This is a blood test to determine its clotting ability. A hemostasiogram (coagulogram) evaluates the state of blood flow in all organs and systems.
A blood test for a hemostasiogram is done within one day. In laboratories, a blood test for a hemostasiogram (coagulogram) differs in parameters, measurement methods and, accordingly, information content and cost. The state of the coagulation system is a functional analysis that reflects changes in blood coagulation or the hemostatic system. The hemostasis system changes depending on external or internal factors. Factors influencing changes in the hemostatic system include age over 40 years, taking OCs and HRT, smoking, surgery, trauma, pregnancy, IVF protocol, etc. Accordingly, the results of the hemostasiogram analysis with the above factors will change.
It is important to monitor the function of blood clotting in pregnant women, patients with oncology and disorders of the cardiovascular system, when prescribing OCs and HRT, when planning surgery; also in patients with a family history of thrombosis, etc.
Hemostasiogram and coagulogram
One may mistakenly think that a hemostasiogram does some additional research and includes an analysis of the plasma system, but this is not the case. Laboratory actions for hemostasiogram and coagulogram are identical. But hemostasiogram and coagulogram differ in parameters, measurement methods and information content among laboratories.
Why do you need to do a hemostasiogram? The hemostasiogram reflects normal blood flow; in case of abnormalities, a shift in blood flow towards thickening or the risk of hemorrhage. Based on the results, you can understand what a person may suffer from - increased blood clot formation or blood loss. This procedure must be carried out before surgery to assess the risk of possible complications. Analysis during pregnancy will allow you to avoid complications throughout the entire period and how to better prepare for the birth process.
Extended hemostasiogram RUB 1,100.
Coagulogram 650 rub.
D-Dimer 1,100 rub.
All prices Make an appointment
Functions of platelets in platelet-vascular hemostasis
Platelets are an important link in ensuring the entire process of eliminating bleeding. For the full functioning of the primary link of hemostasis, structurally intact cells must be present in the bloodstream.
The process of platelet adhesion at the site of injury
The role of blood cells in hemostasis is determined by their action in the bloodstream:
- Angiotrophic. Ensure normal functional ability and permeability of the walls of blood vessels.
- Reparation. In places where microvessels are damaged, growth factor is activated, stimulating the formation of collagen fibers.
- Angiospastic. They support microvascular spasm through the production of active substances.
- Coagulomodulating. Regulation of blood clotting processes.
- Retractile. Compaction of the formed blood clot.
- Adhesive-aggregation. Adhesion of cells to the surface of damaged vessels.
Slowing down or stopping bleeding occurs as a result of the formation of a small diameter blood clot, but it cannot return to the bloodstream, causing complete blockage of the vessel.
How to prepare for donating blood for a hemostasiogram
Blood is donated on an empty stomach, from a vein. 12 hours before hemostasis, you must adhere to a diet excluding fatty and protein foods. The last meal (light snack) is possible 4 hours before blood sampling. It is prohibited to drink alcohol the day before the test. It is recommended to replace any drinks with water. This is done so that sugar does not affect the overall picture.
If you are taking medications that may affect the results of the data, this must be indicated when taking the test. This will be taken into account when deciphering the testimony.
It is not recommended for women to undergo the procedure during menstruation.
It is also better to refrain from playing sports in the previous day, to avoid stress and overexertion. Smokers are advised to give up cigarettes during this time.
The process of drawing blood also affects the accuracy of the result. When collecting from a vein, it is better to use a vacuum system. If this is not possible, then a syringe is used and the blood is allowed to flow on its own.
Indicators
It is extremely problematic to independently understand the results obtained without special education. Based on the results of the hemostasiogram, you must make an appointment with a hemostasiologist or hematologist.
The form indicates the results obtained and the norms given in two columns. These are indicators of prothrombin, aPTT, prothrombin time, prothrombin index, fibrinogen, platelet function, thrombin time, RKMF, INR.
In a detailed analysis, an additional test for D-dimer, lupus anticoagulant, and antithrombin III is often prescribed.
Tests during pregnancy
Hemostasiogram
Pregnancy management
Hemostasiologist during pregnancy
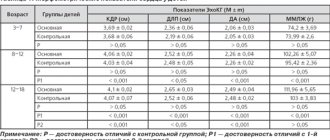
Normal indicators
According to APTT data, the rate at which blood clots is assessed. Ideally, it should be from twenty-four to thirty-six seconds, laboratory referents differ - ADD. With a lack of vitamin K, this time will be longer. In this case, you should be wary of severe blood loss from cuts and deeper wounds. If the time, on the contrary, is less, this means that there is a risk of a blood clot. In this case, during pregnancy the baby will not receive enough nutrients.
The line with data on prothrombin contains the same results, but in percentage equivalent. So prothrombin should be from 78 to 95 to 105 percent.
Fibrinogen should normally be from two to four grams per liter; during pregnancy it can increase.
With normal levels, antithrombin III ranges from 71 to 115 percent,
Exact standards in laboratory abstracts. If deviations are greater or lesser, blood clots or bleeding may appear.
Thrombin time should be from eleven to eighteen seconds, and prothrombin time should be from fifteen to seventeen.
Platelet function is from 30 to 50%, a decrease in function indicates the risk of bleeding or the effectiveness of antiplatelet therapy, an increase indicates an increase in the aggregation function of the blood.
Hemostasiogram in pregnant women
Pregnant women need to especially carefully monitor blood clotting. This will avoid complications during the birth process, as well as throughout pregnancy.
During pregnancy, a hemostasiogram is taken once per trimester or more often if indicated.
The attending physician may prescribe additional tests if there is a threat of miscarriage, also to assess the effectiveness of anticoagulant therapy. It is also recommended to do a hemostasiogram in case of high blood pressure, edema, the presence of protein in a urine test, before surgery, or when prescribing OCs and HRT.
If test results are poor, consultation with a hemostasiologist is necessary.
Do not be alarmed if you suddenly discover that the coagulation rate is slightly higher than required. In pregnant women, this may also be a normal option. This may happen due to changing hormonal levels. For women in an interesting position, it is unstable and can change more than once. The result may be affected by the appearance of an additional circulation that connects the uterus and placenta and an increase in blood volume.
Impaired hemostasis
General information
The process of hemostasis is able to prevent and stop the flow of blood from the vessel. It is he who ensures the formation of the fibrin clot necessary to restore the integrity of the tissue, and finally removes the fibrin when it is no longer needed. Thanks to this system, blood performs an important function - maintaining a liquid state of blood that flows through the vessels, as well as coagulation when the integrity of the vascular wall is violated. As a result, hemostasis should work to maintain blood volume in the body. This complex system involves platelets, blood cells, extravascular tissues, and the vascular wall. Violation of one of the components leads to disruption of the hemostasis process itself.
Causes of impaired hemostasis:
- DIC syndrome. A common type of hemostasis pathology. Blood clotting is impaired due to the massive release of thromboplastic substances from tissues. May be asymptomatic.
- Impaired hemostasis (coagulopathy). Violation of the functions of the blood coagulation and anticoagulation systems. Pathological condition of the body. It is possible to distinguish immune, acquired and genetic forms of coagulopathies.
- Thrombotic syndrome (thrombophilia). It is characterized by inadequate blood coagulation and thrombus formation, leading to ischemia of tissues and organs.
- Hypocoagulative-hemorrhagic condition. Accompanied by a pathological process of reducing blood clotting.
Classification of hemostasis disorders:
- hereditary or acquired;
- hypocoagulative (decreased blood clotting) or hypercoagulative (increased blood clotting);
- local (thrombosis) or global (DIC syndrome).
Reduced blood clotting
Reduced blood clotting can be manifested by increased bleeding, repeated bleeding, and hemorrhages that occur even with minor injuries. Platelet-vascular hemostasis is disrupted by quantitative and qualitative changes in platelets (thrombocytopenia and thrombocytopathies), as well as lesions of the vascular wall. Thrombocytopenia is a decrease in the platelet count in the blood below normal. However, spontaneous bleeding occurs only when its number decreases to less than 30 G/l. Thrombocytopathies are understood as qualitative inferiority and dysfunction of platelets with normal or reduced levels.
Causes of decreased blood clotting:
- Immune reactions (viruses, drugs);
- Deficiency of cyanocobalamin and folic acid;
- Effect of toxic drugs;
- Hormonal disorders (hypothyroidism);
- Heredity.
One of the possible causes of bleeding may be a decrease in the production of von Willebrand factor by the endothelium of the vascular wall - a large molecular component of blood coagulation factor VIII (hereditary von Willebrand disease). This factor accumulates in platelets and is released during their degranulation.
Hemorrhagic syndrome
Hemorrhagic syndrome is characterized by a state of increased bleeding and disturbances in one of the links of the blood coagulation system. It can be either an acute or chronic disease.
Characteristic symptoms:
- rash in the form of small dots;
- spots up to 3 mm in diameter (petechiae);
- bruises on the skin and mucous membranes (eczymoses);
- spontaneous bleeding.
Ecchymoses are not just bruises, but characteristic signs of hemorrhage into the skin or mucous membrane. If the above symptoms are detected, it is important to conduct laboratory diagnostics. It will show indicators of a decrease in the number of platelets and an increase in the bleeding time.
von Willebrand disease
Von Willebrand disease is a congenital deficiency of von Willebrand factor (VWF) that results in platelet dysfunction. Usually characterized by mild bleeding. There is also an increase in bleeding time, a normal platelet count, and possibly a slight increase in partial thromboplastin time. The diagnosis is based on low levels of von Willebrand factor antigen and abnormal ristocetin cofactor activity. Treatment includes bleeding control with replacement therapy
Symptoms of von Willebrand disease:
- tendency to subcutaneous hemorrhages;
- prolonged bleeding of small cuts;
- prolonged menstruation (in some cases);
- abnormal bleeding after surgery.
Thrombocytopenia due to impaired hemostasis
Thrombocytopenia is characterized by a decrease in the number of platelets and is accompanied by increased bleeding and problems with bleeding. It can accompany any hematological diseases as one of the main symptoms.
As an independent disease, it is sometimes diagnosed as Werlhof's disease . The main causes of thrombocetopenia are impaired platelet production, as well as their increased destruction. Also among the possible causes are infectious and epidemiological :
- HIV;
- hepatitis;
- acute manifestations of herpes infection;
- Infectious mononucleosis;
- ARVI;
- flu.
Impaired hemostasis and the development of bleeding during thrombocytopenia are caused by the following mechanisms:
- increasing the permeability of microvessels for red blood cells and other components of the blood;
- fragility of blood vessels due to wall degeneration;
- decrease in the adhesive-aggregation function of platelets;
- violation of the reaction of release of platelet coagulation factors;
- decreased clot retraction as a result of decreased activity of platelet contractile protein.
Coagulation hemostasis
Along with the primary, vascular-platelet hemostasis, a secondary hemostasis develops - coagulation. It plays the role of additional support and regulation of blood loss from the vessels. Violation of coagulation hemostasis can be caused by the following factors :
- activation of the fibrinolytic system;
- increase in endogenous anticoagulants;
- overdose of anicoagulants.
Anticoagulants inhibit the formation of fibrin threads; they prevent thrombus formation, help stop the growth of existing blood clots, and enhance the effect of endogenous fibrinolytic enzymes on blood clots.
Causes of phase I disorders of blood coagulation
thromboplastin formation may be the following:
- decreased production of factors (IX, X) in liver pathology;
- formation of antibodies in leukemia;
- overdose of the anticoagulant heparin;
- genetic defects in the synthesis of factors VIII, IX and XI.
Causes of phase II coagulation disorders
Causes of violations of thrombin :
- liver diseases;
- hypovitaminoses;
- jaundice;
- enteritis;
- drug dysbacteriosis;
- extensive resection of the small intestine;
- anaphylactic shock;
- heparin overdose.
Causes of phase III coagulation disorders
Hemorrhagic diathesis associated with a violation of the third phase of coagulation - the phase of fibrin , occurs when:
- liver pathologies;
- affected lungs;
- hereditary factor;
- injuries (surgeries) of the lungs, pancreas, burns.
Increased blood clotting
Increased blood coagulation manifests itself at the local level (thrombosis) or manifests itself as generalized intravascular coagulation. The basis of the disease is a violation of platelet-vascular and coagulation hemostasis.
Hypercoagulation can be caused by:
- increased platelet count in the blood;
- weakening of fibrinolysis;
- an increase in platelet content in the blood;
- decreased antithrombotic properties of the vascular wall.
DIC syndrome is a severe disorder of hemostasis that occurs when there is an excessive intake of procoagulants and blood coagulation activators into the blood, which leads to the formation of multiple microthrombi in the vessels of the microvasculature, and then the development of hypocoagulation, thrombocytopenia and hemorrhage as a result of increased functional activity of the anticoagulation system and blood fibrinolysis with subsequent depletion of all systems. The universality and nonspecificity of DIC syndrome is due to the variety of possible factors of its occurrence. Among them, doctors highlight:
- traumatic surgical operations;
- states of shock;
- infections;
- renal failure;
- obstetric ptology;
- intravascular hemolysis;
- terminal states (the process of the body dying).
Treatment of hemostasis disorders
Treatment of the disease is a difficult task for the resuscitator and anesthesiologist. Most patients with hereditary and congenital forms of pathologies undergo treatment and observation by a specialist throughout their lives. Doctors use three basic principles for treating hemostatic disorders.
Etiotropic principle of treatment. It is necessary to exclude or reduce the degree of action of factors causing hemostasis disorders. This may be protection from the following factors:
- physical:
- chemical;
- biological;
- pathological.
Pathogenetic principle of treatment. To prevent the procoagulant activity of platelets, injections of procoagulants and antifibrinolytic drugs are practiced. Transfusions of whole blood, platelets, and protein blood products (fibrinogen, thrombin) are also actively used.
Symptomatic principle of treatment. Solutions are introduced into the patient's body that normalize the rheological properties of blood (blood fluidity). As a result, normalization of the functions of organs and tissues impaired due to microcirculation disorders, bleeding and hemorrhage is achieved.
Hemostasis test for pregnant women
The threat of large blood loss during childbirth is the main criterion that guides the obstetrician-gynecologist when prescribing a hemostasis test for a pregnant woman. However, in addition to this, a hemostasiogram can be prescribed by the doctor monitoring the course of pregnancy in the case when the patient develops gestosis or has uterine hypertonicity, there is a threat of miscarriage, or there is a delay in intrauterine development of the child. A hemostasis test is usually prescribed even if the pregnancy is multiple. When observed by an obstetrician-gynecologist in a medical clinic, a woman undergoes all necessary examinations during pregnancy.
Conventional and advanced hemostasis analysis
This diagnostics in Yeysk can be carried out at the Sensitive LCC both according to the regular program and in an expanded form. The standard hemostasiogram includes the following indicators:
- thrombin and prothrombin time;
- prothrombin level;
- fibrinogen level;
- platelet count in peripheral blood;
- soluble complexes of monomers and fibrin.
An advanced analysis for hemostasis adds to the above indicators the study of such parameters as:
- antithrombin III,
- lupus anticoagulant and D-dimer,
- von Willebrand factor.