithium levels in the blood serum is required.
-
(ACE)
inhibitors - the use of ACE inhibitors or angiotensin II receptor antagonists in patients previously treated with furosemide may lead to an excessive decrease in blood pressure with deterioration of renal function, and in some cases - to the development of acute renal disease insufficiency, therefore, 3 days before starting treatment or increasing the dose of ACE inhibitors or angiotensin II receptor antagonists, it is recommended to discontinue furosemide or reduce its dose.
— Risperidone
- Caution should be exercised, carefully weighing the balance of risk and benefit, before deciding to use a combination of risperidone with furosemide or other strong diuretics, as an increase in mortality was observed in elderly patients with dementia receiving concomitant treatment with risperidone and furosemide.
— Levothyroxine
- Furosemide in high doses can inhibit the binding of thyroid hormones to carrier proteins and thus lead initially to a transient increase in the concentrations of free thyroid hormones, and then, in general, to a decrease in the total concentration of thyroid hormones. When using this combination, thyroid hormone concentrations should be monitored.
Interactions to Consider
— Nonsteroidal anti-inflammatory drugs ( NSAIDs)
- NSAIDs, including acetylsalicylic acid, can reduce the diuretic effect of furosemide. In patients with hypovolemia and dehydration (including while taking Furosemide), NSAIDs can cause the development of acute renal failure. Furosemide may increase the toxicity of salicylates.
— Phenytoin
- reduction of the diuretic effect of furosemide.
— Glucocorticosteroids, carbenoxolone, licorice preparations
in large quantities and prolonged use of laxatives when combined with furosemide increase the risk of developing hypokalemia.
— Cardiac glycosides, drugs known to prolong the QT interval
- in case of development of water-electrolyte balance disturbances (hypokalemia or hypomagnesemia) during the use of furosemide, the toxic effect of cardiac glycosides and drugs increases. causing prolongation of the QT interval (the risk of developing heart rhythm disturbances increases).
- Antihypertensives, diuretics or other drugs
that can lower blood pressure
- when combined with furosemide, a more pronounced decrease in blood pressure is possible.
- Probenecid, methotrexate or other drugs that, like furosemide,
are excreted in the renal tubules
, can reduce the effects of furosemide (same route of renal excretion); on the other hand, furosemide may lead to decreased renal excretion of these drugs. All this increases the risk of developing HP both with furosemide and the above-mentioned medications taken simultaneously with it.
— Hypoglycemic agents (both for oral administration and insulin preparations), pressor amines (epinephrine, norepinephrine)
- weakening of effects when combined with furosemide.
— Theophylline, diazoxide, curare-like muscle relaxants
- enhanced effects when combined with furosemide.
— Medicines with nephrotoxic effects
- when combined with furosemide, the risk of developing nephrotoxicity increases.
- High doses of some cephalosporins (excreted primarily by the kidneys)
- in combination with furosemide, the risk of nephrotoxicity of cephalosporins increases.
— Cyclosporine A
- when combined with furosemide, the risk of developing gouty arthritis increases due to hyperuricemia caused by furosemide and impaired renal urate excretion under the influence of cyclosporine.
— X-ray contrast agents —
Patients at high risk of developing nephropathy due to radiocontrast administration treated with furosemide had a higher incidence of renal dysfunction after administration of radiocontrast agents, compared with patients at high risk of developing nephropathy due to radiocontrast administration who received only intravenous fluids (hydration).