Potassium is the main intracellular macronutrient. About 90% of all potassium ions in the body are located inside cells. Such a large difference between intra- and extracellular concentrations is necessary to maintain the membrane potential of cells, their ability to excite and transmit nerve impulses. Accurate data on the overall prevalence of hypokalemia are not available. It is only known that it is detected in 3-20% of patients undergoing hospital treatment. This disorder is somewhat more often observed in patients of cardiology and gastroenterology departments.
Hypokalemia
The normal concentration of potassium in blood plasma is 3.5–5.5 mmol per liter.
The form of electrolyte imbalance in which the level of this element is less than the lower limit of normal is called hypokalemia. Potassium ions are found in the blood, brain, heart, kidneys, liver, muscles and bone tissue. Potassium is involved in the physiological processes of the body - the functioning of the heart, metabolic reactions, muscle contraction, and the conduction of nerve impulses. Potassium ions activate enzymes located inside cells, increase the tone of smooth muscles, participate in the regulation of intercellular contacts, maintain normal blood pressure and stable kidney function, ensure constant acid-base balance, and much more. Accordingly, a deficiency (as well as an excess) of this important element leads to the development of a number of serious disorders in almost all organs and systems of the body.
Pathogenesis
Hypokalemia leads to hyperpolarization of cell membranes, as a result of which the threshold for the occurrence of an action potential increases (up to its complete blocking), which impairs the excitability of neurons and myocytes. The transmission of nerve impulses in neuromuscular synapses and the conduction system of the heart is disrupted. The tone of skeletal muscles, smooth muscle walls of blood vessels, and internal organs decreases. This causes most of the symptoms.
Motility of the gastrointestinal tract slows down. The sensitivity of arterioles to the vasoconstrictor effect of angiotensin II decreases. Hypokalemia contributes to the appearance of ventricular ectopic rhythms in the heart and impairment of the concentrating ability of the kidneys (increased excretion of water). The secretion of insulin in the pancreas and aldosterone in the adrenal glands is suppressed.
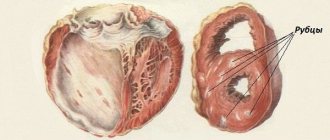
Depletion of K+ reserves leads to the accumulation of hydrogen in the cell and intracellular acidosis. As a result, the processes of tissue respiration and glycolysis are suppressed. A pathological examination reveals dystrophic changes in almost all internal organs (especially the heart, kidneys, and liver).
Causes of hypokalemia
A relative physiological cause of the development of potassium deficiency is considered to be insufficient intake of the macronutrient from food, which is often observed in people who follow strict diets or have a poor diet.
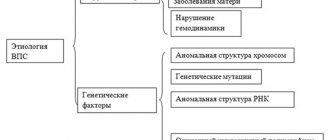
Pathological hypokalemia in children and adults occurs for various reasons:
- Gastrointestinal problems. The electrolyte balance is disrupted by various gastrointestinal pathologies, including profuse diarrhea or prolonged vomiting.
- Excessive intake of potassium into cells. Against the background of some pathologies occurring in the body, there is a movement of potassium ions from the intercellular space into the cells. This is possible with an excess of catecholamines, metabolic alkalosis (a shift in pH levels to the alkaline side), the use of large doses of insulin in patients with diabetic ketoacidosis, alcohol abuse, familial periodic paralysis, and an overdose of certain vitamins (for example, folic acid).
- Impaired renal tubular function. Due to this pathology, potassium transport is disrupted and its excretion increases. This is possible with renal acidosis, renal artery stenosis, Barter syndrome, interstitial nephritis.
- Hyperaldosteronism. The excretion of potassium ions by the kidneys stimulates aldosterone. The condition when the adrenal cortex secretes large amounts of aldosterone is called hyperaldosteronism. It can be primary, arising from an aldosterone-producing adrenal tumor, and secondary, caused by a renin-secreting tumor, chronic renal failure or renovascular hypertension due to occlusion of the renal artery.
- Endocrine disorders. Hypokalemia often develops with congenital dysfunction of the adrenal cortex, Itsenko-Cushing syndrome, and thyrotoxicosis.
- Treatment with certain medications. Most often, potassium deficiency occurs while taking thiazide and loop diuretics. Other drugs that can cause hypokalemia are bronchodilators, beta-agonists, some antibiotics (especially penicillins), tocolytics, theophylline, etc.
Other possible causes: use of a nasogastric tube, extensive burns, hypomagnesemia, hypernatremia, cirrhosis of the liver, lymphoblastic leukemia, diabetes insipidus.
Prognosis and prevention
Hypokalemia is a serious pathology that can be fatal without timely treatment. The most common cause of death is arrhythmias (PVT, VF). Less commonly, patients die from diaphragmatic paralysis or acute renal failure due to massive rhabdomyolysis. Prevention comes down to treating diseases that cause a decrease in the level of K+ in the blood, adding potassium-berger diuretics to regular diuretics, and consuming foods rich in potassium (bananas, dried fruits, vegetables).
Symptoms of hypokalemia
The development of hypokalemia is accompanied by rapid fatigue, muscle weakness (especially in the lower extremities), and sometimes muscle cramps.
If the concentration of potassium ions decreases to 3.0 mmol/l and below, the following are added to the described symptoms:
- neurological and mental disorders - paresthesia, irritability, deterioration of concentration, apathy, etc.;
- functional myocardial failure, heart rhythm disturbances (people receiving cardiac glycosides have a high risk of developing life-threatening arrhythmia);
- gastrointestinal pathologies - nausea, vomiting, constipation, heaviness in the epigastric region, dynamic intestinal obstruction.
Severe acute hypokalemia leads to the development of ascending paralysis affecting the diaphragm and intercostal muscles, which requires the patient to be connected to a ventilator.
Salt metabolism disorder
General information
Water-salt metabolism is a set of processes of the entry of water and salts (electrolytes) into the body, their absorption, distribution in internal environments and excretion from the body.
A person's daily water consumption is about 2.5 liters, of which he receives about 1 liter from food. In the human body, 2/3 of the total amount of water is intracellular fluid and 1/3 is extracellular. Part of the extracellular water is in the vascular bed (about 5% of body weight), while most of the extracellular water is outside the vascular bed, this is interstitial (interstitial) or tissue fluid (about 15% of body weight). In addition, a distinction is made between free water and water retained by colloids in the form of so-called swelling water, i.e. bound water, and constitutional (intramolecular) water, which is part of the molecules of proteins, fats and carbohydrates and is released during their oxidation. Different tissues are characterized by different ratios of free, bound and constitutional water. During the day, the kidneys excrete 1-1.4 liters of water, the intestines - about 0.2 liters; with sweat and evaporation through the skin, a person loses about 0.5 liters, with exhaled air - about 0.4 liters.
Systems for regulating water-salt metabolism ensure that the total concentration of electrolytes (sodium, potassium, calcium, magnesium) and the ionic composition of intracellular and extracellular fluid are maintained at the same level. In human blood plasma, the concentration of ions is maintained with a high degree of constancy and is (in mmol/l): sodium - 130-156, potassium - 3.4-5.3, calcium - 2.3-2.75 (including ionized, not associated with proteins - 1.13), magnesium - 0.7-1.2, chlorine - 97-108. Compared to blood plasma and intercellular fluid, cells have a higher content of potassium, magnesium, phosphate ions and a low concentration of sodium, calcium, chlorine and bicarbonate ions. Differences in the salt composition of blood plasma and tissue fluid are due to the low permeability of the capillary wall for proteins.
Precise regulation of water-salt metabolism in a healthy person makes it possible to maintain not only a constant composition, but also a constant volume of body fluids, maintaining almost the same concentration of osmotically active substances and acid-base balance. Regulation of water-salt metabolism is carried out with the participation of several physiological systems. Signals coming from special imprecise receptors that respond to changes in the concentration of osmotically active substances, ions and fluid volume are transmitted to the central nervous system, after which the release of water and salts from the body and their consumption by the body changes accordingly.
With an increase in the concentration of electrolytes and a decrease in the volume of circulating fluid (hypovolemia), a feeling of thirst appears, and with an increase in the volume of circulating fluid (hypervolemia), it decreases. An increase in the volume of circulating fluid due to increased water content in the blood (hydremia) can be compensatory, occurring after massive blood loss.
Hydremia is one of the mechanisms for restoring the correspondence of the volume of circulating fluid to the capacity of the vascular bed. Pathological hydremia is a consequence of impaired water-salt metabolism, for example, in renal failure, etc.
A healthy person may develop short-term physiological hydremia after taking large amounts of liquid. The excretion of water and electrolyte ions by the kidneys is controlled by the nervous system and a number of hormones. Physiologically active substances produced in the kidney - derivatives of vitamin D3, renin, kinins, etc. - also participate in the regulation of water-salt metabolism. The sodium content in the body is regulated mainly by the kidneys under the control of the central nervous system through specific natrioreceptors. responding to changes in sodium content in body fluids, as well as volume receptors and osmoreceptors, responding to changes in the volume of circulating fluid and osmotic pressure of extracellular fluid, respectively. The sodium balance in the body is also controlled by the renin-angiotensin system, aldosterone, and natriuretic factors.
With a decrease in water content in the body and an increase in the osmotic pressure of the blood, the secretion of vasopressin (antidiuretic hormone) increases, which causes an increase in the reabsorption of water in the renal tubules. An increase in sodium retention by the kidneys causes aldosterone, and an increase in sodium excretion: natriuretic hormones, or natriuretic factors. These include atriopeptides, synthesized in the atria and having a diuretic, natriuretic effect, as well as some prostaglandins.
Causes of salt metabolism disorders
The causes of disorders can be different, most often the following factors negatively affect salt metabolism:
- sedentary lifestyle;
- hormonal changes;
- excess nutrition;
- abundant consumption of meat, spicy dishes and legumes;
- alcohol abuse;
- smoking;
- hypothermia of the body.
The main manifestation of salt metabolism disorders is joint diseases: limited mobility in them, crunching and crackling, pain at rest and during movement, deformation, bone growths.
- disturbances of water-salt metabolism are manifested:
- accumulation of fluid in the body;
- the appearance of edema/fluid deficiency;
- decrease/increase in blood osmotic pressure;
- electrolyte imbalance;
- decrease/increase in the concentration of individual ions;
- change in acid-base state.
Knowledge of pathological conditions in which the ionic composition of the blood plasma or the concentration of individual ions in it changes is important for the differential diagnosis of various diseases. Deficiency of water and electrolyte ions, mainly Na+, K+ and Cl- ions, occurs when the body loses fluids containing electrolytes. A negative sodium balance develops when sodium excretion exceeds intake for a long time. The loss of sodium leading to pathology can be extrarenal and renal.
Extrarenal sodium loss occurs primarily through the gastrointestinal tract with the following manifestations:
- vomit;
- intestinal obstruction;
- pancreatitis;
- peritonitis;
- burns.
Most gastrointestinal juices are nearly isotonic with blood plasma, so if replacement of fluid lost through the gastrointestinal tract is carried out correctly, changes in extracellular fluid osmolality are usually not observed. However, if the fluid lost during vomiting or diarrhea is replaced with an isotonic glucose solution, a hypotonic state develops and, as a concomitant phenomenon, a decrease in the concentration of K+ ions in the intracellular fluid.
The most common loss of sodium through the skin occurs during burns. The loss of water in this case is relatively higher than the loss of sodium, which leads to the development of heterosmolality of extracellular and intracellular fluids with a subsequent decrease in their volumes. The kidneys are capable of excreting more sodium than is necessary to maintain a constant water-salt metabolism when the mechanisms regulating sodium reabsorption in the renal tubules are impaired or when sodium transport into the cells of the renal tubules is inhibited.
Significant renal loss of sodium in healthy kidneys can occur with an increase in diuresis of endogenous or exogenous origin, incl. with insufficient synthesis of mineralocorticoids by the adrenal glands or administration of diuretics. When renal function is impaired (for example, in chronic renal failure), the body loses sodium mainly due to impaired reabsorption in the renal tubules. The most important signs of sodium deficiency are circulatory disorders. Water deficiency with a relatively small loss of electrolytes occurs due to increased sweating when the body overheats or during heavy physical work. Water is lost during prolonged hyperventilation of the lungs, after taking diuretics that do not have a saluretic effect. Restoring the amount of water and isotonicity of the fluid in case of pathological dehydration of the body is achieved by drinking large amounts of drinking water or intravenously administering an isotonic solution of sodium chloride and glucose. The loss of water and sodium due to increased sweating is compensated by drinking salted (0.5% sodium chloride solution) water. Excess water and electrolytes manifests itself in the form of edema. The main reasons for their occurrence include excess sodium in the intravascular and interstitial spaces, more often with kidney disease, chronic liver failure, and increased permeability of the vascular walls. In heart failure, excess sodium in the body may exceed excess water. The disturbed water-electrolyte balance is restored by limiting sodium in the diet and prescribing natriuretic diuretics. Excess water in the body with a relative deficiency of electrolytes (the so-called water poisoning, or water intoxication, hypoosmolar hyperhydria) is formed when a large amount of fresh water or glucose solution is introduced into the body with insufficient fluid secretion; excess water can also enter the body in the form of hypoosmotic fluid during hemodialysis.
With water poisoning , hyponatremia and hypokalemia develop, and the volume of extracellular fluid increases. Clinically, this is manifested by nausea and vomiting, which worsens after drinking fresh water, and vomiting does not bring relief; visible mucous membranes in patients are highly moist. Hydration of the cellular structures of the brain is manifested by drowsiness, headache, muscle twitching, and convulsions. In severe cases of water poisoning, pulmonary edema, ascites, and hydrothorax develop. Water intoxication can be eliminated by intravenous administration of hypertonic sodium chloride solution and sharp limitation of water consumption. Potassium deficiency is mainly a consequence of its insufficient intake from food and loss through vomiting, prolonged gastric lavage, and profuse diarrhea. Loss of potassium in diseases of the gastrointestinal tract, such as:
- esophageal tumors;
- stomach tumor;
- intestinal obstruction;
- fistulas
It is associated to a large extent with hypochloremia developing in these diseases, in which the total amount of potassium excreted in the urine increases sharply. Patients suffering from repeated bleeding of any etiology lose significant amounts of potassium.
Potassium deficiency occurs in patients treated for a long time with corticosteroids, cardiac glycosides, diuretics and laxatives. Potassium losses are high during operations on the stomach and small intestine.
In the postoperative period, hypokalemia is more often observed with the infusion of isotonic sodium chloride solution, because Na+ ions are antagonists of K+ ions. The release of K+ ions from cells into the extracellular fluid increases sharply, followed by their excretion through the kidneys with increased protein breakdown; a significant deficiency of potassium develops in diseases and pathological conditions accompanied by impaired tissue trophism and cachexia (extensive burns, peritonitis, empyema, malignant tumors). Potassium deficiency in the body does not have specific clinical signs.
Hypokalemia is accompanied by the following symptoms:
- drowsiness;
- apathy;
- disorders of nervous and muscle excitability;
- decreased muscle strength and reflexes;
- hypotonia of striated and smooth muscles (atony of the intestine, bladder).
It is important to assess the degree of decrease in potassium content in tissues and cells by determining its amount in the material obtained from muscle biopsy, determining the concentration of potassium in erythrocytes, and the level of its excretion in daily urine, because hypokalemia does not reflect the full extent of potassium deficiency in the body. Hypokalemia has relatively clear manifestations on the ECG (decrease in the Q-T interval, lengthening of the Q-T segment and T wave, flattening of the T wave).
Hyperkalemia
Potassium deficiency is compensated by introducing potassium-rich foods into the diet. These may be the following products:
- dried apricots;
- prunes;
- raisin;
- natural juices.
If a potassium-enriched diet is insufficient, potassium is prescribed orally in the form of potassium chloride, panangin (asparkam), intravenous infusions of potassium preparations (in the absence of anuria or oliguria). With rapid loss of potassium, its replacement should be carried out at a rate close to the rate of removal of K+ ions from the body. The main symptoms of potassium overdose: arterial hypotension against the background of bradycardia, increased and sharpened T wave on the ECG, extrasystole. In these cases, the administration of potassium preparations is stopped and calcium preparations, a physiological potassium antagonist, diuretics, and fluids are prescribed. Hyperkalemia develops when there is a violation of the excretion of potassium by the kidneys (for example, with anuria of any origin), severe hypercortisolism, after adrenalectomy, with traumatic toxicosis, extensive burns of the skin and other tissues, massive hemolysis (including after massive blood transfusions), as well as with increased breakdown of proteins, for example, during hypoxia, ketoacidotic coma, diabetes mellitus, etc. Clinically, hyperkalemia, especially with its rapid development, which is of great importance, manifests itself as a characteristic syndrome, although the severity of individual symptoms depends on the genesis of hyperkalemia and the severity of the underlying disease.
The following symptoms are noted:
- drowsiness;
- confusion;
- pain in the muscles of the limbs;
- stomach ache;
- characteristic pain of the tongue.
Flaccid muscle paralysis is observed, incl. paresis of intestinal smooth muscles, decreased blood pressure, bradycardia, cardiac conduction and rhythm disorders, muffled heart sounds. In the diastole phase, cardiac arrest may occur . Treatment of hyperkalemia consists of a diet limited in potassium-rich foods and intravenous sodium bicarbonate; intravenous administration of a 20% or 40% glucose solution with simultaneous administration of insulin and calcium preparations is indicated. is most effective for hyperkalemia . Sodium is the main cation in plasma and extracellular fluid and largely determines their osmotic pressure. It is excreted mainly in urine. Aldosterone enhances sodium reabsorption in the distal tubules of the kidneys. True hyponatremia is observed with kidney disease and overdose of diuretics, as well as with:
- diarrhea;
- vomiting;
- adrenal insufficiency.
In these cases, a lack of sodium in tissues and tissue fluid is also revealed. A different situation is observed in patients with the development of ascites, before treatment with natriuretics. In such cases, hyponatremia does not reflect the true sodium balance, since it accumulates in large quantities in tissue fluid. The intravenous administration of large amounts of sodium to such patients is dangerous due to the possibility of developing pulmonary edema. Successful treatment of ascites often leads to the disappearance of hyponatremia in these patients. Hyponatremia is observed in a number of patients with acute alcoholic hepatitis, much less often in patients with acute viral hepatitis. Hyponatremia is common in end-stage liver disease. A significant decrease in sodium concentrations in tissue fluid can cause serious damage to hepatocytes. Potassium plays an important role in metabolic processes. The potassium content in the blood serum is regulated primarily by hormones. Hypokalemia is often observed with advanced cirrhosis, as well as with malignant liver tumors . Severe hypokalemia contributes to the development of encephalopathy in patients with severe liver damage. This form of encephalopathy was called Calc's false coma.
Hypercalcemia
Calcium plays an important role in the metabolism of bone and connective tissue. Hypercalcemia is observed in a number of liver diseases that occur with jaundice. Severe calcium metabolism disorders leading to osteoporosis are detected in primary and secondary biliary cirrhosis of the liver.
Hypocalcemia is observed in fulminant viral hepatitis, especially in cases of concomitant pancreatitis and hypoalbuminemia. Hypomagnesemia occurs in severe chronic (especially alcoholic) liver diseases and can contribute to the development of encephalopathy. Along with this, it was noted that cleansing enemas with magnesium sulfate in some patients with hepatic encephalopathy caused the development of hypermagnesemia.
Diagnosis of hypokalemia
Arrhythmic pulse and muscle hypotension are the main symptoms that suggest hypokalemia. To confirm the diagnosis, the following examinations are prescribed:
- Lab tests. A study of the acid-base state of the blood, determination of the content of potassium, magnesium, calcium, sodium, urea and creatinine is required. Urine is examined for the presence of chlorine and its density is determined.
- Hormonal spectrum. A number of hormone tests are performed, including cortisol and aldosterone.
- Electrocardiography (ECG). With hypokalemia, the patient exhibits prolongation of the QT interval and the appearance of a U wave, and sometimes ventricular tachycardia or atrial fibrillation.
Additionally, if necessary, ultrasound, CT, MRI, echocardiography, angiography are performed.
Differential diagnosis is carried out with hyperkalemia, myasthenia gravis, muscular dystrophy, Guillain-Barré syndrome.
How to compensate for potassium deficiency
Pharmaceuticals offers a variety of pharmaceutical drugs, for example: Asparkam, Potassium Orotate, Panangin, Normin at an affordable price to replenish the reserves of an important macronutrient. Replenishing the body means normalizing nutrition, which is important for women during pregnancy with hypokalemia.
The macronutrient is found in large quantities in the following products:
- porridge (oatmeal, buckwheat, barley),
- bananas,
- dried fruits,
- nuts,
- pumpkin,
- melons,
- watermelons,
- mushrooms,
- meat,
- freshly squeezed carrot juice,
- apples,
- celery,
- sprouted wheat grains.
Patients with hypokalemia should avoid consuming strong coffee, sweets, and alcohol. It is recommended to steam dishes made from foods high in potassium in the oven for the purpose. However, during treatment and prevention, one should not overdo it and forget that an excess of potassium is just as harmful as its lack. May cause increased stress on the kidneys.
If patients have to take long-term courses of laxatives and diuretics, then it may be worth discussing with their doctor the selection of a replacement for potassium-sparing diuretics. It is important for athletes to consume foods containing natural minerals every day.
Hypokalemia: treatment
The main goal of therapy is to stop the body losing potassium. To do this, it is necessary to eliminate the cause of hypokalemia. At the same time, the deficiency is corrected.
Treatment of hypokalemia with potassium supplements is mandatory. For mild pathological processes, medications are usually prescribed in tablet form, for example, Asparkam or Panangin. In severe cases, intravenous solutions containing potassium chloride or potassium bicarbonate are required. However, intravenous infusions are contraindicated in patients whose problem is caused by impaired potassium redistribution (with the exception of familial hypokalemic periodic paralysis), since the risk of developing rebound hyperkalemia is high.
In some cases, the use of antiarrhythmic drugs - propafenone or amiodarone - is required to eliminate arrhythmia. In case of ventricular fibrillation, defibrillation is necessary.
Popular questions about hypokalemia
What is hypokalemia?
This is a condition characterized by a decrease in plasma potassium concentration below 3.5 mmol/l.
What does low potassium in the blood mean?
The reason may be different - from insufficient intake of macronutrients from food to dysfunction of the adrenal cortex. To install it, you need to conduct a detailed examination.
How to determine the lack of potassium in the body?
There are no specific symptoms of deficiency of this element. Hypokalemia can be suspected by increasing muscle weakness, increased fatigue, and heart rhythm disturbances. Potassium deficiency can be confirmed by laboratory tests.
Classification
Most often in clinical practice, hypokalemia is divided into:
- light
- K+ content 3-3.5 meq/l. - severe
- K+ level below 3 mmol/l.
Separately, pseudohypokalemia is distinguished, which has no symptoms and does not require treatment. A false test result can be obtained if the patient has a very high level of leukocytes (leukocytes actively absorb K+). This happens, for example, with leukemia or severe infection. Falsely elevated readings are also possible if the K+ concentration is determined in blood stored for a long time at room temperature.