What is diabetic coma
Diabetes mellitus is a pathology of the endocrine system, accompanied by impaired absorption of glucose due to an absolute or relative lack of production of the hormone insulin. The result of such disorders is the development of hyperglycemia (increased blood sugar levels) or hypoglycemia (decreased blood sugar in the patient).
Diabetic coma is a dangerous complication of diabetes mellitus, accompanied by the development of unpleasant symptoms, including complete loss of consciousness and death.
Depending on the mechanism of development, medical practice distinguishes between hyperglycemic and hypoglycemic coma.
Hyperglycemic
Hyperglycemic coma is a complication accompanied by a sharp decrease in the hormone insulin in the blood simultaneously with an increase in glucose levels. This type of complication can occur with any type of diabetes, but is extremely rare in type 2 diabetes. More often, hyperglycemic coma is diagnosed in insulin-dependent patients with type 1 disease.
There are several types of hyperglycemic coma:
- ketoacidotic – occurs due to improper treatment of diabetes mellitus or due to non-compliance with preventive rules for the disease. The mechanism for the development of complications is a significant increase in glucose and ketone bodies in the blood;
- hyperosmolar - this type of coma is caused by a sharp increase in blood glucose levels along with hyperosmolarity and a decrease in acetone in the blood;
- lacticidemic - accompanied by a decrease in the amount of insulin against the background of an increase in the level of lactic acid. This type of complication most often leads to death.
Hyperglycemic coma is caused by increased blood sugar levels
Symptoms for one type of complication or another are similar. These include the development of pathological thirst, the appearance of weakness, dizziness, and increased urination. The patient experiences mood swings, drowsiness is replaced by excitement. Some patients experience nausea, stool upset, and vomiting. In severe cases, there is confusion, a lack of reaction to surrounding people and events, a decrease in blood pressure and pulse rate.
Important! If such symptoms are detected, it is necessary to provide the person with first aid, call a doctor or take the patient to the hospital.
Hypoglycemic coma
Hypoglycemic coma is usually called a pathological condition of a patient that develops as a result of a decrease in blood glucose levels or a sharp drop in its amount. Without glucose, normal functioning of brain cells is impossible. Therefore, when it falls, a malfunction occurs in the body, provoking severe weakness of the person, then a hypoglycemic coma. Loss of consciousness occurs when glucose levels drop below 3 mmol/liter.
Symptoms of hypoglycemic coma include unnatural paleness of the skin, moist cold skin, dizziness, drowsiness, increased heart rate, the patient's breathing becomes weak, blood pressure drops, and the pupils stop responding to light.
Ketoacidotic
Hyperglycemic hyperketonemic coma is an acute decompensation of diabetes, which develops as a result of severe insulin deficiency. At the same time, there is a lot of glucose in the blood, but in the absence of insulin it does not enter the cells, so fat begins to be used as an energy source instead of carbohydrates.
Active breakdown and inclusion of free fatty acids in metabolism leads to the formation of ketone bodies. Their synthesis increases to 1000 mmol per day, which significantly exceeds the ability of the kidneys to excrete ketones in the urine [7].
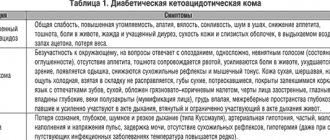
Changes in blood and urine tests in diabetic ketoacidosis in adults are presented in table [1].
| Laboratory indicators | Values |
| Blood plasma glucose | >13 mmol/l to 18-20 mmol/l [3] |
| Plasma ketone bodies | >5 mmol/l |
| Ketonuria | ≥++ |
| pH | ˂7,3 |
Stages of pre-hospital emergency care
Patients suffering from diabetes, their loved ones and relatives must know how to provide first aid to a patient who develops a coma. For different types of coma, the actions are somewhat different.
If a serious condition develops in a person with diabetes, the first thing to do is call an ambulance
First aid for hyperglycemic coma
If signs of increased blood glucose appear, you should immediately seek medical help or call a team of doctors to your home. This condition is considered especially dangerous for children, pregnant women and the elderly. To prevent serious consequences, the actions of relatives should be as follows:
- If there is no breathing, the pulse cannot be felt, it is necessary to perform an indirect cardiac massage. In many cases, this helps save the patient's life.
- If a person is unconscious, but breathing continues, it is necessary to turn him over to the left side, making sure that in case of vomiting he does not choke.
- Fresh air must be allowed into the room; crowds should not be allowed near the patient.
After the ambulance arrives, doctors need to be informed about the time of the attack, the characteristics of the patient’s behavior, and its symptoms.
Actions for hypoglycemic coma
During a coma due to diabetes, emergency care should be immediate. A person needs to be given sugar or tea with it added. In addition to sugar, you can use honey, jam and other products containing glucose.
If the condition worsens, the help algorithm is as follows:
- Call an ambulance.
- Place the patient on his left side. A common symptom of coma development is vomiting. It is important to ensure that if it occurs, the person does not choke.
- If there is information about what dose of glucagon the patient usually administers, this should be done urgently. Often patients suffering from diabetes mellitus carry an ampoule with this medicine.
- Before the ambulance arrives, it is necessary to monitor the person’s breathing. If it is absent and the heartbeat stops, artificial respiration and chest compressions must be performed.
If a patient with a diabetic coma stops breathing, artificial respiration can save his life
Important! If the person is conscious, you have given a glucagon injection, and the patient’s condition improves, you still need to call an ambulance. Doctors must take control of the patient.
Help with hyperosmolar coma
Hyperosmolar coma develops with excessive consumption of carbohydrates, as a result of injuries, against the background of diseases of the gastrointestinal tract in diabetes mellitus. In this case, the patient experiences thirst, weakness, and fatigue. In severe cases, confusion, speech inhibition, and the development of seizures are observed.
First aid for such patients is as follows:
- Call an ambulance.
- Turn the patient onto his left side.
- Prevent tongue retraction.
- Measure the pressure. If it is high, give the patient an antihypertensive drug.
Such actions will help support the patient’s vital processes until the ambulance arrives.
What to do with ketoacidotic coma
The main actions for this type of complication should be aimed at maintaining the person’s vital functions (breathing, heartbeat) until doctors arrive. After calling an ambulance, it is necessary to determine whether the person is conscious. If the patient’s reaction to external stimuli is absent, his life is threatened. If there is no breathing, artificial respiration should be performed. The one who performs it must monitor the condition of the respiratory tract. Mucus, vomit, and blood should not be present in the oral cavity. If cardiac arrest occurs, perform indirect massage.
If the type of coma is not determined
The first rule for providing emergency care when signs of a diabetic coma appear is to call an ambulance. Often the patients themselves and their relatives are informed about what to do in such situations. If a person is conscious, he should inform his family about options for help.
If necessary, in a diabetic coma, you need to help the patient administer insulin.
In case of loss of consciousness, it is necessary to ensure the patient's airway is free. For this, the person is placed on his side and, if necessary, mucus and vomit are removed. This will help avoid tongue retraction and respiratory arrest.
You should contact a medical facility when the first alarming symptoms appear, without waiting for the situation to become more complicated. This will help prevent the development of serious health consequences and prevent the death of the patient.
Causes
Most often, hyperosmolar non-acidotic coma develops in elderly people living with type 2 diabetes [3]. Provoking factors include any diseases and conditions in which the body actively loses fluid:
- irrational use of diuretics;
- diseases accompanied by recurring diarrhea and vomiting;
- staying in conditions that cause active sweating (working in a hot shop, moving to a country with a hot climate, etc.).
Also, this type of diabetic coma can develop with myocardial infarction, massive bleeding, and in patients on hemo- or peritoneal dialysis [7].
Medical care for the patient
When a patient is admitted to a hospital, the algorithm of actions of medical workers is as follows:
- Gradually lowering the amount of sugar in the blood by administering small doses of insulin.
- Drip administration of sodium chloride, Acesol, Ringer and other drugs. This helps prevent dehydration, a decrease in the amount of blood in the body.
- Monitoring potassium levels in the blood. When it drops below 4 mmol/l, potassium is administered intravenously. At the same time, the insulin dose is increased.
- To normalize metabolic processes, vitamin therapy is carried out.
If the patient's serious condition is caused by a bacterial infection, antibacterial therapy is carried out. In addition, antibiotics are prescribed for prophylactic purposes to prevent infection, since during illness a person’s immunity is weakened.
To eliminate symptoms, the following groups of medications are used:
- vasodilators;
- nootropic drugs;
- hepatotropic drugs;
- antihypertensive drugs.
Caring for a patient necessarily includes monitoring the physiological functions of the body. To do this, blood pressure, pulse, central venous pressure, body temperature are periodically measured, the patient’s breathing, the activity of the gastrointestinal tract, and the amount of urine excreted are monitored. Thanks to this, it is possible to find out the cause of decompensation of diabetes mellitus and select the necessary treatment.
Clinical manifestations of hypoglycemia
Precursors are weakness, anxiety, trembling of arms and legs, sweating, and the appearance of hunger. Advanced stage: psychomotor agitation, then stupor, stupor or coma develops. The face is mask-like, severe sweating, tissue turgor is normal, muscle tone is high; tachycardia, blood pressure is initially increased, then it decreases. Clonic-tonic convulsions often occur. Sometimes hypoglycemic coma develops suddenly and is characterized by a triad of symptoms: loss of consciousness, muscle hypertonicity, and convulsions. With prolonged hypoglycemia, a clinical picture of cerebral edema develops. In a patient with diabetes mellitus, hypoglycemic coma is differentiated from hyperglycemic ketoacidotic coma.
Emergency measures for manifestations of hypoglycemia:
- if consciousness is preserved, take carbohydrate-containing products (sweet tea, apple or orange juice); in the absence of positive dynamics after 10-15 minutes. – repeated intake of easily digestible carbohydrates;
- calling an ambulance;
- in case of impaired consciousness - slowly inject 40% glucose solution intravenously - 1-2 ml / kg until the patient comes out of coma and the convulsions stop;
- when regaining consciousness, administer easily digestible carbohydrates orally;
- if there is no effect after 10-15 minutes. – repeated intravenous administration of 40% glucose solution up to 5 ml/kg;
- in the absence of positive dynamics, administer intravenous hydrocortisone 0.5-10 mg/kg body weight (prednisolone, dexamethasone are not administered due to the high risk of developing cerebral edema);
If the child’s consciousness has not recovered, enter:
- intravenous, intramuscular glucagon in a dose of 0.5 ml for children weighing up to 20 kg and 1.0 ml;
- with a weight of more than 20 kg or 0.18% solution of epinephrine (adrenaline) 0.1 ml/kg s.c.
If the patient does not regain consciousness, suspect cerebral edema! For cerebral edema, administer:
- 1% solution of furosemide (Lasix) 0.1-0.2 ml/kg intravenously or intramuscularly;
- 10% mannitol solution 0.5–1.0 g/kg intravenous drip in 10% glucose solution,
- dexamethasone solution 0.5-1 mg/kg (1 ml - 4 mg) intravenously,
- oxygen therapy.
Attention! If acute intracranial hypertension is suspected, limit intravenous infusion, but do not stop - catheter thrombosis is possible
Hospitalization in the intensive care unit (in the absence of consciousness), if the patient is conscious - in the endocrinology department of the hospital.
Pathogenesis and symptoms of hypoglycemia
As the sugar level drops to 2.77-1.66 mmol/l, very characteristic symptoms begin to appear. The person notices an increased feeling of hunger. Trembling appears in the hands, the skin becomes pale.
There is a decrease in mental and physical activity. Disorders of the nervous system are possible, in particular inappropriate behavior, feelings of anxiety and fear, excessive aggression, and mood swings. Glucose deficiency is accompanied by tachycardia and increased blood pressure.
If the sugar level drops to 1.38 mmol/l, the patient usually loses consciousness. In such cases, you need to take the person to the hospital department as soon as possible.
Hyperlactic acidemic coma: features and consequences
This form of coma is observed during hypoxia (oxygen starvation), which develops against the background of insulin deficiency. In such cases, the pathology is accompanied by an accumulation of lactic acid, which leads to a change in the chemical composition of the blood. The result is a narrowing of peripheral vessels, impaired contractility and excitability of the myocardium.
In most cases, this type of diabetic coma is associated with cardiac and respiratory failure, inflammatory processes, and infections. Risk factors include chronic liver and kidney diseases, alcoholism.
Diagnostic measures
Diabetic coma is characterized by symptoms that will not go unnoticed by the doctor. After examining the patient, the specialist can determine his condition and provide the necessary assistance. However, correct diagnosis is important. First of all, laboratory and biochemical analysis of blood and urine is carried out.
In case of hypoglycemia, a decrease in sugar level can be noted, in all other cases - its increase to 33 mmol/l or more. The presence of ketone bodies, an increase in plasma osmolarity, and an increase in the level of lactic acid in the blood are taken into account. In a comatose state, the functioning of the nervous system and other organs is assessed. If complications occur, symptomatic therapy is necessary.
Prevention of coma in diabetes
Complications of diabetes, coma in particular, can be very dangerous. That is why it is better to monitor your own condition and follow some precautionary rules:
- you need to follow the diet prescribed by your doctor and follow a diet;
- the patient is obliged to regularly go to the doctor for examinations and undergo tests;
- Self-control and compliance with safety rules are important (the patient must have a glucometer with him and regularly measure blood sugar levels);
- An active lifestyle, frequent walks in the fresh air, and feasible physical activity are recommended;
- it is very important to follow precise recommendations and observe the dosages of insulin and other medications;
- Under no circumstances should you self-medicate or use any traditional medicine without first consulting your treating endocrinologist.
Compliance with such simple rules in most cases helps prevent the development of complications, including the onset of coma. If any alarming changes occur, you should immediately consult a doctor.
Coma with diabetes: first aid
Patients with diabetes are usually warned about the possibility of developing coma and told about the algorithm of actions. What should you do if a patient shows signs of a condition such as a sugar coma? The consequences are extremely dangerous, so a sick person needs to measure their glucose level using a glucometer. If the sugar level is elevated, you need to inject insulin; if it is low, eat candy or drink sweet tea.
If the patient has already lost consciousness, it is important to place him on his side so as to prevent the tongue from retracting and vomit from entering the respiratory tract. If the patient has removable dentures, they also need to be removed. It is recommended to wrap the victim so as to warm the lower extremities. Next, you need to call an ambulance - the patient needs quick and qualified help.
Sugar coma: consequences
Unfortunately, this phenomenon is considered quite common. How dangerous is a sugar coma? The consequences may vary. This condition is accompanied by serious metabolic disruptions. There is depression of the central nervous system. Coma can last for several days, months or even years. The longer the patient remains in this condition, the higher the likelihood of developing a complication such as cerebral edema.
With adequate treatment, the outcome is usually quite favorable. On the other hand, cerebral edema can lead to significant damage to the central nervous system and, accordingly, functional impairment. For example, some patients suffer from memory and speech disorders and problems with coordination. The list of consequences includes serious pathologies of the cardiovascular system. Coma due to diabetes mellitus in children sometimes leads to further delays in mental and physical development.
Unfortunately, patients are not always able to recover from the consequences of a coma. This is why it is important to take precautions.