The risk of developing hyperglycemic coma in people with diabetes is quite high. The complication occurs against the background of various provoking factors, such as refusal to diet, incorrect administration of insulin or missed injections, injuries, excessive physical exertion, etc. Help for hyperglycemic coma must be timely, otherwise there is a serious threat of severe consequences and death of the patient. The emergency care algorithm for hyperglycemic coma includes several stages, strict adherence to which ensures a favorable prognosis for the patient.
When to sound the alarm
In order to know in what cases a patient needs emergency pre-medical and medical care, you should find out what the main symptoms of hyperglycemic coma are. Signs of complications are divided into several groups. Primary manifestations indicating the risk of coma are as follows:
- weakness, malaise, fatigue;
- pathological thirst;
- development of a strong feeling of hunger;
- frequent urge to urinate;
- the appearance of skin itching;
- dry dermis;
- decreased appetite.
If the above symptoms appear, measures should be taken as soon as possible to prevent true coma.
Symptoms of true coma in diabetes mellitus:
- fog;
- lack of reaction to surrounding people and events;
- heavy, noisy, rare breathing;
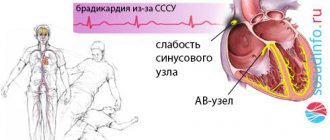
- decreased blood pressure and heart rate;
- eyeballs become soft;
- decreased skin turgor;
- pallor of the dermis;
- dark spots on the mucous membrane of the mouth.
First aid to the patient should be provided as soon as possible. The actions of relatives are aimed at maintaining breathing and heartbeat. It is important to prevent dehydration and other complications until the ambulance arrives.
Symptoms of coma
Clinical manifestations depend on the stage of coma. The initial stage is called precoma and includes a state of stupor, stupor (or stupor). All of them, unlike coma, are distinguished by the preservation of reactions and the patient can be brought out of this state by a painful or sound stimulus. Common conditions for all types of coma are:
- Stunning is a slight depression of consciousness. The patient's movements and speech are somewhat slow, and his face is unexpressive. The patient loses the ability to attentively perceive speech and experiences moderate drowsiness . The pauses between questions and answers lengthen. However, the patient is oriented to the individual, the situation, assesses the situation and follows all commands. During the period of stunning, partial amnesia may be observed (the patient cannot reproduce some events). Deep stupor is characterized by increasing drowsiness, lethargy, and slow speech. Communication with the patient is possible, but it is necessary to repeat questions many times or attract the patient’s attention by patting. The patient answers in monosyllables. With such limited contact, it is established that the patient is oriented in the person and situation, but disoriented in time. The patient's movements are sharply slowed down, and he can only carry out simple commands. The response to pain persists, and control over urination and bowel movements is weakened. With deep deafness, partial amnesia .
- Sopor. This deep depression of consciousness and communication with the patient is impossible - he is in a dream. The patient is awakened by intense external stimuli, to which he opens his eyes. The patient's face is hyperemic and there is an increase in heart rate to the voice of someone close to him. In this state, he can localize pain, and without irritation he is motionless. During the period of stupor, complete amnesia is noted. apnea may occur . There are no reflexes except the pharyngeal ones.
- Stupor develops with mental illness ( schizophrenia ), and stupor develops with somatic illnesses, infections or injuries. This condition is also characterized by pathological drowsiness, the patient opens his eyes only to sound. He is capable of simple movements, swallows food and water, and can change body position. The patient's tendon reflexes are weakened and skin reflexes are increased. Thus, stupor and stupor are characterized by inhibition and difficulty in contact. But with stupor, hallucinations and delusions , and with stunning, the patient is completely indifferent and lacks any experiences.
Coma is a state of complete absence of reflexes, characterized by very low blood pressure and body temperature, dilated pupils and rare breathing. A comatose state is characterized by the fact that the patient cannot be awakened and does not respond to stimuli. In comas that have developed against the background of diseases of the internal organs, there are characteristic symptoms that suggest its type.
Symptoms of hypoglycemic coma
Signs of hypoglycemia (sugar less than 2.5 mmol/l) develop in a short time and are associated with activation of the sympathoadrenal system , so the patient experiences increased sweating, hand tremors, palpitations, hunger, pale skin, nausea and anxiety. With a further decrease in blood sugar, the brain suffers as neuroglycopenia . It manifests itself as headache, disorientation, confusion, difficulty speaking, movement disorders (paresis, paralysis), convulsions, behavioral disorders, and amnesia. If the patient does not receive help at this stage, he falls into a coma.
Symptoms of hyperglycemic coma
Characteristic signs of hyperglycemic coma are a gradual increase in all symptoms of diabetes mellitus (thirst, dry mouth, excessive fluid intake, excessive urination) and eventually coma . A diabetic coma can take several days to develop. At an early stage, in addition to the characteristic complaints for decompensated diabetes mellitus, there is a dysfunction of the central nervous system - headache , apathy , adynamia and drowsiness or increased excitability .
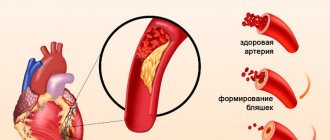
As the coma deepens, dysfunction of the nervous system progresses. Nausea, vomiting, acute abdominal pain, shortness of breath , rapid heartbeat , smell of acetone from the mouth, and decreased reflexes appear. Typical symptoms of ketoacidotic coma are frequent deep breathing (called Kussmaul breathing) and the smell of acetone. When examining the patient, a pronounced loss of fluid is noted - dry skin, mucous membranes and decreased turgor.
Hypothyroid coma
This condition is characterized by a gradual increase in all symptoms of hypothyroidism. These are drowsiness, a decrease in temperature to 34C, a slow pulse, cold extremities, swelling of the face and the whole body. The main symptom of this coma is a decrease in temperature. Coma is accompanied by increasing changes in the central nervous system: lethargy, disorientation, suppression of all reflexes. CNS depression causes an even greater decrease in heart rate and blood pressure, as well as hypoglycemia. The cause of death of a patient in this condition is pronounced changes in the cardiovascular system.
Hepatic coma
Hepatic coma is considered stage IV of hepatic encephalopathy (pathology of the central nervous system), developing in chronic liver diseases or fulminant acute hepatitis . If the patient has suffered one episode of hepatic encephalopathy, then there is a high probability of relapse in the presence of provoking factors. Coma is preceded by precoma - stage III encephalopathy, which is characterized by drowsiness, confusion, disorientation, amnesia, slurred speech, attacks of rage, irritability and disinhibition, and inappropriate behavior. Disturbances in sleep and wakefulness are typical - patients are excessively sleepy during the day and do not sleep at night.
Hepatic coma is manifested by loss of consciousness and a complete lack of response to any irritants. In acute liver failure, coma occurs with psychomotor agitation, and then lethargy and drowsiness develop. Some patients with prolonged coma develop stereotypic movements (sucking, chewing or grasping). And in the terminal stage, the pupils dilate, the reaction to light disappears, general clonic convulsions and respiratory arrest appear.
Why does coma develop?
A complication in the form of hyperglycemic coma in diabetes mellitus develops for the following reasons:
- violation of diet, consumption of large amounts of sweets;
- improper use of drugs to lower blood glucose;
- infectious diseases;
- injuries;
- untimely administration of insulin;
- failure to comply with doctor's instructions regarding the use of medications.
These and other factors cause a sharp increase in blood sugar levels, which causes hyperglycemia.
Regardless of the reasons for the development of diabetic coma, first emergency care should be competent and immediate
Classification
Comatose states can be divided into two groups: primary (or cerebral) and secondary (so-called metabolic). In this regard, the following types of comatose states are distinguished:
- Associated with damage to the central nervous system ( stroke , traumatic brain injury , brain tumors , epilepsy ).
- Occurring when gas exchange is disrupted (hypoxic, respiratory).
- Associated with impaired hormone production (hypothyroid, diabetic, thyrotoxic, hypocorticoid, hypoglycemic, hypopituitary).
- Toxigenic (associated with the action of endogenous and exogenous toxins - hepatic, pancreatic, uremic, alcoholic).
Associated with loss of electrolytes and water (hyponatremic, chlorhydropenic with vomiting, alimentary-dystrophic).
If we separately consider comas with diseases of internal organs, we can distinguish:
- Pancreatic.
- Uremic.
- Hepatic.
- Coma in diabetes mellitus .
The stages of coma are divided into:
- Mild degree. Manifested by lethargy, lethargy, confusion .
- Moderate severity. The patient is in a stupor: does not respond to light, sounds, pain. The pressure drops, the heart rate accelerates. Chaotic movements in the legs and arms are periodically observed, and spontaneous bowel movements are observed.
- Deep coma. Shallow breathing, no swallowing, pupils dilated, blood pressure reduced.
- Terminal stage. Reflexes are completely absent, the pupils do not react, the pressure is critically reduced. The patient is connected to a ventilator and receives parenteral nutrition.
Any coma is a lack of consciousness and a state of wakefulness. The patient lies with his eyes closed, he is not aware of his surroundings, and any stimulation does not cause activity. This is due to the fact that there is diffuse damage to the cortex and white matter of both hemispheres of the brain. Damage to one hemisphere does not lead to coma.
To differentiate coma from fainting, it is generally accepted that the coma lasts more than an hour. In rare cases, it lasts more than a month.
The most common are comas due to diabetes , which are its complications and require immediate treatment. The most common is diabetic coma (synonymous with ketoacidotic), which develops with insulin deficiency, decreased glucose utilization and an increase in its level in the blood (28-30 mmol/l). Develops in patients with severe diabetes mellitus. Provoking factors are:
- improper administration of insulin ;
- increased need for insulin;
- infections, injuries, operations;
- myocardial infarction;
- cerebrovascular accidents;
- stress;
- taking drugs.
Hypoglycemic coma occurs when sugar levels drop to 2 mmol/l. In diabetic patients, this type of coma is caused by a large dose of insulin and lack of food intake, severe physical activity or alcohol intake. Hypoglycemia can also be caused by sulfonylurea drugs ( Glimeperide , Amaryl , Glyme ), but this is less common than with an overdose of insulin. Some diabetic patients experience a syndrome of atypical hypoglycemia—coma develops without prior activation of the sympathoadrenal system. Hypoglycemic conditions are also observed in people who do not have diabetes.
In endocrinology, hypothyroid coma - a severe complication of hypothyroidism , which has not been treated for a long time, so decompensation of the condition has developed. It primarily develops in older people who have not received treatment. Provoking factors for this condition are operations, injuries, serious illnesses, hypothermia, and taking sedatives. Patients in a state of hypothyroid coma die from cardiac and respiratory failure in 40% of cases, even with timely resuscitation measures.
Uremic coma is associated with progressive renal failure, which causes intoxication with nitrogenous wastes and disturbances in water and electrolyte balance. This condition can develop with glomerulonephritis , diabetic nephrosclerosis , a mechanical obstruction to the outflow of urine, or exposure to nephrotic poisons. In addition to kidney diseases, this type of coma develops with shock, massive blood loss, dehydration, which results in renal failure and uremia . There is a gradual increase in symptoms. In precoma weakness , headache drowsiness , slowness of movements, nausea, itching of the skin , and the smell of ammonia in the exhaled air appear
The stuporous state gradually increases and during coma there is no consciousness, swelling , puffiness of the face , vomiting , diarrhea , and no urine appear. Blood pressure is elevated, tachycardia and arrhythmia , shallow breathing.
Another comatose state is hypoxic coma . This is a depression of the central nervous system, which is associated with a deterioration in cellular respiration due to insufficient oxygen supply to the cell. This type of coma develops faster than other types and requires urgent restoration of respiratory function. It has several options:
- Hypoxemic - insufficient supply of oxygen from the outside.
- Asthmatic - considered as a complication of bronchial asthma .
- Anemic - occurs with decompensated anemia.
- Respiratory - develops with respiratory failure.
Epileptic coma occurs after status epilepticus, when frequent seizures occur over a short period of time. The patient is unconscious, the face is pale and cyanotic, the pupils are dilated and do not react well to light. Breathing is wheezing and frequent, blood pressure is low, pulse is weak. Involuntary urination and loss of feces. As the coma deepens, breathing becomes intermittent, the pulse becomes thready, and the bluishness of the skin increases. A characteristic symptom that allows you to distinguish coma from other types is biting the tongue and the presence of bloody foam from the mouth.
First aid to the patient
The first thing to do if a hyperglycemic coma develops is to call an ambulance. If the patient is conscious, you should ask him what dose of insulin he usually injects, and help him give the injection. If there is no medicine, the patient is given sugar syrup. To do this, dissolve several tablespoons of sugar in a glass of water and give it to a person in small portions. In the absence of sugar, any product containing glucose (sweets, jam, honey, etc.) is suitable.
Actions when providing first aid:
- Place the patient on his side. This procedure will help prevent your tongue from sticking. In addition, if vomiting occurs, the patient will not choke on his own vomit.
- It is necessary to ensure the flow of fresh air into the room, to free the person from tight clothing, scarves, and collars.
- It is important to monitor blood pressure and pulse. If possible, indicators should be recorded and then passed on to medical staff.
- If the patient is shivering, cover him with a warm blanket and cover his legs with heating pads.
- The patient must be given enough water to drink.
The correct actions of people around you during an attack often help save a person’s life
If the heart and breathing stop, you cannot wait for an ambulance to arrive; you should perform artificial respiration and chest compressions.
Important! Knowledge of how to carry out resuscitation measures at home helps to avoid the death of the patient.
Prevention
If there is an endocrinological pathology, in this case diabetes mellitus, the patient needs to carefully monitor his condition and its changes. People suffering from diabetes are usually well aware of changes in their condition, regularly measure their sugar levels at home and immediately take action. Patients know that after an insulin they need to eat, they keep a diabetic diary and follow a diet. Persons who are not treated or do not know about the presence of diabetes mellitus can bring themselves into a coma. Severe stress, alcohol exposure, or severe infectious diseases can provoke a sharp deterioration in their condition, even to the point of coma.
Resuscitation actions
The following symptoms are indications for resuscitation:
- lack of pulse;
- respiratory and cardiac arrest;
- cyanosis of the skin;
- lack of pupillary reaction to light.
In this condition, you cannot wait for the doctors to arrive; resuscitation should be carried out as soon as possible.
Artificial respiration
To perform artificial respiration, you need to lay the patient on a hard surface and place a cushion under the neck. The patient's head should be tilted back and the mouth should be open. Before performing the procedure, you need to make sure that there are no foreign bodies, mucus, or blood in the oral cavity. If necessary, mucus and remnants of vomit are removed by wrapping the finger in a bandage or handkerchief.
To perform artificial respiration, a handkerchief or gauze is placed on the patient's lips. Inhalation is done through the mouth for 2–3 seconds, while the patient’s nose should be pinched. Repetition frequency 15–20 times per minute.
Indirect cardiac massage
To carry out the procedure, the person is placed on his back, the chest is freed from clothing. Hands should be clasped and placed in the center of the chest. After this, jerking movements are performed 50–60 times per minute.
When performing artificial respiration and cardiac massage at the same time, you should alternate 1 breath with 4–5 shocks. It is recommended that two people perform the procedure.
Indirect cardiac massage helps maintain its function until the ambulance arrives and prevent clinical death of the patient
Resuscitation measures in children and adults should be continued until doctors arrive or until the patient shows signs of life. If a person has come to his senses, under no circumstances should he be left alone.
Consequences and complications
Complications of hyperglycemic coma are:
- Severe acidosis .
- Hypokalemia.
- Hypocalcemia.
- Infection.
- Brain swelling . This is a rare complication that occurs more often in children and develops 4-12 hours after treatment. The reason is a rapid decrease in blood glucose or osmolality, as well as the presence of hypoxia of the central nervous system. To avoid a rapid decrease in osmolarity, first use 0.9% sodium chloride , and then 0.45% sodium chloride . And to prevent a rapid decrease in blood sugar, first perform rehydration (replenish the loss of the liquid part of the blood), and after 2 hours begin administering insulin.
- Shock.
- Pulmonary edema.
- Arterial thrombosis.
Complications of severe hypoglycemia include:
- Cardiovascular complications ( angina pectoris , myocardial infarction , stroke , atrial fibrillation, paroxysms of ventricular tachycardia , myocardial ischemia ).
- Neuropsychic ( convulsions , paresis , paralysis, decortication , behavioral disorders, intellectual disorders, psychoses ).
With uremic coma, the following may develop:
- Bloody vomiting.
- Brain edema.
- Uremic peritonitis .
- Hemorrhagic stroke.
With hepatic coma the following are possible:
- Brain swelling
- Bleeding.
- Kidney failure.
- Respiratory failure.
Medical measures
A patient with hyperglycemic coma should be hospitalized immediately. Further actions of doctors depend on the patient’s condition and the type of diabetic coma.
Help with ketoacidotic coma
After the patient is admitted to the hospital, insulin must be administered. First, a jet injection is carried out, then a dropper is placed. The stages of medical care include:
- Gastric lavage using an enema method.
- To restore fluid balance in the body, Ringer's solution is injected.
- Sodium bicarbonate is used to restore electrolyte balance.
- Blood sugar levels are constantly monitored. Reduce the amount of glucose gradually. A sharp fall can provoke a serious condition for the patient.
To maintain cardiac activity, oxygen therapy is carried out, glycosides, Cocarboxylase and other drugs are used.
Treatment of hyperosmolar coma
Emergency care for this condition has its own characteristics. Here, the actions of medical workers are aimed at preventing dehydration (dehydration). To do this, the patient is given a sufficient amount of infusion solutions. To restore fluid balance in the body, Ringer's solution and saline solution are used. At the same time, an insulin drip is administered. The hormone is administered in small doses, this helps prevent its sharp jump in the body.
Bicarbonates are not used in hyperosmolar coma, since their use is advisable for acidosis.
Treatment of hyperglycemic coma in a hospital is carried out depending on the patient’s well-being, the type of coma and the characteristics of its course.
Relief of lactic acidotic coma
When lactic acidotic coma occurs, the actions of medical workers are as follows:
- Methylene blue is used to bind and remove hydrogen ions. The drug has a redox effect, disinfectant, and analgesic effect.
- The use of Trisamine helps prevent changes in pH values of the acid-base balance.
- Hemodialysis is used to cleanse the blood.
- Drip administration of sodium bicarbonate is performed.
- Insulin is administered through a drip at 5% glucose. This helps prevent its sudden increase in the body.
After normalizing the biochemical parameters of the patient’s blood, restoring glucose and insulin levels, therapy consists of following a diet and other preventive measures.
Important! Knowledge of how to provide first aid to patients with diabetic coma is necessary not only for the patient himself, but also for his close people and relatives.
Emergency care for hyperglycemic coma is of great importance for the patient. Competent pre-medical measures and professional actions of doctors help save the patient’s life and prevent the development of severe complications in the future.
Causes
The reasons for this condition are varied and the following can be distinguished:
- Traumatic factors (brain injury, exposure to electric current).
- Thermal effects (this can be overheating and hypothermia).
- Exposure to neurotoxins ( ethylene glycol , alcohol substitutes , drugs in toxic doses, barbiturates and sedatives ).
- Hypoxia.
- Infectious factors (exposure to neurotropic viruses, toxins of botulism, malaria, typhus).
- Exposure to large doses of radiation.
- Pathological conditions ( stroke , brain tumor , cerebral edema , abscess ).
- Blood pathology ( hemolysis of red blood cells , anemia ).
- Respiratory failure.
- Liver failure.
- Kidney failure.
Hyperglycemic coma is provoked by:
- Incorrect administration of insulin (reducing the dose and number of injections, unauthorized withdrawal of insulin).
- Infections.
- Injuries and surgeries.
- Acute cardiovascular diseases.
- Psycho-emotional stress.
- Taking drugs.
- Long-term use of glucocorticoids and diuretics.
- Pregnancy.
Hypoglycemic coma is provoked by:
- Violation of the diet with skipping meals.
- Insulin overdose (faulty syringe pen, error in dose calculation, malfunction of the glucometer).
- Drinking alcohol.
- Changing insulin medications.
- Excessive loads.
- Impaired kidney and liver function.