What are hemorrhoids
Hemorrhoids (from the Greek haima - “blood”, roe - “flow”) are one of the most common diseases in proctology, which is based on the pathological condition of the cavernous plexuses of the rectum, accompanied by stagnation of blood in them. Hemorrhoids are manifested by periodic bleeding from the nodes, their prolapse from the anal canal and frequent inflammation. Men and women are equally susceptible to hemorrhoids
Classification of hemorrhoids
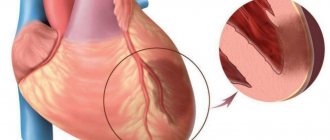
Internal hemorrhoids. With internal hemorrhoids, there are varicose hemorrhoidal veins, which are located deep in the anal canal, so such hemorrhoids are not visible during a normal examination. In order to see them, you have to resort to special research methods: anoscopy, rectoscopy. Also, such nodes can be identified during digital rectal examination. Such a sign of the disease as prolapse of hemorrhoids can cause bleeding when they are injured during the act of defecation. With significant weakness of the ligamentous apparatus of the rectum, such nodes fall out during defecation or significant straining. In addition, the internal nodes, when they fall out and spasm of the anal sphincter, can be infringed. Most often, the first signs of internal hemorrhoids are bleeding.
External hemorrhoids. In this type of hemorrhoid, the hemorrhoids are marked externally and should not be confused with prolapsed internal hemorrhoids. Most often, external nodes manifest as thrombosis. As a rule, bleeding from external nodes does not occur, since they are not injured during defecation. Such hemorrhoids hurt and cause discomfort during bowel movements. But constant stagnation of blood in them can lead to the formation of blood clots in them. Externally, the external hemorrhoidal node can be of different sizes, from 3 mm or more, which depends on its blood supply. An external hemorrhoid is usually covered by skin, while a prolapsed internal hemorrhoid is usually covered by the mucous membrane of the anal canal.
Combined hemorrhoids. As the name implies, with combined hemorrhoids, the patient has a combination of external and internal hemorrhoids.
The occurrence of hemorrhoids
Normally, all people have external and internal hemorrhoidal venous plexuses under the mucous membrane of the anal canal, which are similar in structure to the cavernous tissue of the genital organs. They play a significant role in retaining intestinal contents, ensuring complete closure of the anal canal when they are filled with blood. As a result of the influence of a number of factors, most adults experience an increase in hemorrhoidal nodes, and hemorrhoids begin to develop.
Factors influencing the development of hemorrhoids: constipation, straining; pregnancy, childbirth; hereditary factors; sedentary lifestyle; prolonged standing or sitting; excessive physical activity; practicing some sports (horse riding, cycling, weightlifting); lifting weights; overweight; hot, spicy food; drinking alcohol; prolonged exposure to heat (sauna, hot bath); prolonged diarrhea (diarrhea).
Brief classification
Hemorrhoids are a painful enlargement of the cavernous cavities of the venous plexus of the rectum.
These cavities fill with blood when straining, performing the function of a kind of “pillow” that protects tissues from the traumatic effects of solid feces during the act of defecation. Hemorrhoids are a pressing problem for humanity; about 60% of Earth's citizens experience at least one episode of painful enlargement of hemorrhoids throughout their lives. It must be said that this percentage is much higher in countries that are commonly called civilized.
Anatomically, internal hemorrhoids - hemorrhoidal nodes in the distal (terminal) part of the rectum, and external hemorrhoids , when the nodes are located outside in the anal area.
According to the nature of the course, hemorrhoids can be acute , associated with thrombosis of the hemorrhoidal veins, and chronic , caused by constant overflow of distended veins with blood.
Timely diagnosis
To avoid hemorrhoids and possible complications, it is necessary to identify the disease at its earliest stages. Internal hemorrhoids can be detected by digital examination of the rectum, feeling for compaction of the hemorrhoidal veins. But such an examination is effective only when the nodes are located low. If the cones are located high up, then only modern equipment can help in diagnosing the disease. Anoscopy and sigmoidoscopy are the most common techniques. In the first case, a special tube with an optical device is used, which allows one to examine the rectal mucosa over a ten-centimeter length. If the hemorrhoids are located even higher, then you cannot do without the help of a sigmoidoscope. The rectum at a distance of 25 cm will be “in full view” to the doctor. If the patient states that during defecation he himself observed the prolapse of nodes, then a diagnosis can be made based on this reliable fact. True, unfortunately, for the patient the stage of the disease in this case is later, and therefore less treatable.
Reasons for the development of hemorrhoids in women
Chronic hemorrhoids in women, as a rule, develop after 30 years of age; with age, the risk of developing the disease increases. Women suffer from dilated hemorrhoidal veins four times less often than men. However, the risk increases in the presence of permissive factors: • chronic constipation; • prolonged sitting on the toilet; • obesity; • sedentary work, sedentary lifestyle; • diseases occurring with chronic cough; • diseases of the pelvic organs.
A typical cause of acute hemorrhoids in women is pregnancy or childbirth. In such cases, adequate conservative treatment leads to the disappearance of the problem. However, if therapy was untimely or careless, the disease becomes chronic.
What is prohibited if cavernous nodes have fallen out
If a hemorrhoidal node has fallen out, the patient is prohibited from performing the following manipulations:
- Make sudden movements (to reduce the load on the rectal sphincter, you need to lie on your back and limit walking as much as possible).
- Using toilet paper (after visiting the toilet, hygiene procedures are carried out exclusively with water and soap).
- Wear clothes that are tight in the perineal area (squeezing and injury to the node occurs).
- Sitting and lying on soft surfaces (the mattress or seat should be fairly firm).
- Staying on the toilet for a long time (if it is difficult for the patient to empty his bowels on his own, you can give a cleansing enema).
Symptoms of the acute form of the disease
Symptoms of acute hemorrhoids in young women are most often associated with pregnancy or childbirth. The appearance of an enlarged hemorrhoid constipation characteristic of this period .
Acute dilatation of hemorrhoidal veins manifests itself with sharp pain , which becomes unbearable during bowel movements. In addition, the pain syndrome can intensify while walking, as well as with increased intra-abdominal pressure during straining, coughing, laughing, and hiccups.
Another characteristic sign of the acute form of the disease is bleeding from the dilated veins of the rectum. This symptom manifests itself as fresh blood on the surface of the stool.
Often hemorrhoids in women are combined with anal fissure. In such cases, blood stains on toilet paper and underwear appear even more often after defecation.
Complications of hemorrhoids
If the pathology is not diagnosed on time, the risk of complications increases. In advanced stages, conservative treatment does not make sense, so surgical intervention will be required. The rehabilitation period will be many times longer.
Complications of hemorrhoids include thrush and dysbacteriosis. The microflora in a woman’s body is disrupted, and an infection develops that spreads throughout the body.
Complications also include:
| thrombosis; | A general inflammatory process in the body begins, varicose veins progress. After each act of defecation, bleeding from the anus opens. Blood clots form, which is extremely dangerous for the patient’s life. |
| anal fissures; | The inflammatory process and internal hemorrhoids lead to the formation of anal fissures. Soft tissues are damaged and expand. The risk of cryptitis increases. |
| paraproctitis; | Hemorrhoids that were not diagnosed and treated on time lead to acute and chronic paraproctitis. Harmful bacteria accumulate on the rectal mucosa and pus forms. |
| anemia; | One of the most dangerous complications is called anemia. The patient loses a lot of blood from hemorrhoidal tumors, and hemoglobin decreases. The woman feels chronic fatigue and rapidly loses weight. |
| ulcerative colitis; | Against the background of acute hemorrhoids, a concomitant disease develops. We are talking about ulcerative colitis. Ulcers appear in the body, the mucous membrane of the rectum becomes thinner, destroyed and injured. |
| purulent infections; | Pus collects in the anal fissures and the woman becomes infected. Infection can also occur during a period when the patient does not follow the rules of personal hygiene. |
| benign and malignant neoplasms; | Lack of treatment, compliance with personal hygiene and sanitation standards often provoke the growth of malignant and benign tumors. With hemorrhoids, tumors rapidly increase in size, so it is worth starting a course of treatment immediately. |
Stages of development of chronic pathology
With chronic hemorrhoids, the pain syndrome is much weaker. Often the only signs of chronic pathology are itching around the anus blood appearing on the surface of the stool from time to time .
The stages of development of internal hemorrhoids differ using the most objective symptom - the degree of stretching of the dilated veins: I. The hemorrhoid is constantly located in the intestinal cavity II. The knot falls out when straining and resets itself back III. The patient has to adjust the knot with his hands IV. One or more hemorrhoids are constantly on the outside and cannot be reduced
At any stage, thrombosis of the dilated veins of the rectum , in which case severe pain syndrome characteristic of an acute attack occurs.
With a long course of the disease, the risk of complications increases ( anemia, neurasthenia, anal fissure, etc. ).
Clinical prognosis
The overall clinical prognosis is always favorable. Modern proctological methods make it possible to successfully treat internal hemorrhoids even at the most advanced stages.
The disease can pose a threat to life only if the hemorrhoids become necrotized with the addition of blood poisoning, but this is only possible in the case of a long, persistent and conscious refusal of the patient to receive medical care.
Surgeon-coloproctologist, surgeon of the highest category. Rakhmatullin Andrey Albertovich
Diagnosis and choice of treatment tactics
Diagnosis of hemorrhoids is carried out by a proctologist using a digital examination. Symptoms such as bleeding, pain, and the sensation of a foreign body in the rectum occur with cancer, as well as with other pathologies of the lower intestine.
Therefore, the general list of examinations may include sigmoidoscopy or colonoscopy, as well as laboratory tests.
At the final stage of diagnosis, treatment tactics are chosen. Acute hemorrhoids are treated conservatively, and in the chronic form of the disease they resort to surgery, giving preference to minimally invasive treatment methods.
The exception is cases when surgery is temporarily contraindicated. For women, this is pregnancy, the postpartum period, as well as situations when it is necessary to stabilize the general condition of the patient. This situation can arise during acute infections or during exacerbation of severe chronic diseases.
Features of conservative treatment
The type of treatment determined for the patient by the physician depends on the degree of development of thrombosis. Therapeutic stages are relevant for thrombosis of stages 1 and 2, as well as during pregnancy. During the treatment the following tasks are solved:
- relieving severe inflammation;
- elimination of swelling and pain;
- relieving tension from the anal sphincter;
- dissolution of blood clots and prevention of thrombus formation.
Conservative treatment involves the use of medications or ointments that dissolve the blood clot localized in the node. The choice in favor of one or another means takes into account the location where the nodes are located. The course can also be supplemented with various painkillers that block the pain syndrome that occurs during thrombosis. Naturally, during pregnancy the range of drugs available for treatment is significantly reduced.
Methods for treating hemorrhoids without surgery
Conservative treatment of painfully enlarged hemorrhoids should be carried out comprehensively, affecting all factors contributing to the development of the disease. It is necessary to normalize the stool, because constipation and diarrhea equally seriously injure the inflamed node.
If the cause of hemorrhoids is an attack of diarrhea, every effort is made to cure the disease that caused the stool disorder. Constipation is fought with a diet that includes a large amount of dietary fiber (prunes, dried apricots, oranges, apples). For persistent constipation, mild laxatives (Duphalac) are prescribed.
In order not to irritate the intestines, spices, salt, vinegar, smoked foods, as well as carbonated drinks and alcohol are excluded from the diet.
The pain increases the spasm of the internal sphincter, which contributes to stagnation of blood in the veins. To relieve pain and spasms, use warm baths with potassium permanganate or herbal decoctions.
Painkillers, antispasmodics, blood thinners, and medications that promote tissue regeneration are prescribed as drug therapy. Preference is given to “local” therapy: ointments are used for external nodes, and suppositories for internal nodes.
Attention! The prescription of drugs depends on the location of the hemorrhoid, the stage of development of the disease, the phase of the process, the presence of concomitant diseases and the general condition of the body. Therefore, we recommend not to self-medicate, but to consult a doctor in a timely manner.
Treatment of stage I disease
Yes, at this stage the nodules have not yet appeared, but this does not mean that there is no need to worry. On the contrary, timely treatment prescribed by a proctologist will prevent further loss.
In most cases, complex therapy is prescribed, including the use of medications. Ointments for external use and rectal suppositories are successfully used.
Table No. 1. Popular effective remedies for the treatment of hemorrhoids
| Name of the drug | Active components and action | Features of application |
| Heparin ointment | The active ingredient is heparin, which is an excellent anticoagulant | Eliminates the symptoms of hemorrhoids in acute and severe cases of the disease. |
| Gepatrombin G (gel) | Heparin is an anticoagulant; prednisolone is a glucocorticoid with an anti-inflammatory effect; Lauromacrogol is an anesthetic. | Prescribed for treatment and preventive purposes. |
| Sea buckthorn candles | Sea buckthorn oil has many properties: antibacterial, regenerating, antitumor. | Numerous reviews confirm the effectiveness and safety of this product. |
| Fleming's ointment | A homeopathic remedy that contains healing extracts of calendula, witch hazel and aesculus. Has a powerful bactericidal and anti-inflammatory effect. | Improvements are observed a few days after the start of use. |
| Relief (rectal suppositories) | Phenylephrine hydrochloride is a vasoconstrictor, hemostatic agent; shark liver oil is rich in vitamins, microelements, has an antibacterial and immunomodulatory effect; Cocoa butter softens, reduces swelling and inflammation. | Gives a lasting therapeutic effect. |
| Anuzol (rectal suppositories) | An extract from belladonna leaves helps when hemorrhoids hurt a lot and is an active healing substance; xeroform relieves inflammation that occurs in blood vessels and strengthens their walls; glycerin dries mucous tissues and eliminates inflammation. | The stool is colored black, which should not cause concern. |
| Troxevasin (gel) | Troxerutin is an active venotonic, has angioprotective, anti-inflammatory, anti-edematous and antioxidant effects. | They are often prescribed at later stages, when the node has already come out. |
In case of significant venous insufficiency, a specialist may recommend therapy using systemic venotonic agents.
Radical treatment of pathology
Minimally invasive methods
Doctors treat chronic hemorrhoids with surgical methods. At the initial stages of the disease, preference is given to minimally invasive techniques, which are carried out on an outpatient basis (without placing the patient in a hospital) and provide for a short rehabilitation period.
An important advantage of low-traumatic operations is a short list of contraindications. The list of methods that are suitable for most patients includes: • sclerotherapy (injection into dilated veins of substances that cause “soldering” of the walls of dilated veins); • infrared coagulation (cauterization of the leg of the node); • ligation of the internal hemorrhoid with latex rings.
Sclerotherapy and infrared coagulation are used at stages I – II of the development of internal hemorrhoids. The effectiveness of these methods at stage I is 85%, and at stage II – about 72%. If the node is ligated with latex rings, the effectiveness exceeds 93%.
Operation hemorrhoidectomy
Hemorrhoidectomy is the removal of enlarged hemorrhoids using surgical methods, that is, using a scalpel.
Such treatment must be carried out in a hospital. The rehabilitation period is much longer and is less well tolerated by patients. Therefore, surgical removal of nodes is carried out only in the last stages of the disease , when minimally invasive techniques are no longer effective.
Hemorrhoidectomy can be combined with disarterization of hemorrhoids under ultrasound control. This method is often used for stage III internal hemorrhoids.
The choice of surgical intervention method depends on the number of enlarged nodes, their location, as well as the presence of complications and concomitant pathologies.
Critical risks for the disease without treatment
There is a certain chance of hemorrhoidal thrombosis going away on its own if, when the blood walls are destroyed, the blood clots leave the hidden or external node. However, such luck is unlikely - often qualified treatment for thrombosis of hemorrhoids is required. Without timely treatment of thrombosis, the risk of developing the following critical complications is high:
- necrosis in the node - the death of inflamed areas with the formation of ulcers in their place;
- perarectal abscess - suppuration in the subcutaneous part of the anal area.
When treating thrombosis of hemorrhoidal nodes, it is possible to avoid death, which can result from blood poisoning.
Treatment during pregnancy and after childbirth
Treatment of hemorrhoids in pregnant women and in the early postpartum period does not involve surgical intervention. The fact is that the reasons for the dilation of the veins of the rectum during this period are physiological in nature: • changes in hormonal levels; • increased intra-abdominal pressure; • increase in circulating blood volume; • straining during childbirth.
After childbirth, hormonal levels gradually normalize, which leads to the disappearance of the tendency to constipation. The volume of circulating blood decreases, intra-abdominal pressure decreases, the body's defenses are restored and all conditions for recovery are created.
Therefore, in most cases, a painful node that occurs during pregnancy or after childbirth disappears on its own under the influence of standard methods of conservative treatment.
Attention! When conservatively treating hemorrhoids in pregnant women, as well as in women during lactation, care should be taken. Some active ingredients of topically applied drugs still enter the bloodstream and can harm the child. Therefore, treatment must be done under the supervision of a physician.
We care about your health
Hemorrhoids in women are a fairly common ailment that requires urgent treatment. Its symptoms coincide with a similar disease in men. However, according to statistics, women suffer from this unpleasant disease much more often. This is explained by the lifestyle and structural features of the body of representatives of the fairer sex.
Let's take a closer look at the symptoms and causes of hemorrhoids, treatment of this disease in women and preventive measures.
Symptoms of hemorrhoids in women
The disease does not appear immediately, but develops gradually. Symptoms vary widely and depend on the stage of the disease.
Signs of hemorrhoids in women most often include the following:
- sensation of a foreign body in the anal canal area;
- burning and itching in the anus;
- bleeding from the rectum;
- prolapse of hemorrhoids;
- severe pain in the anus;
- heaviness in the stomach, bloating;
- lack of sensation of complete bowel movement.
With the development of severe inflammation, an exacerbation of the disease occurs, which is accompanied by high fever and blue discoloration of the hemorrhoids.
Causes of female hemorrhoids
Female hemorrhoids can be caused by many factors. Let's look at the most common causes that contribute to the onset of the disease.
- 1. Pregnancy and childbirth. The uterus enlarges during pregnancy and puts strong pressure on the vessels, causing blood stagnation. During childbirth, stagnation increases, pushing is accompanied by increased blood flow to the pelvic veins. This contributes to the development of hemorrhoids.
- 2. Menstrual cycle. During menstruation, a large volume of blood flows to the pelvis, as a result of which the blood vessels become overfilled - there is a risk of hemorrhoids.
- 3. Poor nutrition. The lack of plant fiber in the body and eating disorders can lead to constipation, and this disrupts natural intestinal motility. The result is the development of hemorrhoids. A big risk factor can be a variety of diets that disrupt the diet necessary for the body.
- 4. Profession. Professional activities associated with prolonged sitting or standing positions disrupt the circulation of arterial and venous blood in the pelvic area, which leads to blood stagnation.
- 5. Stress. The occurrence of the disease largely depends on psychological reasons. Women are more likely to be exposed to stress, endure it much more severely and experience severe emotional stress.
- 6. Increased physical activity, lifting weights that do not correspond to the body’s capabilities.
- 7. A sharp decrease in body weight.
- 8. Unconventional sex.
This is not a complete list of the causes of hemorrhoids in women. By adopting a healthy lifestyle and proper nutrition, you can avoid the development of the disease.
Types of hemorrhoids
Hemorrhoids in women can be divided into several types. Each type has its own symptoms and requires specific treatment.
Interior. The disease manifests itself in inflammation of the veins inside the anal canal and develops painlessly. This is explained by the fact that there are no pain receptors in this place.
External. The veins in the anus become damaged, which causes severe pain and itching. In such cases, medical intervention is required.
Combined. It is a combination of internal and external views. The disease may be accompanied by anal fissure, prolapse or thrombosis of hemorrhoids, and this can cause severe bleeding. In such cases, treatment of hemorrhoids in women cannot be delayed - try to see a doctor immediately.
Stages of hemorrhoids in women
In medical circles, there are four stages of hemorrhoids in women.
At the first stage, a slight compaction is felt at the entrance to the rectum. After defecation, itching and burning appear in this place. If you see a doctor right away, the disease can be cured in two to three weeks.
The second stage manifests itself in an increase in hemorrhoidal cones. They become dense and cause pain. When defecating, the lumps may come out and then come back. Discharge in the form of blood or inflammatory fluid appears from the rectum, which is accompanied by unbearable itching and discomfort.
At the third stage, nodes fall out. This happens when visiting the toilet, strenuous physical activity, or lifting heavy objects. Pain haunts a woman constantly: when she sits, walks and even lies.
The fourth , advanced stage is accompanied by severe bleeding during bowel movements, lumps of different sizes on the inside and outside of the anus, the inability to reduce hemorrhoids, and the appearance of blood clots.
The first stage of the disease is treated at home without hospitalization. On the second and third, hospital treatment will be required. The fourth stage of the disease can only be cured with surgery.
Treatment of the disease
Diagnosis and treatment of female hemorrhoids is carried out by a proctologist. He conducts an examination, prescribes therapy and provides advisory assistance.
In the initial stages, ointments, rectal suppositories, and gels help. They relieve pain, irritation, itching and tingling. For oral administration, tablets are prescribed to make it easier to go to the toilet, painkillers, antibiotics (if a bacterial infection is detected), phlebotropic drugs, etc.
For the treatment of female hemorrhoids, special procedures are very effective:
- infrared coagulation - the effect of infrared radiation on hemorrhoids (cures the disease in the initial stages);
- sclerotherapy - the introduction of a sclerosing drug into the inflamed nodes (effective in the treatment of internal hemorrhoids);
- minimally invasive methods - treatment of the disease through latex ligation (when enclosing each node in a ring leads to the falling off of the lump in two to three weeks), ligation of hemorrhoidal arteries (HAL procedure), etc.;
- Hemorrhoidectomy is a surgical operation to remove nodes.
You should not try to diagnose or self-medicate on your own. Hemorrhoids can easily be confused with another serious rectal disease and cause irreparable harm to the body.
Prevention of hemorrhoids in women
To protect yourself from hemorrhoids, follow simple rules for its prevention:
- eat foods rich in plant fiber;
- minimize spicy and spicy foods, alcohol;
- lead an active lifestyle;
- avoid strong strain during bowel movements;
- sit only on hard chairs;
- take breaks during sedentary work;
- Walk more during pregnancy.
Preventing the disease will help avoid unpleasant consequences. A timely visit to a doctor will allow you to cure hemorrhoids quickly and without any complications.
Reviews from patients about the operation
We analyzed patient reviews about the rehabilitation period after hemorrhoid removal. The analysis showed that the severity of pain, difficulty with defecation and bleeding after surgery depends on the size and number of nodes removed.
Patients who have consulted a doctor with a single small node speak of surgical intervention as a completely tolerable procedure, with a short rehabilitation period.
When it comes to several large nodes, treatment will be lengthy. If the doctor recommends a minimally invasive method, you will have to remove one node per week, so the healing process will take several weeks. A surgical operation will remove all pathological elements at once, but in this case the rehabilitation period may also take several weeks.
Therefore, we recommend that you consult a doctor in a timely manner in order to intervene at an early stage of the disease. Additional information about preparing for surgery and rules of behavior during the rehabilitation period can be read in the article “Treatment of hemorrhoids in men.”
Relapse Prevention
If you have already had hemorrhoids removed, there is an increased risk of the disease returning. To protect yourself from relapse, you should follow the recommendations of doctors: 1. Watch your stool (it is advisable to achieve daily morning bowel movements). 2. Be careful with “weight loss” diets (see point 1). 3. If you have a sedentary job, do gymnastics regularly. 4. Treat diseases of the gastrointestinal tract and pelvic organs (gastroenterology, urology, gynecology) in a timely manner. 5. Avoid physical and nervous overload.
Nature has prepared a woman for childbirth, so the venous vessels of the rectum in women are more resistant to stress than in men. If you follow the rules, the disease will not return.
First aid
If a patient has a prolapsed hemorrhoid, it is necessary to urgently provide first aid, which is aimed at relieving pain and alleviating the condition in general.
Ice helps reduce pain when nodes fall out, as it reduces the conduction of nerve impulses to the pain center
First aid algorithm:
- Apply ice to the affected area, after wrapping it with several layers of cloth to avoid frostbite of the soft tissues of the rectal area.
- Taking a sitz bath with a temperature of at least 18 degrees, the duration of the procedure is 15 seconds.
- Taking medicinal baths with the addition of medicinal herbs (chamomile, oak bark, calendula) will help relieve inflammation and reduce pain. You need to take a bath in a sitting position with a water temperature of 37 degrees for 15 minutes.
Is it possible to cure chronic hemorrhoids with folk remedies?
Unfortunately, chronic hemorrhoids cannot be cured using conservative methods. “Folk” methods give a short-term effect. Similar results will be obtained with “home” drug treatment.
The unpleasant symptoms of the disease may disappear for a while, but the disease will develop unnoticed by you. In the future, the following complications may develop: • anal fissure; • anemia; • nervous exhaustion; • infectious processes (proctitis, paraproctitis, etc.).
It should also be noted that under the mask of hemorrhoids a deadly disease such as rectal cancer . Therefore, if alarming symptoms appear, you should urgently consult a doctor to find out an accurate diagnosis and begin adequate treatment.
Don’t waste time on self-medication, come to an appointment with a proctologist!