For normal functioning of the human body, a regular supply of vitamins, nutrients and minerals is necessary. A deficiency of any element causes a malfunction of the entire body and leads to various health problems.
Calcium is an essential element of metabolism and its deficiency is acutely felt by all organs and systems of the body. The most common diseases caused by calcium deficiency are hypocalcemia, hypocalcinosis, and osteoporosis.
Why is calcium needed in the body?
As almost everyone knows, calcium is the main element of bones and teeth, but its role in the body is not limited to this. Calcium regulates the contractile function of the heart, nourishes nervous tissue, ensures the conduction of nerve impulses, reduces the level of bad cholesterol, regulates blood pressure, maintains normal blood pH levels, is involved in the transport of nutrients and the removal of metabolic products, etc. The need for this element increases significantly during pregnancy, and a lack of calcium makes normal development of the fetus impossible and worsens the condition of the expectant mother.
What is the purpose of each mineral in Calcemin® Advance?
— Copper is involved in the formation of cross-links in collagen. — Manganese and zinc contribute to the formation of the collagen matrix. — Magnesium is necessary to restore bone structure. — Boron helps bone cell growth and collagen production.
Thus, Calcemin® Advance helps stop calcium leaching and prevent vitamin D3 deficiency so that bones remain strong, and if taken in a timely manner, avoid the manifestation of unwanted symptoms in both adults and children.
What can cause calcium deficiency in the body?
A lack of calcium in the body occurs in two cases. When there is insufficient intake of a mineral from food or when the body’s ability to absorb this trace element decreases. Calcium deficiency can be caused by:
- dysfunction of the thyroid and parathyroid glands;
- impaired absorption of calcium in the intestine caused by intestinal diseases (dysbacteriosis, allergies, colitis, etc.)
- metabolic disorder, which is characterized by low levels of vitamin D and high levels of lead, zinc, phosphorus, magnesium, iron, cobalt, potassium and sodium, which contribute to the excretion of calcium;
- uncontrolled use of diuretics and diuretics;
- hormonal disorders (lack of estrogen);
- elderly age.
Abuse of coffee-containing drinks, alcohol and smoking are pathogenic factors in the occurrence of calcium deficiency in the body.
What are the consequences of calcium deficiency?
As calcium is washed out of bone tissue into the blood, the tendency to fractures, dislocations, and subluxations increases. Young people periodically experience joint pain characteristic of osteoporosis, while older people experience fractures of the vertebral bodies or the neck of the femur.
Photo: istockphoto.com
If calcium deficiency has already been diagnosed, it is better to take a course of supplements. The best absorbable form is calcium citrate. It is taken in a dosage of 800-1200 mg per day (pregnant women and elderly people 1500 mg) on an empty stomach. Calcium is better absorbed when reacting with acid, for example, taken simultaneously with vitamin C or lemon juice). Vitamin D, adequate animal protein intake and a healthy gastrointestinal tract are also essential.
Consult your physician before taking supplements.
Symptoms of calcium deficiency in the body
Calcium deficiency does not have specific, pronounced symptoms. As a rule, a general deterioration in health is diagnosed, expressed in the following disorders:
- increased nervous excitability, sleep disturbances, irritability, fatigue, decreased performance;
- muscle cramps, tingling, numbness of fingers and toes, with periodic pain;
- dry and flaky skin, brittle nails, increased sweating, especially in the head area;
- tooth decay, increased bleeding gums;
- frequent fractures and cracks of bones, development of osteoporosis;
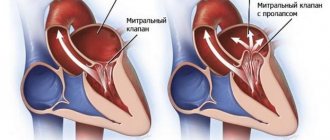
- disruption of heart function up to the development of heart failure, cardiac arrhythmia;
- blood clotting disorder;
- decreased immunity, which is expressed in a long course of the disease and frequent morbidity;
- increased sensitivity to cold, chilliness, body aches, severe chills.
Blood Ca levels
The daily intake of macronutrients depends on age and gender.
Adults:
- men and women under 65 years of age – 800–1000 mg;
- from 65 years – 1200 mg;
- lactating and pregnant women – 1500–2000 mg.
Children:
- up to 6 months – 400 mg;
- up to 3 years – 600 mg;
- from 3 to 10 years – 800 mg;
- from 10 to 14 years – 1000 mg;
- up to 18 years – 1200 mg.
Increased amounts of calcium are required by athletes and people engaged in heavy physical labor. Also, its consumption should be increased in the presence of injuries and bone fractures. The exact daily dose is determined by the attending physician.
Treatment of Ca deficiency
The disease can occur in acute and chronic form. An acute condition requires treatment in a hospital setting, as it threatens the patient’s life. In case of chronic calcium deficiency in the body, synthetic calcium-containing preparations, vitamin and mineral complexes are prescribed, the diet is adjusted to increase the intake of microelements in food, and concomitant pathologies are treated. To speed up metabolic processes, sufficient physical activity is recommended.
Calcium deficiency cannot be treated on your own. Self-medication is especially dangerous during pregnancy or childhood. An overdose of calcium in the body, which occurs from uncontrolled intake of calcium supplements, can pose a serious health hazard. You should take any medications only after examination and consultation with a specialist.
At a medical clinic, you can undergo a comprehensive examination to determine the level of calcium in the body and, based on its results, receive qualified consultation from a doctor. It is important to remember that uncontrolled use of calcium supplements is dangerous to health. Without determining the degree of calcium deficiency, the causes of pathology, identifying and treating diseases that could provoke a lack of the mineral, you cannot take calcium supplements. Treatment of complications of the disease may also be necessary, and this should also be done by a specialist. You can make an appointment by phone: +, +.
When there is not enough calcium in a person's bones...
As you know, there are many bones in the structure of the skeleton, each of which performs its own function. Moreover, bone is a living element of the system that requires nutrition and renewal. Moreover, the bones themselves cannot function normally if they do not receive the appropriate load.
Why is there not enough calcium in the skeletal system: what are the reasons?
Every part of the bone skeleton contains calcium, which makes bones strong and hard. If the body does not receive this chemical element in full, pathological changes may begin in the bones, and serious changes do not require much time. If a person breaks his leg and walks in a cast for even thirty days, we can already talk about the beginning of disorders in the bone tissue.
But not only bone injury leads to calcium deficiency. Scientists have already proven that human aging is accompanied by a sharp leaching of calcium from the body. This is why bones in older people become less strong and brittle. A disease such as osteoporosis appears. He can accompany any elderly person. This disease begins much earlier. This calcium deficiency is considered normal and cannot be avoided. If you have osteoporosis, treatment should only be carried out under the supervision of specialists.
Decalcification of the skeletal system can be caused by various diseases:
- Diseases of the gastrointestinal tract, when the body is not able to obtain enough calcium from the foods it eats.
- In case of kidney disease, when a huge amount of calcium is washed out along with the urine.
- In women expecting the birth of a baby, the fetus requires calcium in large quantities for the proper formation of the skeleton. But, in fact, it is produced in such a large amount that it leads to damage to bone tissue and makes the bones completely fragile.
- If a person takes a large number of medications that are hormonal drugs. In this case, the balance of calcium in the skeletal system is also disturbed, since these medications capture free calcium and remove it from the body.
How can you determine that there is a calcium deficiency in the body?
If bone tissue lacks an element such as calcium, the bones begin to lose hardness, become less strong and brittle. It is for this reason that older people get broken bones when they fall.
Sometimes there is not even a fall, but the bones break: this is due to bone deformations, most often the vertebral bodies are deformed. If the cartilage and bone endplate breaks, part of the nucleus pulposus is displaced. It is embedded in the spongy substance. Due to such an injury, an intervertebral hernia appears.
Elderly people often experience fractures:
- In the area of the femoral neck.
- The vertebral bodies themselves.
- Spongy bones can have microfractures, after which microcalluses subsequently form.
What you need to know about the treatment of diseases associated with calcium deficiency?
Decalcification is a serious process, sometimes leading to irreparable consequences. The fight against such a disease is never easy.
If a person does not have problems with the intestines or kidneys, and the metabolism is not impaired, then maintaining the functioning and structure of the skeletal system is not so difficult. It is enough to adhere to a healthy lifestyle. Dealing with decalcification is often very difficult. This is an effective method that has a beneficial effect on the cells responsible for the structure of bone tissue.
But in our fast-moving times, it is not always possible to find the opportunity to visit the gym. You can purchase a Swing Machine, with which you can not only load your spine physically, but also receive the necessary dose of massage.
In order for the metabolism in the body not to be disturbed, it is necessary to treat nutrition correctly; products should be healthy and properly balanced. Food should contain enough calcium-rich foods. We should not forget that in addition to this element, other minerals and vitamins must be supplied to the body in the required quantities.
A lot of calcium is found in a number of foods that you need to have in your diet:
- Milk and dairy products, including cheese. You need to eat it every day.
- Fish.
- Don't shun cow butter and eggs.
- Spinach, legumes, cabbage.
Complete absorption of calcium is possible only with the presence of vitamin D, so milk, margarine, and liver should be present in your diet.
Author: K.M.N., Academician of the Russian Academy of Medical Sciences M.A. Bobyr
Long-acting calcium antagonists in the treatment of arterial hypertension
Introduction
Calcium antagonists are a large group of drugs, the main property of which is the ability to reversibly inhibit the flow of calcium through the so-called slow calcium channels. These drugs have been used in cardiology since the late 70s and have now become so popular that in most developed countries they occupy one of the first places in terms of frequency of prescription among drugs used to treat cardiovascular diseases.
.
This is due, on the one hand, to the high clinical effectiveness of calcium antagonists, on the other hand, to the relatively small number of contraindications to their use and the relatively small number of side effects they cause. Calcium antagonists are a large group of drugs, the main property of which is the ability to reversibly inhibit the flow of calcium through the so-called slow calcium channels.
These drugs have been used in cardiology since the late 70s and have now become so popular that in most developed countries. This is due, on the one hand, to the high clinical effectiveness of calcium antagonists, on the other hand, to the relatively small number of contraindications to their use and the relatively small number of side effects they cause. Recently, long-acting dosage forms of calcium antagonists have been increasingly used. Such dosage forms have been created for almost all groups of calcium antagonists currently in use.
Classification of calcium antagonists
There are different classifications of calcium antagonists. According to chemical structure
distinguish: dihydropyridine calcium antagonists (nifedipine, nicardipine, felodipine, lacidipine, amlodipine, etc.), benzodiazepine derivatives (diltiazem) and phenylalkylamines (verapamil).
Calcium antagonists are also distinguished by their duration of action
. Short-acting calcium antagonists (first-generation calcium antagonists) include conventional tablets of nifedipine, verapamil, diltiazem; to maintain a constant effect, they must be prescribed 3 or even 4 times a day. Long-acting calcium antagonists (second-generation calcium antagonists) include either special dosage forms of nifedipine, verapamil, diltiazem, which ensure uniform release of the drug over a long time (generation IIa drugs), or drugs of a different chemical structure that have the ability to circulate in the body for a longer period of time ( IIb generation drugs: felodipine, amlodipine, lacidipine).
Second-generation calcium antagonists are prescribed 1 or 2 times a day. Amlodipine has the longest lasting effect of all calcium antagonists.
, its half-life reaches 35–45 hours.
Basic pharmacological properties
Despite the common mechanism of action of calcium antagonists at the cellular level, the pharmacological properties of various drugs in this group are quite different. The most significant differences are observed between dihydropyridine calcium antagonists (nifedipine), on the one hand, and phenylalkylamine derivatives (verapamil) and benzodiazepine derivatives (diltiazem), on the other hand.
Dihydropyridine calcium antagonists primarily act on the smooth muscle of peripheral arteries, i.e. are typical peripheral vasodilators. Due to this, they reduce blood pressure (BP) and can reflexively increase the heart rate (HR), for which they are also called pulse-increasing calcium antagonists. Dihydropyridine calcium antagonists in therapeutic doses do not affect the sinus node or the conduction system of the heart, so they do not have antiarrhythmic properties. They also do not affect myocardial contractility.
The selectivity of action on peripheral vessels varies among different dihydropyridine calcium antagonists. Nifedipine is the least selective in this regard; amlodipine and lacidipine have the greatest selectivity. Due to the gradual onset of action and long half-life, amlodipine does not cause reflex tachycardia
or its manifestations are insignificant [1, 2].
Verapamil and diltiazem have significantly less pronounced peripheral vasodilating effects than dihydropyridine calcium antagonists. Their action is dominated by a negative effect on the automatism of the sinus node (due to this they are able to reduce heart rate and are called pulse-reducing calcium antagonists), the ability to slow down atrioventricular conduction, and have a negative inotropic effect due to the effect on myocardial contractility. These properties make verapamil and diltiazem similar to b-blockers.
Indications and contraindications for the use of calcium antagonists
All calcium antagonists are successfully used to treat arterial hypertension, stable angina pectoris, and vasospastic angina. Calcium antagonists that reduce the pulse - verapamil and diltiazem - are quite widely used as antiarrhythmic drugs (for the treatment of supraventricular rhythm disturbances). These drugs, however, are contraindicated in patients suffering from sick sinus syndrome and patients with impaired atrioventricular conduction. For these last two conditions (very common in elderly patients), only dihydropyridine calcium antagonists can be used. If we remember that the use of dihydropyridine calcium antagonists is also possible in a number of situations where the use of b-blockers is contraindicated or undesirable (peripheral circulatory disorders, obstructive pulmonary diseases, bronchial asthma), it becomes clear why dihydropyridine calcium antagonists are often the drugs of choice.
The use of calcium antagonists that reduce pulse rate is undesirable in patients with impaired left ventricular function, as it can cause even greater deterioration. The use of dihydropyridine calcium antagonists in such patients is safer, however, in such cases, preference should be given to more selective dihydropyridine calcium antagonists, primarily amlodipine. In a special study PRAISE
(Prospective Randomized Amlodipine Survival Evaluation) it was demonstrated that the administration of amlodipine to patients with chronic heart failure and significantly reduced left ventricular ejection fraction was not only completely safe, but also
significantly improved the prognosis of life
in such patients [3].
Calcium antagonists in the treatment of arterial hypertension
All calcium antagonists have the ability to reduce blood pressure in patients with arterial hypertension and are successfully used as antihypertensive drugs. It is noteworthy that the ability to lower blood pressure of these drugs is more pronounced when they are prescribed to patients with arterial hypertension and less pronounced when they are prescribed to people with normal blood pressure. The high effectiveness and good tolerability of calcium antagonists for arterial hypertension has made them very popular among doctors and patients. In most countries, calcium antagonists continue to occupy one of the leading places in the frequency of prescription among drugs used to treat arterial hypertension.
.
Most researchers believe that different calcium antagonists have approximately the same hypotensive effect. It still seems that the antihypertensive effect of dihydropyridine calcium antagonists is somewhat more pronounced than that of pulse-reducing calcium antagonists [4]. According to various researchers, the number of patients in whom a significant hypotensive effect is achieved (a decrease in diastolic blood pressure to 90 mm Hg or by 10 mm Hg or more) when prescribed calcium antagonists ranges from 55 to 80%, which is not differs from results obtained with other antihypertensive drugs.
For long-acting antihypertensive drugs, it is very important that the effect completely covers the 24-hour interval and persists until the next dose of the drug. Since antihypertensive drugs are usually taken in the morning, the therapeutic effect should overlap the morning hours, since this period of the day is the most vulnerable to the development of serious cardiovascular complications. Modern long-acting calcium antagonists (amlodipine, lacidipine), when prescribed for the treatment of hypertension, clearly provide the required final effect/peak effect ratio >=0.5
. Calculation of this indicator allows, to a certain extent, to give a comprehensive assessment of both the magnitude and duration of the hypotensive effect of the drug. According to several studies, for diastolic blood pressure, the final effect/peak effect ratio is 0.5–1.0 for amlodipine prescribed at a dose of 5–10 mg [5].
Left ventricular hypertrophy, which is a compensatory response to increased blood pressure over a long period of time, is now recognized as one of the serious risk factors for the development of cardiovascular complications [6]. Available data suggest that treatment with calcium antagonists can lead to a decrease in the severity of myocardial hypertrophy and thereby reduce the risk of developing serious cardiovascular complications [7]. Ismail F. Islim et al. in their study showed that amlodipine after 20 weeks of therapy at an effective dose of 5–10 mg leads to a significant decrease in the mass of the left ventricular myocardium
, a significant decrease in the thickness of the interventricular septum and the posterior wall of the left ventricle, a significant and statistically significant decrease in peripheral resistance. However, there were no significant changes in the size of the left ventricular cavities, ejection fraction, stroke volume and cardiac output [8].
As is known, there is still no consensus on which drugs should be used to start therapy for arterial hypertension. First-line drugs are often called diuretics and beta-blockers. It should be noted, however, that calcium antagonists have significantly fewer contraindications for use than many other antihypertensive drugs, and do not cause a number of side effects characteristic of other antihypertensive drugs.
Thus, calcium antagonists, unlike diuretics, do not cause unfavorable metabolic changes (do not affect the level of electrolytes, lipids, uric acid, or glucose in the blood). The advantages of calcium antagonists over beta-blockers in patients with obstructive pulmonary diseases and peripheral arterial diseases were mentioned above. Calcium antagonists never cause such a common complication when prescribing angiotensin-converting enzyme (ACE) inhibitors as cough.
Since long-acting calcium antagonists are part of the main drugs for the treatment of coronary artery disease, their administration is especially indicated for patients with arterial hypertension and concomitant coronary heart disease, especially in cases where the administration of beta-blockers is contraindicated for any reason.
Benefits of long-acting calcium antagonists
Long-acting drugs were created to simplify the dosage regimen to once a day and thereby improve patient adherence to treatment. Medication adherence is known to be particularly poor in patients with hypertension because the disease is usually asymptomatic. If we consider that the treatment of arterial hypertension is carried out over a long period of time, over many years, and that the success of this therapy, in particular, its effect on the prognosis of the disease, significantly depends on the regularity of treatment, it becomes clear that this property may be decisive.
The advantage of long-acting calcium antagonists is that they are much less likely to cause side effects than short-acting calcium antagonists.
(this pattern is primarily characteristic of dihydropyridine calcium antagonists). This is due to the fact that short-acting calcium antagonists quickly create a high concentration of the drug in the blood, which causes significant, sometimes excessive vasodilation and significantly increases the tone of the sympathetic nervous system. That is why side effects of dihydropyridine calcium antagonists associated with peripheral vasodilation (tachycardia, redness of the skin, dizziness, feeling of heat) are much more common when using short-acting drugs.
In addition, long-acting calcium antagonists are drugs that can provide an adequate therapeutic effect in patients who do not always take therapy regularly, when the interval between doses of the drug can be 48 hours. It has been shown that a single omission of amlodipine leads to only a slight decrease in the antihypertensive effect of therapy [9]. In a comparative study that examined the possibility of withdrawal syndrome while taking amlodipine and perindopril, conducted by Zannad F. et al., it was shown that 48 hours after taking the last dose of amlodipine, there was only a slight increase in blood pressure and systolic and diastolic blood pressure levels were lower in patients receiving amlodipine than in patients receiving perindopril [10]. The absence of a sharp rise in blood pressure due to an unintentional omission of the drug indicates a low likelihood of developing withdrawal syndrome while taking amlodipine and increases the safety of therapy with this drug.
Possibility and feasibility of combination therapy with calcium antagonists and other drugs
Combination therapy for arterial hypertension can be used both to achieve a more pronounced reduction in blood pressure and to reduce the dose of the drug and reduce the likelihood of side effects.
The possibility and feasibility of combination therapy in relation to calcium antagonists should be considered differentiated for different subgroups of these drugs. Thus, verapamil and diltiazem combine well with most other groups of antihypertensive drugs, with the exception of beta-blockers. In the latter case, the likelihood of side effects of each drug increases significantly. Dihydropyridine calcium antagonists, on the contrary, combine well with beta-blockers. This combination not only significantly enhances the severity of the hypotensive effect, but also significantly reduces the likelihood of side effects. In particular, tachycardia, which can still appear when prescribing long-acting dihydropyridine calcium antagonists [11], is completely eliminated when a beta-blocker is added to therapy.
Dihydropyridine calcium antagonists, in addition, combine well with ACE inhibitors and diuretics. Such combinations have been successfully used in a number of large international studies [12, 13].
Do calcium antagonists affect the prognosis of patients' lives?
Since the mid-90s, there has been ongoing debate about whether long-term use of calcium antagonists is safe. The reason for them was data obtained back in the 80s, demonstrating the ability of short-acting dihydropyridine calcium antagonists, prescribed without beta-blockers, to negatively affect the outcome of the disease in patients with unstable angina and acute myocardial infarction [4,11]. There are no special studies proving the possibility of a negative effect of long-acting calcium antagonists either in patients with coronary heart disease or in patients with arterial hypertension. In the Lancet journal in 2000, data from a special analysis were published [12], which proved that long-term use of long-acting calcium antagonists in patients with arterial hypertension is not only safe, but also leads to a significant reduction in the likelihood of developing a cerebral stroke and the likelihood of developing coronary heart disease
and its complications. According to this analysis, the effectiveness and safety of calcium antagonists was in no way inferior to those of ACE inhibitors.
The safety of long-term treatment of arterial hypertension with long-acting calcium antagonists from the dihydropyridine group is confirmed by the results of the recently completed HOT and INSIGHT studies. In the HOT
(Hypertension Optimal Treatment) it was demonstrated that a significant decrease in diastolic blood pressure (on average to 82.6 mm Hg) under the influence of drug therapy with felodipine, both as monotherapy and in combination with other antihypertensive drugs, leads to a significant reduction in the likelihood of heart disease –vascular complications and increased life expectancy of patients [13].
In the INSIGHT
(International Nifedipine GITS Study Intervention as a Goal in Hepertension Treatment) it was demonstrated that long-term administration of a special dosage form of nifedipine - nifedipine-GITS (gastrointestinal therapeutic system) to patients with arterial hypertension - is no less effective and safe than treatment with diuretics. Additional analysis conducted as part of this study showed that nifedipine has a positive effect on the prognosis of patients’ lives, and the severity of this effect of nifedipine is not inferior to that of diuretics [13].
Conclusion
Thus, the data available today convincingly indicate the effectiveness and safety of treatment with long-acting calcium antagonists
patients with arterial hypertension.
In some cases, when taking other antihypertensive drugs is contraindicated, these drugs may be the drugs of choice. The ability to prescribe these drugs once a day makes them very convenient for long-term regular treatment. References:
1. Abernethy DR. The pharmacokinetic profile of amlodipine. Burges RA, Dodd MG, Gardiner DG Pharmacologic profile of amlodipine Am J Cardiol 1989; 64:101–201 Am Heart J 1989; 118:1100–1103.
2. Burges RA, Dodd MG, Gardiner DG. Pharmacologic profile of amlodipine. Am J Cardiol 1989; 64: 101–201.
3. Packer M., O'Connor C., Ghali J. et. al. Effect of amlodipine on morbidity and mortality in severe chronic heart failure. New. Engl. J. Med. 1996;335:1107–1114.
4. Halperin AK, Icenogle MV, Kapsner CO et al. A comparison of the effects of nifedipine and verapamil on exercise performance in patients with mild to moderate hypertension. Am. J. Hypertens. 1993; 6: 1025 – 1032.
5. Zannad F, Matzinger A, Laeche J. Through/peak ratios of once daily angiotensin converting enzyme inhibitors and calcium antagonists. Am J Hypertens 1996; 9:633–643.
6. Levy D, Garrison RJ, Kannel WB, Castelli WP: Prognostic implications of echocardiographically determined left ventricular mass in the Framingham Heart Study. New Engl J Med 1990; 322:1561–1566.
7. Dahlof B, Pennert K, Hansson L: Reversal of left ventricular hypertrophy in hypertensive patients. A meta analysis of 109 treatment studies. Am J Hypertens 1992; 5:95–110.
8. Islim IF, Watson RD, Ihenacho HNC, Ebanks M, Singh SP: Amlodipine: Effective for the treatment of Mild to Moderate Essential Hypertension and Left Ventricular Hypertrophy. Cardiology 2001; 96: 10–18.
9. Leenen FHH, Fourney A, Notman G, Tanner J. Persistence of antihypertensive effect after missed doses of calcium antagonist with long (amlodipine) vs short (diltiazem) harf–life. Br.J.Clin.Pharmacol.1996; 41:83–88.
10. Zannad F, Bernaud CM, Fay R. Double–blind, randomized, multicentre comparison of the effects of amlodipine and perindopril on 24h therapeutic coverage and beyond in patients with mild to moderate hypertension. Journal of Hypertension 1999; 17:137–146
11. Zannad F., Boivin JM, Lorraine General Physician Investigators Group. Ambulatory 24–h blood pressure assessment of the felodipine–metoprolol combination versus amlodipine in mild to moderate hypertension. J.Hypertens. 1999;17:1023–1032.
12. Hansson L., Zanchetti A., Carruthers SG et al. Effects of intensive blood–pressure lowering and low dose aspirin in patients with hypertension: principal results of the Hypertension Optimal Treatment (HOT) randomized trial. Lancet 1998;351:1755–1762.
13. Brown MJ, Palmer CR, Castaigne A. et al. Morbidity and mortality in patients randomized to double–blind treatment with a long–acting calcium–channel blocker or diuretic in the International Nifedipine GITS study: Intervention as a Goal in Hypertension Treatment (INSIGHT). Lancet 2000;356:366–372.