Determination methods
To determine a person's blood type, the agglutination method is used, in which a set of antigens (or agglutinogens) that are located on the surface of red blood cells is determined.
If foreign antibodies enter the body, our body begins to produce special proteins. The classification of AB0 groups (the main system for dividing blood groups in humans) is based on whether α and β proteins are absent or present.
Agglutination method
You can find out which blood type is suitable for all people by the result of agglutination (clumping of red blood cells). A few drops of blood are dropped into the serum containing proteins α, β, α and β. The blood transfusion procedure is performed only in a clinical setting.
Based on the result of the reaction, they determine which group the blood belongs to:
- if there is no reaction - blood group 1. Almost 50% of the planet's inhabitants are its carriers;
- in the case when the reaction is present in the serum α and α+β – blood group 2. About 40% of people have this type of blood;
- if agglutination occurred in serum β and α+β - blood group 3. Approximately 8% of residents have it;
- the reaction is present in all three test tubes - blood group 4. Only 2% of people have this group.
ABO and RH system
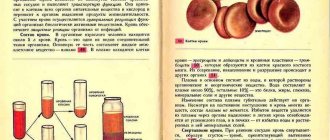
The main blood classification is the AB0 system, which was discovered in the early 20th century. They are determined by the presence on the surface of red blood cells of specific antigens (agglutinogens) A and B. One of their tasks is to signal the presence of foreign elements, thereby causing an immune response in the body. The immune system does not react in any way to its own antigens, but when those that are not in the body appear, it mistakes them for enemies and begins to destroy them. The body produces antibodies (immunoglobulins) to foreign antigens, and as a result of their reaction, red blood cells stick together.
The set of antigens found on red blood cells determines membership in one group or another. In fact, doctors know about 400 antigens, and therefore there are quite a few classifications. However, the properties of most antigens are weakly expressed and are not taken into account during transfusion. During blood transfusions, the greatest attention is paid to the AB0 and Rh systems.
According to the AB0 system, blood is divided into four groups. The first has neither one nor the other antigen, the second has only A, the third has B, the fourth has both antigens - A and B. Natural antibodies (agglutinins) are present in the plasma - anti-A and anti-B (α and β ). Only opposite antigens and antibodies can be present in the blood. The first contains anti-A and anti-B, the second contains anti-B (β), the third contains anti-A (α), and there are no antibodies in the plasma of the fourth.
The table clearly demonstrates this.
| Group | Agglutinogen in red cells | Agglutinin in plasma |
| I | absent | anti-A and anti-B |
| II | A | anti-B |
| III | B | anti-A |
| IV | AB | absent |
According to the Rh system, blood can be Rh positive or Rh negative. This depends on the presence of a specific Rh factor antigen on the surface of red cells. If the blood of the donor and the patient belongs to the same group, but one is Rh-positive and the other is Rh-negative, incompatibility occurs.
The process of determining blood identity
An important point in transfusion is to determine the identity of the biological fluid and the presence of infections in it. To do this, a blood sample is taken for a general analysis, the resulting amount is divided into two parts and sent for research. In the laboratory, the first one will be checked for the presence of infections, the amount of hemoglobin, etc. The second one is used to determine the blood type and its Rh factor.
How is blood transfused to a patient?
Blood transfusion occurs through veins; in rare, severe cases, a blood transfusion machine is used through an artery. Nowadays in medicine both the direct transfusion method (directly from the donor to the recipient) and the method with preliminary collection are used. Those. Blood that has been stored for some time in a blood donor bank is also transfused. Modern medicine transfuses not just blood in bulk, but a specific component needed by the recipient:
- plasma,
- leukocytes,
- platelets,
- red blood cells,
- other rare blood components.
To carry out a transfusion, donor blood undergoes careful monitoring by doctors in order to exclude any dangerous pathogens, viruses or infections, as well as the compatibility of not only groups, but also Rh factors, so as not to cause a conflict in the recipient.
What are the indications for blood transfusion?
Signs of incompatibility
If the victim is infused with inappropriate donor biomaterial, this will cause specific symptoms. More often there are such deviations:
- Study: which blood type is considered the best: positive and negative aspects
- The patient becomes restless.
- The occurrence of discomfort and sharp pain in the lumbar region. This marker indicates that changes have begun to occur in the kidneys.
- Pallor of the skin.
- Increased breathing, shortness of breath.
- Increased body temperature or chills from feeling cold.
- Hypotension.
- Bacterial toxic shock. The violation is rare and occurs due to infection during transfusion.
5% show the following symptoms:
- Nausea and vomiting.
- Turning blue.
- The occurrence of severe convulsions.
- Involuntary urination and defecation.
In rare cases, there is a possibility of hemolytic shock. With this complication, it is necessary to immediately save the patient.
Indications for blood transfusion in a patient
Blood transfusion is applicable when it is not possible to replace it with other methods of treatment. Of course, severe blood loss is an absolute indication for transfusion. Typically, the volume of donated blood is 500-3000 ml, depending on the needs of the recipient. Blood transfusion is also possible if the need for blood is greater than 3 liters.
However, there are a number of contraindications to the transfusion procedure:
- liver and kidney dysfunction,
- injuries associated with cerebral circulation - hemorrhages, concussions,
- allergy,
- active stage of tuberculosis,
- disruption of the cardiovascular system.
Now you know what blood transfusion is intended for and what indications exist for it.
Algorithm for blood transfusion
ABO system The main antigens of the ABO system are 2-A and B. As separate specificities, 2 more antigens are distinguished in it - A, B and A1. The absence of these 4 antigens on red blood cells is designated O. Anti-A and anti-B antibodies are of natural origin. They are designated by the Greek α and β. There are 4 blood groups formed by combinations of antigens A and B with isohemagglutinins α and β. On red blood cells of the first group O (I), antigens A and B are absent, the plasma contains antibodies α and β. In the second blood group A (II), the erythrocytes have antigen A, and the plasma contains β antibodies. The third group B (III) contains the B antigen and α antibodies. In the fourth group AB (IV), antigens A and B are present; isohhemamaglutinins α and β are absent in the blood serum.
Rh factor
Rh factor is an antigen found in the red blood cells of 85% of people, as well as in Macaus rhesus monkeys. The blood of people whose red blood cells contain Rh is called positive. There are several different antigens of the Rh system, including the Hr group, which forms a common system with Rh. Rh-Hr Including -3 varieties of Rh agglutinogen (C, D, E) -3 varieties of Hr agglutinogen (c, d, f) and other rarer species. Agglutinogen Hr is found in the red blood cells of 83% of people. The Rh factor is inherited as a dominant trait and does not change throughout life. The transfusion of blood components has the right to be carried out by: - The attending physician or the doctor on duty. -During the operation, the surgeon or anesthesiologist (not involved in the operation or anesthesia). -Doctor of the blood transfusion department or room. -Transfusiologist.
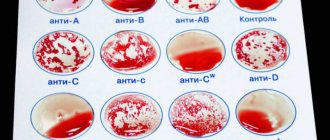
Determination of blood group according to the ABO system (Using coliclones) - 2 drops (0.1 ml) of the reagent and next to one drop of red blood cell sediment (0.02 - 0.03 ml) - Serum and red blood cells are mixed with a glass rod - The plate is periodically shaken, observing the progress of the reaction for 5 minutes (allows you to identify the weak agglutinogen A2) - interpret the results
Difficult to determine blood types
Blood subgroups. Antigen A, contained in erythrocytes of groups A (II) and AB (IV), can be represented by two variants (subgroups) - A_1 and A_2. Antigen B has no such differences. Nonspecific agglutination of erythrocytes. It is judged on the basis of the ability of erythrocytes to agglutinate with sera of all groups, including AB (IV). Nonspecific agglutination is observed in autoimmune hemolytic anemia and other autoimmune diseases accompanied by the adsorption of autoantibodies on erythrocytes, in hemolytic disease of newborns, whose erythrocytes are loaded with maternal alloantibodies.
Blood chimeras. Blood chimeras are the simultaneous presence in the bloodstream of two populations of red blood cells that differ in blood type and other antigens. Transfusion chimeras arise as a result of repeated transfusion of red blood cells or suspension of group 0 (I) to recipients of another group. True chimeras occur in heterozygous twins, as well as after allogeneic bone marrow transplantation. Other features. Determining the AB0 blood group and Rhesus affiliation can be difficult in patients due to changes in the properties of red blood cells in various pathological conditions (in patients with liver cirrhosis, burns, sepsis). Determination of Rh-belonging
Apply a large drop (about 0.1 ml) of reagent to the plate. A small drop (0.02-0.03 ml) of the red blood cells being tested is placed nearby. Mix the reagent with red blood cells thoroughly using a glass rod. Rock the record gently. The reaction results are taken into account 3 minutes after mixing. If agglutination is present, the blood being tested is labeled as Rh positive; if not, it is marked as Rh negative.
Compatibility test on a plane at room temperature
To conduct tests for individual compatibility, the patient’s blood (serum) is used, taken before transfusion or no more than 24 hours before, provided it is stored at a temperature of +4+2°C.
Apply 2-3 drops of the recipient's serum to the plate and add a small amount of red blood cells so that the ratio of red blood cells to serum is 1:10. Next, the red blood cells are mixed with the serum, and the plate is gently rocked for 5 minutes. Compatibility test using 33% polyglucin
Add 2 drops (0.1 ml) of recipient serum, 1 drop (0.05) ml of donor erythrocytes into the test tube and add 1 drop (0.1 ml) of 33% polyglucin.
The test tube is tilted to a horizontal position, shaking slightly, then slowly rotated so that its contents spread over the walls in a thin layer. Contact of erythrocytes with the patient’s serum while rotating the tube should continue for at least 3 minutes.
After 3-5 minutes, add 2-3 ml of physiological solution to the test tube and mix the contents by inverting the test tube 2-3 times without shaking.
The result is taken into account by viewing the test tubes with the naked eye or through a magnifying glass. Agglutination of red blood cells indicates that the blood of the recipient and the donor are incompatible; the absence of agglutination is an indicator of the compatibility of the blood of the donor and recipient.
Technical errors
Incorrect order of reagents. Temperature conditions (blood group determination is carried out at a temperature not lower than 15°C and not higher than 25°C) The ratio of reagents and red blood cells being studied. Duration of observation. (allows us to identify weak agglutinogen A_2, characterized by delayed agglutination)
Biological sample
The biological test is carried out regardless of the volume of the blood transfusion medium and the speed of its administration.
If it is necessary to transfuse several doses of blood components, a biological test is carried out before the start of the transfusion of each new dose. Technique for conducting a biological test: 10 ml of blood transfusion medium is transfused once at a rate of 2 - 3 ml (40 - 60 drops) per minute
observe the recipient for 3 minutes, monitoring his pulse, breathing, blood pressure, general condition, skin color, and measure body temperature
This procedure is repeated twice more. The appearance during this period of even one of the clinical symptoms such as chills, lower back pain, a feeling of heat and tightness in the chest, headache, nausea or vomiting requires immediate cessation of the transfusion and refusal to transfuse this transfusion medium.
The urgency of transfusion of blood components does not exempt one from performing a biological test!!!
The doctor performing the transfusion of blood components is obliged to:
1. Determine the indications for blood transfusion therapy, taking into account contraindications.
2. Obtain informed voluntary consent of the recipient or his legal representative to conduct blood transfusion therapy in the prescribed form.
3. Conduct an initial determination of the patient’s blood group according to the ABO system.
IT IS STRICTLY PROHIBITED TO USE DATA ABOUT GROUP MEMBERSHIP FOR THE ABO AND RHESUS SYSTEMS FROM THE PASSPORT, PREVIOUS ILLNESS HISTORY AND OTHER DOCUMENTS.
4. Include in the referral to the clinical diagnostic laboratory (form No. 207/u) information about the result of determining the blood group according to the ABO system, a series of diagnostic tests, transfusion and obstetric-gynecological history. Sign the direction
5. Familiarize yourself with the conclusion of the clinical diagnostic laboratory. Transfer data about the group and Rh affiliation of the patient to the front part of the inpatient medical card, indicating the date of the analysis and your last name.
6. Prepare a pre-transfusion epicrisis.
7. Conduct a macroscopic assessment of laboratory gelatin and diagnosticums.
8. Conduct a macroscopic assessment of each dose of blood transfusion medium.
9. Immediately before transfusion, determine the recipient’s blood group according to the ABO system.
10. Determine the blood group according to the ABO system with erythrocyte-containing medium.
11. Check the compliance of passport data.
12. Conduct a compatibility test between the recipient’s blood and the donor’s blood (transfusion medium) according to the ABO and Rh systems.
13. Record the results of isoserological studies in the protocol of the blood transfusion operation.
TESTS FOR INDIVIDUAL COMPATIBILITY ACCORDING TO THE ABO AND RHESUS SYSTEM DO NOT REPLACE EACH OTHER.
ARE CARRIED OUT IN ALL CASES WITH BLOOD SAMPLES FROM EACH CONTAINER.
MANDATORY EVEN IF THE ERYTHROCYTE MASS OR SUSPENSION IS SELECTED FOR THE RECIPIENT INDIVIDUALLY IN A SPECIALIZED LABORATORY.
14. Conduct a biological test. Record its result in the protocol of the blood transfusion operation.
15. Monitor the condition of the recipient, the rate of administration of the transfusion medium.
16. If the patient’s condition changes, first of all, exclude a post-transfusion complication.
17. Assess blood pressure, pulse, thermometry results.
18. Register blood transfusion:
•in the observation diary of the medical record of an inpatient;
• in the register of registration of blood transfusions and its components (form No. 009/u);
•fill out the blood transfusion protocol
19. Conduct a macro-assessment of the first portion of urine.
20. Prescribe clinical blood and urine tests the next day after blood transfusion.
21. Assess daily diuresis, water balance, results of urine and blood tests.
22. Observe the patient and reflect the observation results in the medical history diary. If clinical symptoms and laboratory parameters change before the patient is discharged from the hospital, first of all exclude a post-transfusion complication.
Complications - Immune complications (acute hemolysis, hyperthermic non-hemolytic reaction, anaphylactic shock, non-cardiogenic pulmonary edema)
-Non-immune complications (acute hemolysis, bacterial shock, OSHF, pulmonary edema)
- Immediate complications (alloimmunization with antigens of erythrocytes, leukocytes, platelets or plasma proteins, hemolysis, graft-versus-host disease, post-transfusion purpura)
Long-term complications
-Immune (hemolysis, Graft-versus-host disease, Post-transfusion purpura, Alloimmunization with antigens of erythrocytes, leukocytes, platelets or plasma proteins
Literature:
A. G. Rumyantsev, V. A. Agranenko. Clinical transfusiology-M.: GEOTAR MEDICINE, 1997.
E. B. Zhiburt. Transfusiology-S.: PETER, 2002.
Regulations and audit of blood transfusion. Guide for doctors. -M. , RANS, 2010.
Ragimov A. A. Transfusiology . National leadership-M.: GEOTAR Media, 2012.
S. I. Donskov, V. A. Morokov. Human blood groups: Guide to immunoserology - M.: IP Skorokhodov V. A., 2013.
Zhiburt E. B. Patient blood management//Healthcare. -2014.
Algorithms for studying erythrocyte antigens and anti-erythrocyte antibodies in difficult to diagnose cases. Methodological recommendations N 99/181 (approved by the Ministry of Health of Russia on May 17, 2000)
Order of the Ministry of Health of Russia dated November 25, 2002 N363 “On approval of the Instructions for the use of blood components”
Order of the Ministry of Health of Russia dated 04/02/2013 N183н “On approval of the rules for the clinical use of donor blood and (or) its components”
History of the 4th group
The opinions of scientists regarding the relatively recent appearance (no earlier than the 11th century AD) of the 4th Civil Code are divided. But there are three main theories:
- Mutation of the 2nd and 3rd groups into the 4th as a result of the mixing of races: Indo-European and Mongoloid, which were characterized by individual characteristics that appeared during a long evolutionary process. This mixing began recently, which explains the youth of the fourth group.
Mixed marriage of Indo-European and Mongoloid races
- Another version: the emergence of the 4th group is associated with humanity’s opposition to viruses that threatened the complete destruction of the earth’s population. The response to such attacks was the development of appropriate antibodies that combine A and B.
- According to the third theory, the young fourth group was formed as a defense for the body during the evolution of the culture of eating. As food processing methods became more complex, the need arose to combine antigens A and B, which should protect the body from unnatural food preferences.
Disagreements regarding the truth of the theory of the origin of the 4th group still exist in the scientific community. But there is unity regarding the rarity of this blood.
Interesting! Carriers of different HAs have characteristic agglomerations. The first and second groups are characteristic of the inhabitants of Africa and Europe, and the third - of Asia and Siberia. The 4th GC is characteristic of the inhabitants of Southeast Asia, Japan and Australia. Traces of AB (IV) were found on the Shroud of Turin.