Vascular patterns on the skin in the form of stars, nets, bluish-violet swellings resembling tangled ropes are not only an aesthetic discomfort. They may be a sign of the initial stage of venous disease or dysfunction of internal organs. Even if such cosmetic defects do not cause any particular inconvenience, it is necessary to find out the cause of their appearance and rule out serious medical problems.
Why do spider veins develop?
There are several theories:
- pathological venous reflux
- micro valve failure
- hormonal influence
- activation of vasoactive mediators under the influence of a variety of conditions, which leads to vascular reorganization
- connective tissue abnormalities.
In general, such a vascular reaction can be caused by a number of diseases and provoking external and internal factors:
- Hormonal changes: pregnancy, taking COCs, corticosteroids.
- Genetic predisposition.
- Violation of the venous system of the lower extremities.
- Symptomatic spider veins in liver cirrhosis, carcinoid, collagenosis, HIV, mastocytosis, cardiovascular disease.
- Congenital diseases and syndromes.
- Physical, mechanical stress: solar, radiation, temperature, injury.
Telangiectasia often develops with age due to the fragility of blood vessels. Their appearance is also influenced by an unhealthy lifestyle.
Undesirable consequences
After sclerotherapy of veins, the following complications may develop:
- Folliculitis;
- Purulent-septic diseases;
- Nicolau syndrome (skin necrosis at the site of sclerosant injection);
- Allergic reactions;
- Deep vein thrombosis;
- Pulmonary embolism;
- Neurological complications (transient cerebrovascular accident).
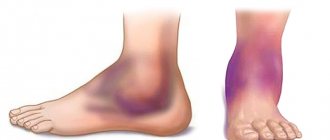
Sometimes swelling of the legs develops after sclerotherapy, intradermal and subcutaneous hemorrhages (bruises), hyperpigmentation, and new “stars”. The so-called recurrent telangiectasias are a reaction in the form of the appearance of a bright red vascular network. It appears on the third to fifth day after sclerotherapy and persists for 6-12 months. After this, most telangiectasias disappear on their own.
The thickening of the veins after sclerotherapy goes away without treatment within a month. If after sclerotherapy your leg hurts or lumps (bumps) appear, this is not a complication, but a predictable consequence of the procedure. During a follow-up examination, the phlebologist pierces them with a very thin needle and removes the accumulated fluid. After this, the “bumps” decrease and the pulling sensation goes away.
It is also normal for slight swelling to occur after sclerotherapy if it persists no longer than four days. Intradermal hemorrhages occur as a result of the penetration of red blood cells through the damaged vein wall as a result of the action of a sclerosing drug. Prolonged resorption of hematomas can lead to persistent skin hyperpigmentation and pain in patients.
After sclerotherapy, complications may occur within a month. Pigmentation disappears on its own within a few months. In a small number of patients, hyperpigmentation persists for more than a year. If bruises do not go away for a long time, you should immediately contact the doctor who performed the procedure. He will conduct an examination and perform an ultrasound to make sure there are no complications.
What can spider veins lead to?
In themselves, such formations do not pose a threat to health. In rare cases, they are accompanied by pain, swelling or bleeding, causing physical discomfort. Telangiectasia can remain only an aesthetic problem if the factor that caused it is eliminated.
However, there are situations when altered vessels are a nonspecific sign of chronic venous insufficiency or severe somatic pathology. It is impossible to make a diagnosis on your own. Finding out the cause of telangiectasia and starting treatment is the doctor’s task.
Rehabilitation period
The process of treating varicose veins using sclerotherapy is not a one-step process. To achieve results, a certain rehabilitation period must take place. It is individual for each patient and depends on the characteristics of a particular organism. The main condition for high-quality recovery is the patient’s self-control and discipline.
After sclerosis, local aseptic inflammation occurs in the venous wall (without the participation of microorganisms). During this period, the patient may experience pain in the leg, swelling may develop, and minor hemorrhages may appear. This is a normal course of the recovery period. For severe pain, your doctor may prescribe acetaminophen. You should refrain from taking non-steroidal anti-inflammatory drugs. Swelling after sclerotherapy decreases when the patient lies down for 15 minutes with his leg elevated at an angle of 15°.
During the recovery period after sclerotherapy, bruises may appear at the injection sites. They first have a characteristic bluish color, but over time they become yellow. Approximately 7-10 days after the procedure, the skin acquires its normal color. Wearing compression stockings can prevent bruising and speed up the process of bruising. In 5-10% of cases, hyperpigmentation of the skin occurs at the injection sites of drugs during the recovery period after sclerotherapy. It does not require treatment and goes away on its own after 2-3 months.
Make an appointment
How and why do varicose veins develop?
Blood flows through the veins in only one direction - up to the right side of the heart. Valves on the walls of blood vessels prevent its reverse movement. If they fail, the blood stagnates, stretches and deforms the veins.
Risk factors include:
- pregnancy;
- physical inactivity;
- constant static loads;
- obesity;
- lifting weights;
- dyshormonal conditions;
- frequent constipation, lack of fiber in the diet;
- high heels.
Varicose veins are a disease with a genetic predisposition. The failure of the vessel wall and valve apparatus is inherited. The pathological process develops under the influence of provoking factors.
What can dilated veins lead to?
Without treatment, varicose veins progress, chronic venous insufficiency develops, and clinical symptoms appear:
- swelling of the legs in the evening, then they become permanent;
- muscle cramps;
- feeling of heaviness, burning, bloating in the limbs, itching, fatigue.
In advanced cases, scar tissue grows in the subcutaneous layer, venous ulcers, hyperpigmentation, and eczema appear. Dangerous complications - thrombophlebitis, bleeding from varicose nodes, phlebothrombosis.
What treatment methods are there?
The goals of treatment are to restore blood flow, eliminate aesthetic defects, and prevent complications. It is impossible to return a damaged vein to its original state using conservative methods. Such a vessel must be excluded from the bloodstream. Then healthy veins will take over its function.
Minimally invasive surgical methods are used to remove dilated veins and vascular networks:
- Sclerotherapy is the introduction of a special adhesive agent into the damaged vessel.
- Miniphlebectomy - removal of a vein through a pinpoint incision (1-2 mm).
- Transdermal (percutaneous) coagulation of vascular defects with a laser.
- Radiofrequency obliteration of veins is a radio wave effect on a modified vessel of the limb.
- Endovenous laser coagulation is intravascular laser irradiation using a flexible light guide.
The choice of method depends on the clinical picture, medical history, and instrumental studies (ultrasonic angioscanning).
To prevent relapse, it is necessary to eliminate provoking factors, wear compression stockings, take phlebotropic drugs, and see a phlebologist.
Historical reference
The use of sclerotherapy
as a method of treating varicose veins dates back more than 100 years.
The first mention of sclerotherapy dates back to 1682: it was then that Dr. Zolikofer introduced acid into the lumen of the vein to form thrombosis. Scientists Debout and Cassagnac published their research materials in 1853, which provided data on the successful treatment of varicose veins
using iron perchlorate.
The scientist Desgrange in 1860 used iodine and tannin to treat varicose veins
in 16 patients.
However, all methods of using sclerosing agents to treat varicose veins
had side effects at the time, allowing surgical treatment to take precedence over
sclerotherapy
.
Only at the beginning of the 20th century new data appeared on the successful treatment of varicose veins
with mercury-based drugs, but these publications did not influence the development
of sclerotherapy
.
In 1946, the drug tetradecyl sulfate (fiberwein) was discovered, which is currently successfully used in sclerotherapy
.
New rise of sclerotherapy
experiences in 1960 when scientist George Fegan reports successful
treatment of varicose veins
in 13,000 patients.
Fegan outlined the basic principles of successful sclerotherapy
: precise injection of the drug into the lumen of the vein, sufficient contact time of the drug with the vein wall, mandatory subsequent compression with elastic materials.
The technique of vein sclerosis
is being adopted by medical communities in leading European countries.
treatment of varicose veins gradually began to improve
and other vascular diseases.
In particular, the duplex angioscanning technique began to be used not only for diagnosing vascular diseases - with its help it became possible to control the administration of sclerosant, as well as evaluate the effectiveness of the therapy. Scientists Knight and Thibault studied the possibility of
ultrasound-guided
sclerotherapy echosclerotherapy
), and the research of the founders of the
foam sclerotherapy
, Cabrera and Monfro, became the basis for modern
sclerotherapy
.
What is sclerotherapy?
The method involves the injection of a sclerosing drug into a vein in the form of liquid or foam. As a result, the vessel turns into a thin fibrous cord, which resolves over time. In fact, the vascular defect is removed, as during surgery, but in a minimally invasive way that does not require hospitalization and a long recovery period.
This type of treatment is recommended for all types of dilated veins. The indication for sclerotherapy of the vascular network is the patient's dissatisfaction with a cosmetic defect, bleeding from telangiectasis.
How is the procedure done?
- The puncture site is first marked with the patient in an upright position.
- The vein is punctured with an ultra-fine needle in the supine position. The location of the needle in the vein is controlled by the flow of dark blood into the syringe.
- The drug is administered very slowly. After removing the needle, compression bandaging is performed along the treated vein, the timing of which is determined by the doctor individually.
- Sclerotherapy of complex veins is performed under ultrasound guidance. At the final stage, a one-hour walk is recommended. Several injections can be given in one session.
Contraindications
Relative contraindications – pregnancy, severe somatic pathology. Among the absolute ones:
- thrombosis;
- allergy;
- infectious process;
- long-term immobilization.
How does it help?
This treatment method helps to achieve cosmetic and medical results. The changed vessels disappear, the legs look attractive again. From a medical point of view, blood flow improves, pain, swelling in the legs, ulcers are prevented, and the progression of the disease is reduced.
Microsclerotherapy
Cosmetic sclerotherapy for spider veins (microsclerotherapy) allows you to get rid of aesthetic troubles associated with the presence of small vascular networks on the legs. In our clinic, until the full aesthetic effect is achieved, scleratherapy of veins is carried out, the reviews are very positive, especially after using special devices for illumination (venovisor). Our clinic employs experienced specialists in sclerotherapy of spider veins and venous networks. The procedure is carried out with the finest needles using certified Western-made drugs. The procedure is effective, painless and does not interfere with work ability. A good cosmetic result is achieved in most cases within 3-6 weeks of sclerotherapy.
Why is it better to contact the Central Clinical Hospital of the Russian Academy of Sciences?
- Doctors of the highest category, doctors and candidates of medical sciences work with patients.
- The clinic has extensive diagnostic capabilities: a multifunctional laboratory, expert-level equipment, doctors of almost all medical specializations.
- The effectiveness of treatment of vascular pathology in the clinic corresponds to the experience of the world's best clinics, but the cost is significantly lower.
- There are only positive reviews from patients and colleagues about our work.
If you are looking for where to undergo sclerotherapy of the veins of the lower extremities in Moscow, contact the Central Clinical Hospital of the Russian Academy of Sciences. The final price for the procedures can be found out during a consultation with a doctor. Make an appointment by applying on our website.
Results of vein sclerotherapy in our center. Photos before and after treatment
The result of sclerotherapy (removal) of spider veins
The result of sclerotherapy for spider veins in Moscow. Photos before and after treatment
The result of sclerotherapy (scleroobliteration) of varicose veins with Dr. Raskin V.V.