Antiphospholipid syndrome (APS) is an autoimmune process of non-inflammatory origin.
During this process, immune cells produce antibodies aimed at destroying phospholipids - structural formations of vascular and nerve cells, as well as platelet membranes. Of particular danger are complications of antiphospholipid syndrome in pregnant women - stillbirth, premature birth, miscarriages, severe preeclampsia. To prevent this, even at the stage of preparation for pregnancy, the necessary diagnostics must be carried out, acquired or hereditary thrombophilia must be excluded through a blood test.
There are the following types of this pathology:
- catastrophic APS - thrombus formation in various organs in a short period of time (up to seven hours);
- primary – without manifestations of lupus erythematosus or concomitant infectious diseases;
- secondary – against the background of systemic lupus;
- syndrome without specific antibodies;
- APS, manifested by symptoms characteristic of other forms of thrombophilia.
Types of APS caused by the presence or absence of antiphospholipid antibodies:
- seropositive form - in addition to specific antibodies, a lupus anticoagulant was detected in the blood;
- seronegative form – absence of lupus anticoagulant, absence of antibodies to cardiolipin.
Diagnosis of antiphospholipid syndrome and its form is possible only in a modern laboratory equipped with highly sensitive technical equipment and high-quality reagents.
What is AFS?
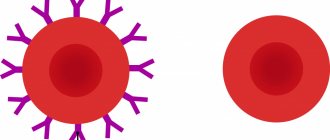
APS is an autoimmune condition when antibodies to phospholipid complexes present in a variety of human organs begin to attack the tissues of their own body, because they perceive them as foreign and, as a result, try to resist an imaginary threat.
Despite the fact that theoretically any system can be affected, most often APS causes thrombosis (both arterial and venous), resulting in the development of such dangerous pathologies as thromboembolism, stroke and heart attack. In addition, the syndrome provokes serious complications during pregnancy.
It should be immediately noted that the production of antibodies to phospholipids itself cannot cause thrombosis. A certain event is necessary that will become a factor triggering the activation of the body’s immune forces. What could it be? For example, pregnancy, injury and stress.
Pathogenesis of the development of antiphospholipid syndrome
Against the background of antiphospholipid syndrome, antibodies begin to circulate in a person’s blood, which destroy phospholipids located in the membranes of the cells of the body’s tissues. Phospholipids are present in platelets, nerve cells, and endothelial cells.
Phospholipids can be neutral or negatively charged. In the latter case, they are called anionic. It is these two types of phospholipids that are found in the blood more often than others.
Since phospholipids can be different, the antibodies produced to them are different. They are able to react with both neutral and anionic phospholipids.
Antiphospholipid syndrome is determined by immunoglobulins that appear in the blood as the disease develops.
Among them are:
- Lupus immunoglobulins lgG, lgM. These antibodies were first identified in patients with lupus erythematosus. At the same time, it was possible to detect an increased tendency to thrombosis in them.
- Antibodies to cardiolipin antigen. This component of the test allows you to detect syphilis in a person. At the same time, antibodies of classes A, G, M will circulate in his blood.
- Antibodies, which are represented by a combination of cardiolipin, phosphatadylcholine and cholesterol. They are capable of giving a positive result when performing the Wassermann reaction (diagnosis of syphilis), but this result can be false.
- Total immunoglobulins of classes A, G, M (beta-2-glycoprotein-1-cofactor-dependent antibodies to phospholipids). Since beta-2-glycoprotein-1 is an anticoagulant phospholipid, the appearance of antibodies in the blood aimed at destroying them leads to increased formation of blood clots.
The detection of antibodies to phospholipids makes it possible to diagnose antiphospholipid syndrome, the identification of which is associated with a number of difficulties.
Types of API
Antiphospholipid syndrome is divided into primary and secondary. The clinical manifestations of both forms are the same - thrombosis of various locations, miscarriage, obstetric complications (fetal growth restriction, preeclampsia, placental abruption). The only difference is the presence or absence of a background disease that could cause the appearance of APS.
- Primary antiphospholipid syndrome
Occurs in patients without concomitant autoimmune pathology, cancer, or infectious processes. In other words, there is no obvious reason for the production of antiphospholipid antibodies.
- Secondary antiphospholipid syndrome
“Lays on” the patient’s existing concomitant pathology:
- Secondary antiphospholipid syndrome against the background of autoimmune pathological conditions: rheumatoid arthritis, systemic lupus erythematosus, systemic scleroderma, ulcerative colitis, autoimmune thyroiditis, etc.
- Antiphospholipid syndrome occurring against the background of malignant pathology (carcinoma, thymoma, tumors of the lymphatic system).
- APS, which arose against the background of infectious and inflammatory processes, as well as infectious and immunological pathology (HIV, glomerulonephritis, bronchial asthma and others).
- APS that arose against the background of systemic pathologies, such as chronic renal or liver failure.
Criteria for antiphospholipid syndrome
To make a diagnosis of “Definite antiphospholipid syndrome”, at least one clinical and one laboratory criterion must be present simultaneously:
1. Clinical criteria:
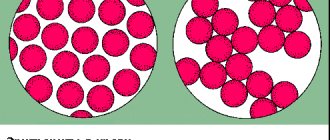
- Thrombosis of any location. This may be venous thrombosis (affecting the veins of the lower or upper extremities, thrombosis of the venous sinuses of the brain); arterial thrombosis (in the vessels of the extremities, the arteries of the heart - myocardial infarction, the arteries of the brain - ischemic stroke, the vessels of the abdominal cavity - mesenteric thrombosis, thrombosis of the renal arteries, etc.), thrombosis of the retinal vessels, as well as thrombotic lesions of the microvascular bed - for example, subcutaneous diffuse thrombosis, which manifests itself as a reticular pattern on the skin (livedo reticularis).
- 3 or more consecutive losses of a morphologically normal fetus before 10 weeks of gestation. If a chromosomal pathology is detected in a dead fetus, such a case of pregnancy loss is not taken into account as a criterion for APS.
- At least one loss of a morphologically normal fetus during pregnancy more than 10 weeks (antenatal death, late miscarriage).
- Premature birth before 34 weeks of pregnancy due to placental abruption, severe preeclampsia, placental insufficiency.
2. Laboratory criteria:
- positive blood test for lupus anticoagulant,
- antibodies to cardiolipin IgG and/or IgM, determined by ELISA, in a titer of 40 U/ml and above (with the laboratory norm not exceeding 20 U/l),
- antibodies to beta-2-glycoprotein IgG and/or IgM, determined by ELISA, in a titer of 40 U/ml (with the laboratory norm not exceeding 20 U/ml)
Important
: The laboratory criterion is considered met if positive antibodies are detected at least twice with an interval of at least 12 weeks between tests, but not more than 5 years.
In addition, the diagnosis of APS is not considered confirmed if more than 5 years have passed between clinical manifestations (thrombosis or pregnancy loss) and a positive laboratory test.
Probable antiphospholipid syndrome
If the patient has antiphospholipid antibodies, but collectively the criteria for definite APS are not met, a diagnosis of “probable APS” can be formulated. This happens, for example, with one or two fetal losses for up to 10 weeks and the presence of antiphospholipid antibodies; in case of inconsistent fetal losses (miscarriage, then childbirth, then two more miscarriages), or if, for example, the pregnancy was complicated by preeclampsia or placental abruption, but the birth occurred later than 34 weeks, and so on.
Also, the diagnosis of “probable APS” can be established when laboratory criteria are not fully met: the antibody titer does not reach the required 40 U/ml, or positive antibody tests are performed at intervals of less than 12 weeks, and so on.
Treatment
Treatment of antiphospholipid syndrome consists of prescribing anticoagulant and antiplatelet therapy. APS is treated by a rheumatologist and a hematologist; in pregnant women, by an obstetrician-gynecologist together with a hematologist.
Bibliography:
- Federal clinical guidelines for the treatment of APS, 2013
- “Antiphospholipid syndrome” Makarenko E.V. Health and environmental issues, 2021
- “Antiphospholipid syndrome in obstetric practice” Goncharova A.A., Kravchenko E.N., Krivchik G.V., Votrina I.R., Chebakova V.Yu. Mother and child in Kuzbass, 2021
- “Antiphospholipid syndrome in surgical practice” Altukhov I.A., Lyubarsky M.S., Nimaev V.V. Medicine in Kuzbass, 2014
- “Antiphospholipid syndrome in the fibrinolysis system” Ostryakova E.V., Patrushev I.L., Reshetnyak T.M. Scientific and practical rheumatology, 2011
- “The role of b-2-glycoprotein I in the pathogenesis of antiphospholipid syndrome” Kobilyanskaya V.A. Kazan Medical Journal, 2008
Symptoms of antiphospholipid symptom
The doctor may be concerned about episodes in the patient’s past, such as:
- frozen pregnancies for a period of 10 weeks or more (even one such case is a reason for examination for the presence of APS);
- premature birth before 34 weeks, if severe forms of preeclampsia or fetoplacental insufficiency were detected during pregnancy;
- miscarriages (3 or more) in the early stages (up to 10 weeks), if the reasons for this could not be found;
- hypoxia (a condition caused by insufficient oxygen supply) and delayed fetal development;
- premature detachment of a normally located placenta.
Also at risk are women who have previously developed venous or arterial thrombosis during pregnancy, while taking oral contraceptives, or after giving birth.
What body systems are affected by APS, symptoms of disorders
Antiphospholipid syndrome is associated with a risk of developing various diseases. Moreover, any organs and systems can be affected, even the brain. If its vessels are damaged, a transient ischemic attack or heart attack may develop.
This is accompanied by symptoms such as:
- The appearance of seizures.
- Dementia that is constantly progressing.
- Mental disorders.
APS can also manifest itself with the following neurological symptoms:
- Severe headaches of the migraine type.
- Uncontrollable trembling of the limbs.
- Symptoms characteristic of transverse myelitis. They occur because in APS the spinal cord is affected.
The most serious complication of heart damage is a heart attack. It develops when blood clots form in the coronary arteries. If their small branches are involved, then the heart attack will be preceded by disturbances in heart contraction. APS can also lead to the development of heart defects and the formation of an intracardiac thrombus. Such indirect signs of antiphospholipid syndrome can make it difficult to diagnose the cause of the disease.
Symptoms of APS, depending on which organ is affected by thrombosis, will be as follows:
- An increase in blood pressure is observed with thrombosis of the renal arteries.
- When a pulmonary artery is blocked by a blood clot, pulmonary embolism develops, which leads to a sharp deterioration in a person’s well-being. Sometimes the death of a patient can occur instantly.
- Bleeding in the gastrointestinal tract.
- Splenic infarction.
- The appearance of subcutaneous hemorrhages, skin necrosis, ulcers on the legs - all these symptoms develop when the dermis is damaged.
The AFS clinic is diverse. It is impossible to describe the exact symptoms, since any organs and systems can be involved in the pathological process.
APS during pregnancy
To prevent the development of dangerous complications, the doctor prescribes treatment from the very beginning of pregnancy.
If there are appropriate indications, the specialist may prescribe anticoagulants (drugs that reduce blood viscosity) and antiplatelet agents (substances that prevent red blood cells and platelets from sticking together).
Additionally, it is recommended to take B vitamins (including folic acid) and magnesium.
If a pregnant woman suffers from APS, she develops progesterone deficiency, so from the very beginning of pregnancy the doctor prescribes progesterone drugs.
Pregnancy management should be carried out under the supervision of an experienced hemostasiologist. Careful monitoring of the condition of the expectant mother and baby is necessary, as well as adjustment of the dosage of drugs based on research results. In the absence of adequate treatment, the likelihood of a successful pregnancy outcome is very low. If therapy is started in a timely manner, the chances increase markedly.
Antiphospholipid antibodies in the blood - normal or pathological?
Sometimes the level of antiphospholipid antibodies can be elevated in a healthy person. In 12% of people, these antibodies are present in the blood, but they do not develop the disease. The older the person, the higher the levels of pathological immunoglobulins may be. There is also a possibility of a false-positive Wasserman reaction, for which the patient should be prepared. The main thing is not to panic and undergo a comprehensive diagnosis.
Video: APS and other thrombophilias in obstetrics:
Author of the article:
Volkov Dmitry Sergeevich |
Ph.D. surgeon, phlebologist Education: Moscow State Medical and Dental University (1996). In 2003, he received a diploma from the educational and scientific medical center for the administration of the President of the Russian Federation. Our authors