Chronic venous insufficiency and pregnancy
Pregnancy is a wonderful, joyful and natural state.
However, pregnancy does not always go smoothly. Hormonal changes in this period of life have a positive effect on a woman’s body, protecting it during this difficult period, but the same hormones can significantly complicate the work of other organs and systems. Connective tissue undergoes the greatest changes. This can cause various problems: pain in the lower back and joints, the appearance of “stretch marks” on the skin of the chest and abdomen, flat feet. In addition, 50% of women develop either dilated skin capillaries or varicose veins during their first pregnancy. With repeated pregnancies, this percentage increases, and the risk of thrombotic complications also increases sharply. Nature made sure that during childbirth the mother did not lose a lot of blood. To do this, during pregnancy, under the influence of hormones, the blood becomes thicker. Blood thickening, as well as venous congestion, significantly increase the risk of blood clots forming in the veins. For an expectant mother, this risk is 3-5 times higher than for a non-pregnant mother. The formation of blood clots in the veins can cause a serious and sometimes fatal complication - pulmonary embolism, which threatens not only the health, but also the life of the mother and the unborn child. The high risk of thrombosis remains and is even especially dangerous within 6 weeks after birth, especially after a cesarean section or major blood loss during childbirth. Thus, pregnancy is actually a thrombogenic condition. This means that normal changes that occur in the body during physiological pregnancy increase the likelihood of deep vein thrombosis.
These changes are:
- Significant slowing of blood flow in the deep veins of the legs due to increased blood outflow from the placental part of the uterus with overload of the iliac veins;
- Decreased tone of the vein walls and their physiological expansion, which leads to natural valve insufficiency and reverse blood flow;
- Increase in pressure in the veins of the lower extremities by 2-3 times;
- Increased production of sex hormones progesterone and relaxin, which directly affect elastic fibers and reduce the tone of vascular smooth muscles;
- Significant increase in the concentration of blood clotting factors;
- Decreased fibrinolytic (dissolution of clots or thrombi) ability of blood at the end of pregnancy and in the first stage of labor;
- Receipt of active substances into the blood after separation of the placenta
Difficulty in venous outflow from the lower extremities during pregnancy is caused by a cascade of five mechanisms:
— Mechanical factor. An enlarged uterus is an obstacle to circulation, as it compresses the inferior vena cava, pressing it against the spinal column and the iliacus muscle.
— Circulatory factor. An increase in blood volume and blood flow from the heart leads to an increase in the load on the veins and their expansion. This is especially important for the veins of the lower extremities and the vaginal area.
— Hormonal factors. Progesterone, due to its relaxing effect on smooth muscle fibers, leads not only to a decrease in the tone of the venous wall, but also to a decrease in the tone of the urethra, bladder and small intestine.
— Hemostatic factors. Changes in the hemostatic system always occur in the direction of increasing coagulability (increased fibrinogen levels, increased platelet activity and decreased fibrinolytic activity).
— Hemorheological factors. Blood viscosity increases despite a decrease in hematocrit
— Other contributing factors. These factors include a strong family history, a sedentary lifestyle, prolonged sitting while working, driving, too high or thin heels, obesity, hot baths, multiple pregnancies or short intervals between them.
The danger increases from the 5th month of the first pregnancy and increases significantly with each subsequent one. The triggering factor is the hormonal changes that occur in the pregnant woman’s body: the release of large quantities of female sex hormones, in particular, the hormones of the corpus luteum. In addition, the pregnant uterus grows and gradually puts more and more pressure on the large veins located in the pelvis and abdominal cavity, creating obstacles to the outflow of venous blood from the lower extremities. As a result, venous blood stagnates and pressure increases in the veins of the legs and pelvis.
During pregnancy, a woman's body undergoes many changes. The hormone progesterone, which is responsible for the preservation and development of the fetus, affects not only the uterus, but also the veins and their smooth muscle cells, which reduces their tone. The influence of progesterone begins from the first days of conception and fetal development. High levels of the hormone lead to the development of degenerative changes in elastic and collagen fibers, as a result of which the veins become less elastic and dilate. The process proceeds more quickly if the hormonal balance was disturbed even before pregnancy, and also if the woman took hormonal drugs or oral contraceptives.
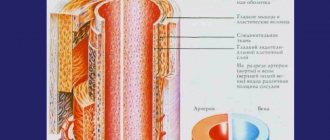
The development of varicose veins during pregnancy occurs as a result of many factors. An increase in the volume of circulating blood leads to an increase in pressure on the vessels. Because of this, veins suffer, since their wall has lower density and elasticity compared to arteries.
The increase in the size of the uterus puts pressure on the veins of the pelvis, which leads to a delay in the outflow of blood from the legs to the upper region. For this reason, varicose veins of the lower extremities occur. Increased pressure on the vessels of the lower extremities due to the constant weight gain of a pregnant woman. The most affected veins are the saphenous veins, which are not surrounded by muscle, compared to the deep veins. They are most often subject to varicose veins, since their wall is not surrounded by an outer layer of muscle.
Medicines
The most effective and preferred method of treating pathological changes in the veins in the groin is drug therapy. It can not only protect a woman from possible complications, but also eliminate the unpleasant symptoms characteristic of varicose veins.
The basis of this therapeutic method is the use of venotonic and venoprotective drugs aimed at restoring the natural functions of smooth muscle fibers, through the work of which the necessary narrowing of the lumen in the veins is achieved, and also relieves local inflammatory processes and their consequences. Taking medications of this pharmacological group is acceptable starting from the second trimester. Phlebologists widely use oral medications based on diosmin and troxerutin, herbal components, namely:
- Detralex
- Antistax
- Phlebodia 600
- Troxerutin
- Ginkor-Forte
- Venarus
Note! Pregnancy is not the time for experiments! Therefore, any medications, including over-the-counter ones, can be taken only after the approval of a doctor.
After a blood test, if elevated coagulation rates are detected, the doctor prescribes antiplatelet drugs for a pregnant woman at any stage. They prevent platelets from sticking together and, as a result, improve blood circulation, nutrition of the placenta and prevent blood clots. The most famous representative of this pharmaceutical group is Curantil. This product is safe for the fetus because it does not penetrate the placental barrier.
In addition, special multivitamin complexes may be prescribed: Elevit, Vitrum Prenatal, Pregnavit, Alphabet Mom's Health, Complivit Mom and others.
There are the following forms of varicose veins in pregnant women:
- Varicose veins of the lower extremities
- Varicose veins of the pelvis
- Varicose veins of the external genitalia
- Pelvic venous congestion syndrome
- Right ovarian vein syndrome
- Varicose veins of the ovarian veins (varicoovarium)
Currently, there are 2 variants of the course of varicose veins of the small pelvis: varicose veins of the perineum and vulva, as well as pelvic venous congestion syndrome. It should be emphasized that this division is quite arbitrary, since in more than 50% of cases, varicose veins of the perineum and vulva provoke a violation of the outflow from the pelvis, and vice versa.
Varicose veins of the perineum and vulva
Occurs in 30% of women during pregnancy. The mechanisms of this condition are basically similar to those of varicose veins of the lower extremities. At the same time, the progressive varicose transformation of the perineal veins is aggravated by compression of the main veins of the retroperitoneal space (iliac and inferior vena cava) by the pregnant uterus. Outside of pregnancy, it persists in 2-10% of cases.
Pelvic Congestion Syndrome
The variety of clinical manifestations and imperfect diagnostics disguise it as various forms of gynecological (inflammatory diseases of the uterus and its appendages, endometriosis), urological (cystitis), surgical (colitis, Crohn's disease, etc.) and even orthopedic (diseases of the hip joint) pathology.
This disease is associated with varicose veins of the venous plexuses of the ovaries and the broad ligament of the uterus. The main mechanism is valvular insufficiency of the ovarian veins, leading to the discharge of blood and increased pressure in the venous plexuses of the pelvis. Predisposing factors may be uterine retroflexion, leading to bending of the broad ligament of the uterus, which impedes the outflow of venous blood, as well as various gynecological diseases (endometriosis, tumors of the uterus and ovaries). In recent years, the adverse effects of hormonal therapy and contraception have been discussed. The influence of hormonal levels is evidenced by the fact that the manifestations of pelvic venous congestion syndrome in the postmenopausal period become less pronounced.
The clinical picture of the disease is quite characteristic and manifests itself as varicose veins of the perineum, vulva, vagina, and lower extremities progressing as the pregnancy period increases (cosmetic defect). Signs of such violations will be:
- Itching in the area of dilated veins.
- A feeling of heaviness and bursting pain in the perineum, pelvis, swelling of the external genitalia, lower extremities.
- Dyspareunia (pain during sexual intercourse)
- Dysmenorrhea
- Severe premenstrual syndrome
- Pain when walking and exercising
- Pain along the veins
- General pain and aches in the legs
- Dysuric disorders.
- Fatigue.
- The development of acute varicothrombophlebitis and rupture of altered veins, which is accompanied by massive bleeding.
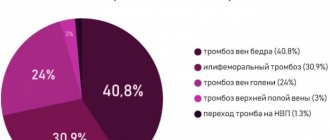
Thrombosis during pregnancy is the most important clinical problem. This is due to the high frequency of this condition as a cause of maternal mortality (20% of all causes). As is known, during pregnancy there is a tenfold increase in the risk of thrombosis. The incidence of thrombosis is 0.7 - 4.2/1000 in pregnant women versus 1/10,000 in non-pregnant women of childbearing age.
The critical stage of the thrombotic process is pulmonary embolism - a severe and very often fatal complication of thrombosis. PE is the leading cause of maternal mortality in Western obstetric practice - 0.7 cases per 1000 births (from 11% to 27%). The likelihood of venous thromboembolic complications (VTE) during cesarean section is 3-6 times higher. The risk of developing VTE returns to the level typical for non-pregnant women 6 weeks after birth.
The main WTO risk factors include the following:
- Age (> 35 years)
- C-section
- Weight > 80 kg
- Personal and family history of thrombosis
- Repeated births
- Ovarian hyperstimulation
- Prolonged immobilization
- Varicose veins
- Thrombophilia
The difficulty of treating HTO during pregnancy is as follows:
- Direct dependence on the duration of pregnancy (safe periods of pregnancy for active treatment tactics 7-8 weeks, 13-17 weeks, 23-27 weeks)
- Difficulty in selecting the type and dosage of an anticoagulant
- High probability of miscarriage and/or complications
- The need to resolve the complex issue of choosing treatment tactics
- The ethical problem of choosing to preserve life
- The problem of achieving compliance with the patient and her relatives
As for varicose veins of the lower extremities during pregnancy, this problem is very extensive and controversial. Patients with varicose veins who are planning a pregnancy should be clearly aware of the risks, adequately assess the danger that the disease poses not only to the mother, but also to the unborn child, so as not to then place all responsibility on doctors, who in this case will have very limited possibilities. Such responsibility, first of all, should lie with the parents of the unborn child. Experts always insist that varicose veins be cured before pregnancy, then there will be no corresponding risk.
On the one hand, the presence of varicose veins is the main risk factor for the occurrence of VTO, i.e. there is a strict need to prevent such complications - surgical treatment. On the other hand, during pregnancy, the possibilities of surgical treatment are sharply limited by the safe periods of pregnancy. And if before pregnancy the patient has a fairly large choice in treatment methods, then if complications of varicose veins occur during pregnancy, for example thrombophlebitis, the only possible method of removing the veins will be a standard operation, and this means general anesthesia and the need to prescribe medications, which is a direct threat to the fetus, and in addition, severe surgical trauma, causing certain changes in the body that are clearly not beneficial to the pregnant woman and the fetus. In this case, modern low-traumatic methods of surgical treatment - EVLO and RFO - will have a clear advantage, because they do not require the use of general anesthesia and the prescription of a significant amount of medication, and also do not cause significant surgical trauma and are safe. However, in this case, given the constant growth of the pregnant uterus and progressive changes in venous circulation with a sharp increase in pressure in the veins, the likelihood of a relapse of the disease is very high. An important factor will be certain conditions and technical capabilities for performing such an intervention.
Therefore, if a patient with varicose veins seeks help during pregnancy, in most cases conservative methods of prevention are still prescribed, as a rule - compression therapy, taking phlebotropic drugs during safe periods of pregnancy, dynamic observation with an objective assessment of the condition. In the absence of complications during pregnancy, surgical treatment is prescribed after the period of breastfeeding. However, the high risk of VTO with varicose veins in pregnant women remains, even with compression therapy, especially in the presence of several risk factors, which we mentioned above.
For example, the standard for preventing VTO in Europe in the presence of several risk factors for thrombosis, in the presence of varicose veins, is to prescribe daily injections of drugs that “thin” the blood for the ENTIRE period of pregnancy! Is it really worth not having your varicose veins operated on before pregnancy, using modern methods, quickly, painlessly, and then being absolutely calm both for yourself and for your unborn child?!
So, the main measure to prevent the development of VTO in the presence of varicose veins is timely and adequate treatment (timely surgical treatment, compliance with compression therapy, correction of the rheological properties of blood and blood coagulation processes, active lifestyle).
On the small lips
Along with the labia majora, the pathological process can also affect the labia minora. However, they do not swell as often. The clinical picture does not change. In the initial stages, the disease does not cause much discomfort and is asymptomatic, causing only visual defects. However, over time, symptoms characteristic of venous insufficiency appear, which were mentioned above.
Having discovered any changes at the entrance to the vagina, you should see a gynecologist , who will resolve the issue with further examination and refer you for a consultation to a specialized specialist.
The main simple preventive measures are the following:
- Wear comfortable underwear;
- Limit physical activity, while performing simple exercises to keep fit, swimming
- Monitor your diet by adding more fiber to your diet
- Sufficient amount of liquid
- Walking in loose shoes, heels no more than 4 cm, comfortable, non-tight clothing
- Do not take hot baths, do not visit the bathhouse, sauna
- Daily ascending contrast shower
- Active motor mode, avoid prolonged stationary positions, walking for 2 hours
- Perform special venous exercises
- Watch your weight
- Sleep on your left side
- Wear compression stockings
- See a phlebologist
Considering all of the above, our advice for pregnant women with varicose veins:
- Wear compression stockings at all times throughout your pregnancy.
- maintain an active motor mode;
- see a phlebologist throughout pregnancy;
- strictly follow all recommendations of the specialist;
- If the first signs of deterioration occur, seek help immediately.
If you are planning a pregnancy and have varicose veins, have them operated on before pregnancy and protect yourself and your unborn child.
The article was prepared by a vascular surgeon of the highest category, phlebologist Vladimir Vladimirovich Gerasimov.
For information about treatment and to make an appointment, call contact: 044 495 2 888 or 097 495 2 888
Consultation with a phlebologist Prevention of varicose veins
On big lips
Enlargement of the labia during pregnancy is evidence of the development of pathology. Due to the localization of the process, a woman is not always able to examine the manifested swollen vessels in a timely manner. Most often they are detected during independent palpation or at an appointment with a gynecologist, during an examination on a gynecological chair.
Symptoms characteristic of the disease can also alert the expectant mother:
- The appearance of single or multiple swollen venous nodes, vascular networks or asterisks.
- Swelling of the genital organs, changes in their shape, color of the mucous membrane.
- Feeling of dryness in the genital area, burning sensation.
- Uncomfortable or painful sensations after prolonged sitting, sexual intercourse, defecation or urination.
The appearance of any of these signs is a reason to think about your own health and the health of your baby, and go to the hospital for qualified help.
Read other materials about varicose veins during pregnancy in our section.
How to measure your foot correctly
The size of the knitwear is selected individually, according to the patient’s anatomical measurements. Measurements are taken in the morning, since during the day swelling may appear on the legs and the measurements will not be correct. If selected incorrectly, products of a smaller size will cause discomfort, while larger ones will not have the desired effect.
4 measurements:
- Ankle circumference (b) - Measure your ankle, the narrowest part of your leg.
- We measure the circumference of the shin under the knee joint (d).
- Thigh circumference (g) - 5 cm below the groin.
- Length of the leg from the foot to point (g) - for stockings and tights or to point (d) for golf.
For each type of product, certain parameters are measured and then compared with a size selection table. Do not forget that each manufacturer has its own table and you should strictly adhere to this selection rule! If you are afraid that you will take measurements in the wrong place, then trust the professionals. At the Ortix orthopedic salon, they will take the necessary measurements and select the product according to size.
What are varicose veins?
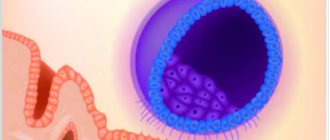
Varicose veins are a condition in which blood accumulates under the vein valves. The veins become swollen and immune cells attack the walls of the distended veins, causing inflammation. The stretched walls of the vessels allow elements of blood and plasma to pass into the subcutaneous tissue, and the leg begins to look characteristic of the disease.
Diagnostics
Diagnosis of the disease is simple; preventive examinations should be carried out for early detection of the disease.
To make a diagnosis, the doctor must:
- carefully collect anamnesis of life and illness;
- examine the external and internal genitalia;
- palpate enlarged nodes;
- conduct an ultrasound examination to confirm the diagnosis and exclude other pathologies;
- order general laboratory tests.
After making a diagnosis, you should determine the cause and decide on the treatment of varicose veins of the intimate organs.