Features of resuscitation
Resuscitation must be started in adults and children, without waiting for the arrival of ambulance specialists, when symptoms appear: lack of pulse in the carotid arteries, lack of breathing, the skin acquires a gray-bluish tint, the pupils are dilated and do not respond to light.
- Place the patient on the floor or other hard, flat surface.
- Tear or cut outer clothing to provide access to the chest.
- Tilt the patient's head back as far as possible, place one hand on the forehead, and with the other push the patient's lower jaw forward. This technique ensures airway patency.
- Make sure there are no foreign bodies in the mouth and throat, and if necessary, remove mucus with a quick movement.
Compliance with the rules of resuscitation is a step towards its successful completion.
Breathing “mouth to mouth”. A napkin, a piece of gauze or a handkerchief is placed on the patient’s lips. A deep breath is taken, the lips are pressed tightly to the patient’s mouth. Then they exhale forcefully (for 2-3 seconds), while closing the person’s nose. The effectiveness of artificial ventilation can be seen by raising the chest. The frequency of breaths is 16-18 times per minute.
Indirect cardiac massage. Place both hands on the lower third of the sternum (approximately in the center of the chest), standing on the left side of the person. Energetic pushes are performed towards the spine, shifting the surface of the chest by 3-5 cm in adults, 1.5-2 cm in children. The frequency of pressing is 50-60 times per minute.
When combining mouth-to-mouth breathing and cardiac massage, as well as carrying out activities by one person, it is necessary to alternate 1 breath with 4-5 chest compressions. Resuscitation is carried out until emergency personnel arrive or until the person shows signs of life.
If the patient has regained consciousness, do not leave him alone under any circumstances.
Symptoms
A person with ketoacidosis' condition worsens gradually, usually over 1-2 days or more. The clinical picture is divided into 3 successive stages:
- Moderate ketoacidosis. There is weakness, lack of appetite, thirst, dry skin and mucous membranes, and frequent urination. The smell of acetone appears in the exhaled air.
- Hyperketonemic precoma. Muscle weakness, thirst, dry mouth increases. Abdominal pain, heart pain occur, and decreased vision is noted. The patient is inhibited.
- Ketoacidotic coma. The man loses consciousness. A characteristic rare deep noisy breathing appears with a noticeable odor of acetone in the exhaled air [7].
Hypoglycemic coma
Hypoglycemia is clinically manifested when blood glucose decreases to 2.8 mmol/l or more.
Basic diagnostic signs: rapid development of coma, pronounced moisture of the skin, muscle hypertonicity, clonic-tonic convulsions.
- with any change in behavior in a patient with diabetes (unmotivated or inappropriate actions, confusion), hypoglycemia should be suspected;
- after relief of hypoglycemic coma, ECG monitoring (to exclude MI) and a careful neurological examination (to exclude stroke) are required;
- In any case of hypoglycemia, poisoning with insulin or oral antidiabetic drugs must be excluded.
Medical care for hypoglycemic coma
- Ensure reliable venous access.
- Thiamine chloride (vit. B1) 5% 2 ml intravenously (the administration of thiamine is especially important in patients who abuse alcohol).
- Glucose 40% 60 ml IV (the rate of administration should not exceed 10 ml/min).
- If the patient’s consciousness is not restored within 5-10 minutes and/or the blood glucose level remains below 5.5 mmol/l, re-introduce 40-60 ml of 40% glucose solution intravenously (total dose of 40% glucose solution is not more than 120 ml !).
- Failure to restore consciousness in the patient, despite normalization of blood glucose levels, may indicate the development of cerebral coma (due to cerebral edema due to prolonged hypoglycemia):
- restoration of patency of the upper respiratory tract, evacuation of mucus and/or vomit from the oral cavity, oxygen therapy (oxygen 40-60 vol%);
- mannitol 20% 200 ml IV for 10 minutes, magnesium sulfate 25% 10 ml, dexamethasone 8 mg (0.4% 2 ml) IV.
In case of oral poisoning with hypoglycemic drugs - gastric lavage followed by the administration of enterosorbent (activated carbon or polyphepan) at the rate of 1 g per 1 kg of the patient's weight, and when seeking medical help 6-8 hours after poisoning, also a saline laxative (magnesium sulfate 25 % 50 ml).
After regaining clear consciousness and glycemic levels, leave the patient at home and transfer the asset to a health care facility.
Indications for hospitalization:
- Pathogenesis, clinical picture and care for hypoglycemic and hyperglycemic coma
- if the patient lives alone;
- recurrence of hypoglycemic coma during the day;
- poisoning with glucose-lowering drugs;
- development of cerebral coma (lack of recovery of consciousness in the patient, despite normalization of blood glucose levels).
In case of refusal, the asset is in the health care facility.
Hyperosmolar non-acidotic
Non-ketoacidotic hyperosmolar coma also develops due to acute decompensation of diabetes. It is based on a sharp decrease in insulin levels and loss of fluid from the body. In this case, there is no excessive formation of ketone bodies and acidosis [7].
| Laboratory indicators | Values |
| Blood plasma glucose | >30 mmol/l |
| Blood osmolarity | 400-500 mOsm/l [4] |
In a general blood test, an increase in hemoglobin and hematocrit levels is noted due to a decrease in plasma volume. There is no acetone in the urine [3].
Hyperglycemic coma: emergency care algorithm before the doctor arrives
With this kind of problem, it is extremely important to immediately provide first aid to the patient. So, for diabetic coma, the emergency care algorithm assumes the following:
- The person is placed on a flat surface in a horizontal position.
- The patient is provided with a free flow of fresh air. To do this, remove outer clothing, remove belt, tie, etc.
- The head is turned to the side. Otherwise, the victim may choke on gastric secretions in the event of an attack of vomiting.
- Determine whether the patient is taking insulin injections. If confirmed, conditions are created for introducing the required dosage of the drug into the blood.
- If possible, record the pressure level in order to communicate the obtained data to ambulance workers.
- Before the doctor arrives, the person is given warm, sweet tea.
- If breathing stops or the pulse disappears, the victim is given artificial respiration or chest compressions.
Symptoms
The patient's health deteriorates slowly over 1-2 weeks. At the precoma stage, severe thirst, dry mouth, dryness and decreased skin turgor, and frequent excessive urination are noted.
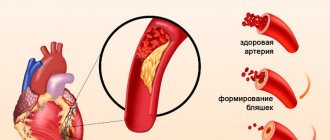
In a coma, as a result of fluid loss, the patient's facial features become sharpened, the eyeballs sink and become soft to the touch. There is no smell of acetone in the exhaled air. Various neurological disorders are characteristic: pathological reflexes, nystagmus, paralysis, epileptiform convulsions. The result of blood thickening can be thrombosis of arteries and veins [3, 7].
Pathogenesis
This condition is caused by a deficiency of insulin in the blood against the background of an increase in glucose concentration. The complication is life-threatening.
The pathogenesis of hyperglycemic coma is explained by impaired metabolic processes in the diabetic body. With insufficient synthesis of insulin, a protein hormone necessary for the utilization of glucose, metabolism is disrupted. Glucose does not penetrate the body's cells, but remains in the blood. Over time, high glucose concentrations occur. This condition is called hyperglycemia. Ketone bodies are formed, gluconeogenesis is activated in the liver, acidosis occurs, and intoxication of the central nervous system occurs. This leads to diabetic coma.
Rarely, hyperglycemic coma occurs before diabetes is diagnosed.
There is a classification that allows you to determine the type of complication depending on the etiology and mechanism of development.
In 80% of diagnosed cases, ketoacidotic coma is diagnosed. Most often it develops in patients with type 1 diabetes. Usually occurs in young people under 20 years of age. According to statistics, 1 out of 3 patients suffering from the juvenile form of the disease experienced a similar condition. This form can transform into hyperosmolar and vice versa.
Hyperglycemic coma without ketosis is also distinguished. This condition is accompanied by an increase in blood glucose levels, while the body does not begin to break down fat tissue for energy. As a result, ketone bodies are not released, as in ketoacidotic coma.
On average, 4–31% of deaths are recorded. Death often occurs in the elderly and patients with weakened bodies.
- Emergency care and symptoms of hypoglycemic coma
Causes
The likelihood of developing a coma due to progressive ketoacidosis increases in the following cases:
- Errors in insulin therapy.
- Increased need for insulin in pregnant women, during surgical operations, the prescription of certain drugs (glucocorticosteroids, diuretics, etc.), physical activity, and stressful situations.
- Excessive intake of easily digestible carbohydrates and fats from food in case of severe dietary violations [4, 7].
Prevention
Severe complications of diabetes can only be avoided if you strictly follow medical recommendations for controlling the disease: strict adherence to a diabetic diet, rational physical activity, timely treatment of infectious diseases, avoidance of alcoholic beverages and nicotine, and regular visits to an endocrinologist. It is strictly forbidden to independently change the regimen and dosage of prescribed medications. You should not delay visiting your doctor if you experience symptoms of illness. The development of further events can be dangerous for health and life.
Hospital treatment
Sugar coma is stopped in the intensive care unit. The main goal of treatment is to restore the patient’s vitality and normalize blood sugar levels. Resuscitation measures include:
- Restoration of cardiac and respiratory activity. The patient is connected to a ventilator and given injections of cardiac medications.
- Stabilization of glycemia. For hyperglycemia, certain doses of insulin are administered; hypoglycemia involves drip administration of glucose.
- Normalization of acidity. In case of lactic acidosis and DKA, the body is alkalized with special solutions.
- Restoring electrolyte balance, removing breakdown products. Droppers with an aqueous solution of sodium chloride are used.
- Hemodialysis. The presence of renal failure is an indication for blood purification using the hardware method.
- Antishock therapy. It is carried out with hormone-containing medications (glucocorticoids).
After stabilization of the patient, a course of treatment of concomitant diseases and complications of diabetes mellitus is carried out. The rehabilitation time depends on the severity of the coma and the compensatory mechanism in the patient’s body.