Types and specific symptoms
The disease comes in several types and each of them has its own causes and symptoms.
Iron-deficiency anemia
- the most common type, occurs when there is a deficiency of iron in the body. Signs: shortness of breath during exertion, rapid heartbeat, tinnitus, pale and dry skin, cracks in the corners of the lips, brittle nails.
B12 and B9 deficiency anemia
— occur with a deficiency of vitamins B12 and folic acid. Signs: deterioration of mental activity, disturbances in the functioning of the central nervous system, unsteady gait, decreased sense of touch.
Hemolytic
- characterized by accelerated destruction of red blood cells, in newborns it occurs as a result of a conflict between the red blood cells of the mother and child.
Aplastic and hypoplastic anemia
- a disease associated with disruption of the hematopoietic function of the bone marrow.
Posthemorrhagic
- the result of blood loss. It can be acute (for injuries and operations) or chronic (for some types of internal diseases).
Sickle cell anemia
- the result of a genetic defect in which red blood cells take on a sickle shape. Signs are general weakness, increased fatigue, a tendency to form blood clots, pain in the joints and abdominal cavity.
Hereditary thalassemia
- the most severe type, caused by genetic disorders.
Each type is dangerous in its own way for humans, since iron deficiency negatively affects the functioning of all its organs.
Why does the blood composition change?
Anemia develops under the influence of many provoking factors. These include:
- genetic diseases of the red bone marrow;
- deficiency of iron, vitamin B12, folic and ascorbic acid;
- injuries, extensive burns or frostbite of the skin;
- congenital or acquired kidney pathologies;
- liver diseases (hepatitis, cirrhosis);
- diseases of the digestive system (colitis, ulcers, gastritis);
- oncological formations;
- damage to internal organs by viral or bacterial infections;
- chemical or food poisoning of the body.
The conditions described above negatively affect the qualitative or quantitative composition of the blood, leading to impaired formation of red blood cells and hemoglobin deficiency.
Deficiency of red blood cells and hemoglobin occurs in many diseases
Important! Only timely treatment of anemia will help maintain health and prevent many negative consequences.
The severity of anemia is determined by the concentration of hemoglobin in the blood.
- 1st degree (mild) - the hemoglobin level is 20% below normal: 90 - 120 g/l, mild weakness, fatigue, and decreased concentration appear.
- Grade 2 (moderate) - hemoglobin is 20-40% below normal (70-89 g/l), shortness of breath, rapid heartbeat, disturbed sleep and appetite, tinnitus and frequent headaches.
- Grade 3 (the most severe) - hemoglobin is below normal by more than 40% (less than 70 g/l), signs of heart failure occur, treatment is recommended in a hospital.
Mechanism of disease development
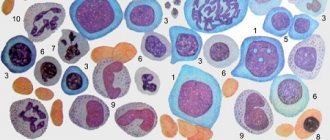
Red blood cells are synthesized by red bone marrow tissue. Protein and non-protein fractions take part in this process, as well as a special hormone produced by the kidneys (erythropoietin). The role of red blood cells is very important, since these cells transport oxygen and nutrients through the tissues of the body, while simultaneously removing carbon dioxide and waste products. The period of active functioning is 90–120 days, after which the red cells are utilized in the spleen.
Red blood cells are filled with a special protein - hemoglobin, which contains iron. It is this that colors the cells red. Hemoglobin is necessary for respiratory function. Thanks to it, oxygen molecules are distributed throughout all human tissues and internal organs. With a decrease in the number of red blood cells and hemoglobin in the blood, anemia develops, accompanied by many negative symptoms. In medical practice, there are 3 degrees of anemia, each of which entails certain clinical signs.
Treatment of anemia
Effective treatment is impossible without accurate diagnosis and identification of the cause of anemia.
Examination methods:
- anamnesis;
- general blood analysis;
- blood chemistry;
- general clinical urine test;
- CT scan;
- endoscopy;
- rectoscopy;
- Ultrasound (for women).
At the medical office, you can get qualified advice from a therapist and carry out all the necessary tests and any additional tests on site.
Share the article on social networks:
Classification of anemia by severity
The concept of “anemia” includes several types of disease, each of which has its own stages of development. The classification of anemia by severity depends on the causes of the pathology. Let's look at each type in detail.
Iron-deficiency anemia
This type of pathology is accompanied by a decrease in the amount of iron in the human blood (hypochromic anemia). A patient with this condition experiences a decrease in hemoglobin and blood color index. Most often, anemia, accompanied by a lack of iron, occurs in people who do not eat meat, pregnant women, in patients with heart defects, and also due to the loss of large amounts of blood (due to injuries, internal bleeding or during surgery).
Degrees of the disease:
- the first one often goes unnoticed. The patient may experience periodic headaches, malaise, and fatigue;
- the second – causes memory impairment, attention, dizziness, drowsiness. Second degree anemia of this type is often characterized by shortness of breath and rapid heartbeat;
- the third – entails the development of pronounced symptoms. The patient is concerned about sleep disorders, loss of ability to work, chronic fatigue, hair loss, brittle nails, peeling skin, and gum problems.
People in the final stages of iron deficiency anemia complain of frequent limb cramps, for example, when walking or climbing stairs. If such manifestations are detected, it is recommended to immediately consult a doctor, since the course of the pathology only worsens over time.
B12 deficiency anemia
This type of anemia is caused by a lack of vitamin B12 in the body. When the diagnosis is made, the patient is found to have an increased number of cells, the precursors of red blood cells - megaloblasts. In this case, it is customary to talk about the hyperchromic type of anemia. Among the main causes of the disease are insufficient intake of B12 from food, diseases of the digestive tract, conditions in which the body requires an increased amount of the vitamin (intense physical activity, rapid growth, multiple pregnancy).
B12 deficiency anemia has several degrees of severity
Severity of B12-deficiency anemia:
- the first is characterized by weakness, headaches, dizziness, and increased fatigue;
- the second – causes a yellow color of the skin, rapid heartbeat, shortness of breath, tachycardia, and increased blood pressure. In addition, grade 2 anemia causes loss of appetite, weight loss, pain in the intestines, and the formation of ulcers in the oral cavity;
- the third is accompanied by the addition of various neuralgic disorders. In addition to the symptoms described above, patients note muscle weakness, trembling and numbness of the limbs, and atrophy of the leg muscles.
Treatment of this type of anemia is carried out by eliminating the underlying disease that led to a violation of the blood composition and following a therapeutic diet.
Average degree
With iron deficiency anemia, in most patients the decrease in Hb is relatively moderate (up to 85 - 114 g/l), much less often a more pronounced decrease develops - up to 60 - 84 g/l. Anemia at this stage can manifest itself with the following clinical symptoms:
- weakness, fatigue;
- shortness of breath, palpitations on exertion;
- dizziness, darkening of the eyes when standing up quickly and in a stuffy room;
- pulsation in the temples, neck;
- headache;
- possible weakening of attention, memory deterioration, decreased mental performance;
- the course of coronary heart disease becomes more severe;
- pallor of the skin and mucous membranes.
In some patients with iron deficiency anemia, a connection with restless legs syndrome is described. It is characterized by the need to move the legs due to a feeling of discomfort that arises in them, mainly in the evening and at night. The appearance of palpitations will characterize the transition to the stage of severe anemic syndrome.
Anemia... Is it always due to gastritis and lack of iron?
Anemia is not an independent pathology; it is a symptom that accompanies a number of diseases that are not always associated with the hematopoietic system. Thus, anemia often occurs with gastrointestinal diseases, metabolic diseases, when the absorption of iron or vitamin B12 is impaired. Anemia is diagnosed when the concentration of hemoglobin in the blood decreases, the number of red blood cells decreases, or their qualitative composition changes.
Symptoms and dangers of anemia
Healthy heart
Functional examination methods, laboratory and other types of diagnostics, selected specifically taking into account age, general health and individual characteristics, allow you to get a complete picture of the health of the cardiovascular system in 1-2 days without unnecessary time and financial expenses.
The main task of red blood cells is to transport oxygen to tissues. If red blood cells or hemoglobin are defective or their concentration is insufficient, the body suffers from oxygen starvation. Because only in the presence of oxygen does energy production become possible. In other words, the body simply does not have enough strength to live and function normally. Hence the manifestations of the disease; an experienced doctor will suspect anemia based on an examination by a doctor:
- cyanosis of the skin and mucous membranes;
- shortness of breath with minor exertion (the body compensates for the lack of oxygen by trying to inhale more air);
- hair loss and thinning;
- poor condition of nails (brittleness, thinness, lamination);
- tachycardia and palpitations even with minor exertion;
- memory impairment, decreased performance, sleep disturbances and other neurological symptoms such as lethargy, apathy, nervousness;
- “flies” before the eyes;
- dizziness when suddenly changing position
With serious anemia, pain in the heart, swelling of the limbs, pain in the limbs, even cramps and intermittent claudication occur. There may be food perversions - desire for bitter things, eating ice, sand, earth.
Children with anemia are stunted in growth and development, women experience menstrual irregularities, and have problems conceiving (including miscarriages).
Acute anemia is easily treated; often only nutritional correction is sufficient. They occur after blood loss (trauma, surgery). Acute anemia can also be called anemia in pregnant women (if the woman never had anemia before pregnancy). WHO allows a natural decrease in hemoglobin in the third trimester to 105 g/l, and in the first two to 110 g/l. If the fetus’s nutrition is not impaired, the woman does not complain, her diet is complete, often the doctor does not prescribe treatment, monitoring only the hemoglobin level. Nowadays, various diets have become fashionable, including those with the complete exclusion of animal foods, this contributes to the growth of iron deficiency anemia among healthy people.
B12 deficiency anemia
It is considered a relatively simple form, red blood cells and hemoglobin molecules are not changed, hematopoiesis is normal, but anemia occurs due to a lack of vitamin B12. In this case, the deficiency should be chronic; only 5-6 years after the cessation or decrease in the supply of vitamin B 12 does anemia occur. If such anemia is not detected in a timely manner and the lack of vitamin B12 is not compensated for, the type of hematopoiesis changes, which can lead to serious problems. Most often, B12 deficiency anemia occurs due to gastrointestinal diseases:
- inflammatory and atrophic diseases of the intestines and stomach;
- operations on the gastrointestinal tract with partial or complete resection of one of the areas;
- parasites (tapeworms, etc.);
- liver diseases;
- constant use of certain medications (for example, anticonvulsants).
In addition, such anemia accompanies other blood diseases - leukemia, erythromyelosis.
What to do: first of all, take a detailed blood test, the hematologist will see the changes, collect anamnesis and, if necessary, involve other specialists - most often a gastroenterologist and an infectious disease parasitologist. This type of anemia responds well to treatment or compensation, with the exception of blood cancer.
Previously, B12 deficiency anemia was observed in children who were fed goat milk or powdered milk. Today, even formula-fed children who receive formula are protected from anemia.
The main danger: a long asymptomatic period. If you have gastrointestinal diseases, you often eat fish or medium-cooked meat, or have “problems” with your liver, take a detailed blood test regularly.
Iron-deficiency anemia
The main reason is loss of iron with hidden bleeding or lack of it in food. Congenital iron deficiency and iron transport disorders are rare. Long, heavy menstruation in women depletes the body, they are not the norm, and the iron supply does not have time to be replenished. The second reason is chronic minor bleeding of the gastrointestinal tract - they are detected by tests for occult blood in the stool. Infectious diseases and serious burns can contribute to the development of iron deficiency anemia. Another reason is malnutrition, this is especially dangerous in childhood during the period of active growth - from birth to 2-3 years, when the body actively accumulates, but also consumes iron no less actively. The second stage is puberty - girls begin menstruation.
Previously, it was believed that gastritis was one of the causes of iron deficiency anemia, but no, atrophic gastritis occurs in response to a lack of iron.
For diagnosis, it is not enough to take a blood test; you need to find out at what stage the anemia is. Since the body initially uses tissue iron, the tests in this case will be normal. You also need to get tested for serum iron, ferritin and transferrin.
If detected in a timely manner, the prognosis is usually favorable, the patient is either cured completely or takes iron supplements according to the prescribed regimen. Of course, it is recommended to change your diet, choosing a balanced diet rich in microelements, vitamins and not giving up protein foods.
Anemia associated with disturbances in red blood cells and hemoglobin
It is these anemias that are chronic pathologies, the most severe of which are associated with the inability of the bone marrow to regenerate:
aplastic anemia (bone marrow does not produce enough blood cells). In severe cases, a bone marrow transplant is required. Bone marrow suppression can be congenital or acquired. Main reasons:
- poisoning by chemicals (in particular heavy metals);
- ionizing radiation (radiation);
- taking medications (in some cases, aplastic anemia is observed only while taking medications, in others it can be persistent)
- infectious diseases (severe infections in risk groups)
- autoimmune diseases.
hemolytic anemias are associated with increased destruction of red blood cells. Usually the structure of the erythrocyte is disturbed, there is a deficiency of enzymes, there are disturbances in the hemoglobin molecule - these anemias are congenital and are often hereditary. Acquired hemolytic anemia most often occurs due to the toxic effects of hemolytic poisons, immune diseases, and often hemolytic anemia complicates operations for prosthetic heart valves. A striking example of hemolytic anemia is jaundice in newborns - maternal antibodies destroy the red blood cells of the fetus, as a rule, the prognosis is favorable, but some children require a blood transfusion - as soon as the antibodies leave the body, hematopoietic functions are completely restored. Sometimes hemolytic anemia may be the only manifestation of lymphoma.
This is a brief excursion into anemia; in fact, their classification is quite complex, but the first two pose a real threat to a group of healthy people, as they are diagnosed too late. The therapist will not always offer to take extensive tests or conduct biochemical studies.
What to do? Regular monitoring of blood tests and scheduled visits to the doctor are enough for people who are considered healthy. If you are at risk, the doctor will determine treatment tactics, taking into account diagnostic data.
What tests are taken if anemia is suspected (minimum list)
- Prelatent iron deficiency:
- Ferritin is either reduced or has a tendency to decrease
- Transferrin and percentage of transferrin saturation are within normal limits
- Iron is within normal limits
- Complete blood count and hemoglobin content in red blood cells are within normal limits
Latent iron deficiency
- Ferritin is reduced in women <10 µg/l, in men <20 µg/l
- Transferrin > 4g/l;
- Transferrin saturation in women <15%, in men <20%
- Iron in women <8 µmol/l in men <11 µmol/l
- Complete blood count and hemoglobin content in red blood cells are within normal limits
Iron deficiency
- Ferritin is reduced in women <10 µg/l, in men <20 µg/l
- Transferrin > 4g/l;
- Transferrin saturation in women <15%, in men <20%
- Iron in women <8 µmol/l in men < 11 µmol/l
- hemoglobin content in red blood cells <80fl
- hemoglobin 100-120 g/l
You can take a blood test with us without having to visit a doctor, but you can make an appointment with a therapist or hematologist for an extended consultation if there are abnormalities in the analysis. At the same time, the danger of self-diagnosis is that one basic analysis may not be enough, you remember that some anemias begin to appear only after 5-7 years
Forecast and prevention of iron deficiency anemia
In most cases, iron deficiency anemia can be successfully corrected. However, if the cause is not addressed, iron deficiency may recur or progress. Iron deficiency anemia in infants and young children can cause delayed psychomotor and intellectual development.
In order to prevent iron deficiency anemia, annual monitoring of clinical blood test parameters, nutritious nutrition with sufficient iron content, and timely elimination of sources of blood loss in the body are necessary. Persons at risk may be advised to take prophylactic iron supplements.
Treatment of IDA
The basic principles of treatment for iron deficiency anemia include eliminating the cause of iron deficiency, correcting the diet, and replenishing iron deficiency in the body.
- The diet for iron deficiency anemia consists of eating foods rich in iron. Patients are advised to have a nutritious diet with the obligatory inclusion in the diet of foods containing heme iron (veal, beef, lamb, rabbit meat, liver, tongue). Plant foods rich in iron include beans, beans, lentils, peas, spinach, cauliflower, potatoes, carrots, beets, bananas, apricots, peaches, apples, blueberries, raspberries, strawberries, almonds and walnuts. It should be remembered that ascorbic acid, which is found in bell peppers, cabbage, rose hips, currants, citrus fruits, sorrel, enhances the absorption of iron in the gastrointestinal tract, and oxalates and polyphenols (coffee, tea, soy protein, milk, chocolate) worsen the absorption of iron. calcium, dietary fiber and other substances. However, no matter how much meat we eat, only 2.5 mg of iron will enter the bloodstream per day - this is exactly how much the body can absorb. And 15-20 times more is absorbed from iron-containing complexes - that’s why the problem of anemia cannot always be solved with the help of diet alone, and therefore iron-containing drugs are prescribed
- Oral iron supplements differ from other medications by special rules of administration: - short-acting iron-containing preparations are not taken immediately before or during meals. The medicine is taken 15-20 minutes after meals or in the pause between doses; prolonged medications (sorbifer durules, tardiferron-retard, etc.) can be taken before meals and at night (1-2 times a day); - iron supplements are not taken with milk and milk-based drinks (kefir, fermented baked milk, yogurt) - they contain calcium, which will inhibit the absorption of iron - tablets (except for chewable ones), dragees and capsules are not chewed, are swallowed whole and washed down with plenty of water, rosehip decoction or clarified juice without pulp Oral iron supplements (in tablets, drops, syrup, solution) are the initial treatment for mild to moderate anemia; if there is pregnancy, the intake is agreed with an obstetrician-gynecologist. The duration of treatment is 4–8 weeks until hemoglobin levels normalize, then the drug is taken for 4–6 weeks at half the dose. The most commonly prescribed: - sorbifer durules/fenuls 100 mg, 1-2 tablets 1-2 times a day until hemoglobin levels are restored (in pregnant women, for prevention, 1 tablet 1 time a day, for treatment, 1 tablet 2 times a day) - ferretab comp . 1 capsule per day, up to a maximum of 2-3 capsules per day in 2 divided doses, minimum period of use is 4 weeks - maltofer/actiferrin comes in three dosage forms (drops, syrup, tablets), intake 40-120 drops/10-30 ml syrup / 1-3 tablets per day in 1-2 doses - tardiferron 80 mg, 1-2 tablets per day, pregnant women 1 tablet per day, II-III trimester - totema (combined preparation of iron, copper and manganese) 2- 4 ampoules per day, solution diluted in 1 glass of water, taken for 3-6 months - ferlatum 15 ml 1-2 bottles per day in 2 divided doses
- Injectable iron preparations (venofer, likfer, cosmofer, ferrinject) are used exclusively in the hospital (it is necessary to have the ability to provide anti-shock care), contraindicated during pregnancy and lactation
- Hemotransfusion (transfusion of red blood cell-containing blood components) is performed in case of severe anemia, according to strict indications and in a hospital setting.
Mild anemia
Anemia may not cause any clinical manifestations for a long time. Iron deficiency is observed in 30% of women, in some countries this figure reaches 70%. The high rate of patients with anemic syndrome in our country is associated with a large number of births and low meat content in the diet.
In case of iron deficiency anemia, the term “mild anemia” is used incorrectly: if anemia is detected, iron deficiency is already progressing. Treatment with iron supplements at this stage is necessary, since the lack of a microelement has consequences even when anemia is not clinically manifested.
Along with iron deficiency anemia, an iron deficiency state without anemia is distinguished. This is sideropenia - a low iron content in the blood plasma, a decrease in the iron content in reserves with normal hemoglobin levels and the number of red blood cells. Latent iron deficiency is the stage preceding iron deficiency anemia. If there is no replenishment of iron deficiency, sooner or later anemia occurs.
What is hemoglobin
Hemoglobin (Hb) is the red iron-containing pigment in the blood. It is the main component of red blood cells and makes up 35% of their total mass. It is a complex protein consisting of heme (the non-protein part, an iron complex with protoporphyrin) and globin, the protein component. Main functions of hemoglobin:
- transport oxygen from the lungs to tissues;
- remove carbon dioxide from the body;
- regulate the acid-base state (ensure the normal course of redox processes in the blood plasma).
There are physiological and pathological types of hemoglobin. They differ in the amino acid composition of globin, physical properties and affinity for oxygen. Physiological hemoglobins include Hb A (adult hemoglobin) and Hb F. The bulk of hemoglobin in an adult consists of the following fractions:
- Hb A1 (96−98%) – main;
- Hb A2 (2−3%) – slow;
- Hb F (1−2%).
Hemoglobin F – fetal. It makes up the bulk of fetal Hb. In newborns, its part is 60 - 80%. By the fifth month of life, its amount decreases to 10%. And by the second year of a child’s life, hemoglobin F disappears almost completely.
Hemoglobin A appears in the fetus at 12 weeks. In an adult, it makes up the bulk. Changing the ratio of hemoglobin types in the blood is used in clinical practice to diagnose various pathological conditions. Hemoglobin F in concentrations up to 10% can be detected in aplastic, megaloblastic anemia.
In addition to physiological hemoglobins, there are several pathological varieties of hemoglobin, differing from each other in physicochemical qualities: B(S), C, D, E, G, H, I, Y, K, L, M, N, O, P and Q. Abnormal hemoglobins result from a congenital, inherited defect in hemoglobin formation. Changes in the molecular structure of Hb (impaired synthesis of globin chains) are the basis for the development of hemoglobinopathies. These are “molecular” diseases. Hemoglobinopathies (hemoglobinoses) can cause the development of severe stages of hemolytic type anemia. The most common hemoglobinopathy S is sickle cell anemia.
The level of hemoglobin in the blood of healthy individuals is 132 – 164 g/l in men and 115 – 145 g/l in women. Age-related changes in hemoglobin content are shown in Table 1. Table 1
| Age | Red blood cells, × 10 12 /l | Hemoglobin, g/l | Reticulocytes (young red blood cells),% |
| Newborns | 6,0 | 210,0 | 20,0 |
| 2 – 4 weeks | 5,3 | 170,6 | 14,0 |
| 1–3 months | 4,4 | 132,6 | 13,0 |
| 4 – 6 months | 4,3 | 129,2 | 12,0 |
| 7 – 12 months | 4,6 | 127,5 | 10,0 |
| Over 2 years old | 4,2 – 4,7 | 116 – 135,0 | 7,0 |
| Adults: | 2 – 12,0 | ||
| men | 4,0 – 5,1 | 132 – 164,0 | |
| women | 3,7 – 4,7 | 115 – 145,0 |
Determining the concentration of hemoglobin in the blood plays a vital role in the diagnosis of anemia. The conclusion about the presence of anemia is based on the results of determining the level of hemoglobin and the hematocrit value Ht (the part of the blood volume accounted for by red blood cells):
- for men - a decrease in Hb concentration below 140 g/l and Ht less than 42%;
- for women - less than 120 g/l and 37%, respectively.
The hemoglobin concentration in the blood can increase to 180 − 220 g/l and higher:
- with tumor diseases of bone marrow cells, increased formation of red blood cells - erythremia;
- with a symptomatic increase in the number of red blood cells and hemoglobin (erythrocytosis), which occurs in various conditions.
Changes in hemoglobin concentration in various diseases are presented in Table 2. Table 2
| Increased Hb concentration | Reduced concentration |
|
|
In some diseases, a false increase in hemoglobin concentration in the blood is observed. The study of hemoglobin concentration over time provides important information about the clinical course of the disease and the effectiveness of treatment.
Causes of iron deficiency anemia (IDA)
- insufficient intake of iron from food: fasting, vegetarianism, or a diet depleted in iron and protein, followed for a long time. In breastfed children, the cause may be iron deficiency anemia of the mother, early transfer to artificial feeding, late introduction of complementary foods
- impaired iron absorption: enteritis (inflammation of the mucous membrane of the small intestine caused by infection or helminthic infestation), gastritis and peptic ulcer of the stomach and duodenum; hereditary diseases (cystic fibrosis and celiac disease); autoimmune damage to the intestinal mucosa and possibly the stomach (Crohn's disease); condition after removal of the stomach and/or duodenum; stomach and intestinal cancer
- chronic blood loss. This is the most basic reason. This includes losses due to: gastric and duodenal ulcers, nonspecific ulcerative colitis, Crohn's disease, hemorrhoids and anal fissures, intestinal polyposis, bleeding from disintegrating tumors of any location and varicose veins of the esophagus; hemorrhagic vasculitis; pulmonary hemorrhages, pulmonary hemosiderosis; chronic pyelonephritis, polycystic disease and cancer of the kidneys and bladder; losses during hemodialysis; uterine fibroids, endometriosis, hyperpolymenorrhea, cervical cancer; nosebleeds
- congenital deficiency of iron in the body (prematurity, birth from multiple pregnancy, severe iron deficiency anemia in the mother, pathological bleeding during pregnancy and childbirth, fetoplacental insufficiency)
- alcoholism (the mucous membrane of the stomach and intestines is damaged, making it difficult to absorb iron)
- use of medications: non-steroidal anti-inflammatory drugs (diclofenac, ibuprofen, aspirin) reduce blood viscosity and can promote bleeding, in addition, these drugs can provoke the occurrence of stomach and duodenal ulcers; antacids (Almagel, Gastal, Rennie) reduce the production of hydrochloric acid, which is necessary for effective absorption of iron; iron-binding drugs (desferal), these drugs bind and remove free iron and iron in ferritin and transferrin, and in case of overdose can lead to iron deficiency states
- donation (with donations more than 4 times a year, iron deficiency develops)
- disruption of transferrin synthesis. Transferrin is an iron transport protein that is synthesized in the liver.
Normal hemoglobin level in the blood: in women – 120-140 g/l, in men – 130-160 g/l
Diagnostic methods
To determine the stage of anemia, the World Health Organization recommends using the following methods:
- measurement of cyanmethemoglobin;
- HemoCue® system.
In the cyanmethemoglobin method, a fixed amount of blood is dissolved in a reagent and the hemoglobin concentration is determined at a set time interval using an accurate, well-calibrated photometer. Cyanmethemoglobin measurement is a standard laboratory method for the quantification of hemoglobin.
The HemoCue® system is based on the cyanmethemoglobin method and has been shown to be stable and reliable when used in the field. When determining hemoglobin concentrations, the source of the blood sample should also be considered. Some studies suggest that hemoglobin values measured from capillary blood samples are higher than those measured from venous blood samples, which may lead to false-positive results.