Surely every person has encountered people in their life who are constantly freezing. Even in the summer, when everyone around is trying to bare as much as possible so that it is not so hot, these men and women can wrap themselves up in woolen sweaters and wear thick trousers. Constant chills without fever is a feature that is most often inherent in girls and women of asthenic physique. However, sometimes strong representatives of the stronger sex, who at first glance are simply bursting with health, also suffer from chills.
Why does this happen? First of all, it should be noted that chills and weakness in themselves are not a disease - they are nothing more than symptoms. They may indicate that the patient has an endocrine or infectious disease, as well as a benign or malignant neoplasm in the body. In addition, chills often bother those people in whom an inflammatory process develops in the body, which is accompanied by suppuration.
Most common causes of chills
The first thought that appears in a person who notices a headache, chills and weakness is that he has an acute respiratory viral infection or the flu. The patient's body has to produce a large amount of heat, so in most cases the temperature rises in such patients. These symptoms may be accompanied by a runny nose, headache, aching bones and other signs of illness. Under no circumstances should you suffer from discomfort on your legs! Seek medical help and start treatment as soon as possible.
Often the feeling of cold in people with a hypersensitive nervous system is accompanied by severe anxiety. In addition, this may be a consequence of fright. This is a temporary symptom - as soon as a person manages to relax and calm down, he stops freezing. In many cases, chills without fever are a common companion for those people whose working blood pressure is below normal. In addition, in women, the cause of chills can be the first days of the menstrual cycle, as well as the beginning of pregnancy.
Often the cause of chills is all sorts of disturbances in the patient’s peripheral circulation. Especially many of these people live in regions where damp, cold weather is the norm. In such patients, the blood supply to the fingers of the upper and lower extremities is reduced. This can be visually determined by redness and swelling of the skin. Symptoms include severe itching.
People who have been diagnosed with diabetes mellitus are familiar first-hand with the unpleasant sensations that accompany chills. In addition, this symptom may indicate that the patient has other types of endocrine diseases. For example, in patients with insufficient thyroid function, the following symptoms may be associated with chills and headaches:
- hair loss up to baldness;
- a sharp increase in body weight up to obesity;
- mood swings from complete euphoria to hysteria and depression;
- excessively dry skin on the face and body;
- weakness, drowsiness, decreased performance, etc.
The feeling of cold is associated with insufficient production of hormones by the gland, which results in impaired thermoregulation. In addition, similar symptoms are often observed in women aged 50 years and older. This is associated with menopause.
Finally, patients with VSD often suffer from chills and weakness. They can be cold even in July, when everyone is wearing light dresses, shorts, T-shirts and flip-flops. The fact is that people suffering from vegetative-vascular dystonia may have seriously impaired thermoregulation. Such patients need to visit saunas and baths more often, and also start each morning with a contrast shower. During the cold season, swimming in an ice hole can help them strengthen blood vessels and improve thermoregulation. Finally, a massage course conducted by a qualified specialist can play the role of an “ambulance” for such people and temporarily relieve them of chills.
Please note that the above methods of healing the body are not suitable for people suffering from cardiovascular diseases.
Ways to normalize the condition
When a person suffers from high blood pressure for a long period of time, accompanied by accompanying symptoms, one should immediately seek help from a hospital as quickly as possible. If the pressure has increased sharply, the patient should lie down, try to calm down and take an effective medicine. This way he won't have to endure suffocation. To do this, it is also better to open a window so that the body tissues receive a sufficient amount of oxygen.
After the ambulance arrives, doctors will use certain manipulations to lower blood pressure and give advice such as:
- if deviations are accompanied by pain in the heart, you should take Corvalol or Validol;
- a person can wet a towel with apple cider vinegar, which helps reduce blood pressure and get rid of chills within 10 minutes from the start of the procedure;
- When the doctors leave, you can try to warm your feet using a blanket, heating pad, or warm socks.
If chills occur against the background of a hypertensive crisis, doctors advise taking No-shpa or Drotaverine, and then Valocordin. Next, you should lie down in bed as comfortably as possible and relax. The trembling will disappear gradually due to normalization of blood pressure. Doctors do not advise getting up and doing anything for at least 1.5-2 hours.
Folk remedies
To cope with chills and high blood pressure, people successfully use folk methods using medicinal herbs. Each of them has sedative, vasodilator and diuretic properties. Herbal infusions are brewed like regular tea and drunk warm. These drinks can be stored for a maximum of 2 days in the refrigerator. If possible, it is better to take a single dose and not store the tea at all.
To achieve the fastest possible effect, use rose hips, calendula, peppermint, strawberry leaves, hibiscus, chamomile and valerian root. The most common are herbal mixtures selected as a complex.
To combat a hypertensive crisis, you can use the following formulations:
- Black elderberry flowers and hawthorn fruits.
- Chamomile, valerian root, peppermint and fennel.
- Dill seeds, motherwort and chamomile.
- St. John's wort, valerian and oregano herb.
- Mint leaves, calendula flowers and linden.
Medicines
The patient should not prescribe each of the medications independently. This is done by the doctor, based on an early examination. If the patient does not take into account the individual characteristics of his body and contraindications, taking pills can greatly aggravate his condition.
If you need to lower your blood pressure urgently, the specialist will prescribe the following medications:
- Enalapril;
- Furosemide;
- Adelfan;
- Anaprilin;
- Captopril.
Speaking about longer-term treatment, it is relevant to use the following:
- Propranolol;
- Metoprolol;
- Prestarium;
- Diroton;
- Cordaflex;
- Losartan.
How to get rid of chills?
If chills are caused by the penetration of a viral infection into the body, then it is necessary to devote all efforts to treating the disease. Adhere to the treatment regimen prescribed by your doctor and follow all his recommendations. Bed rest in combination with taking pharmaceuticals, including antipyretics, gargling and drinking plenty of fluids will help get rid of all manifestations of the disease in a matter of days.
How to get rid of chills caused by any endocrine diseases? To do this, you need to see a doctor, undergo an examination and begin treatment for identified problems in the body under the strict guidance of a specialist. In our private clinic in Ryazan, the best endocrinologists of the city, as well as doctors of other specialties, see patients every day. The diagnostic department of ON CLINIC in Ryazan is equipped with the latest medical technology. Our examination will not take much time and will allow you to learn everything about how your body works!
If the cause of chills is being under stress or being very excited in anticipation of some event, then drinking hot tea, preferably herbal tea with lemon balm or chamomile, will help you relax, calm down and warm up. In addition, you can take a mild sedative, such as valerian. But do not overuse medications - consult a doctor and get examined! Based on its results, the doctor will prescribe you effective treatment.
Be that as it may, constant chills are not just a feature of the body, but rather a symptom that something is wrong in its functioning. Make an appointment with us, and our qualified specialists will be able to identify the cause of chills and eliminate it!
How does the body's response to change develop?
When people complain of chills with high blood pressure, but the body temperature is normal, the muscles of the body begin to suddenly contract spastically, causing tremors that initially appear in the masticatory muscle, and then in all other places. Speaking about the reactions occurring in the body itself, there is an increase in glucose concentration and rapid breakdown of fat cells due to the synthesis of adrenaline. This means that the temperature may drop, causing a feeling of coldness and trembling throughout the body.
Symptoms of nocturnal hypertension
If your blood pressure rarely rises at night, there is no reason to worry. With persistent hypertension at night, a detailed clinical and laboratory examination is needed to establish the root cause. The pathology has no characteristic symptoms. According to blood pressure indicators, it is divided into three stages:
- up to 160/100 – initial: insomnia, headache, chest discomfort;
- up to 180/110 – severe symptoms: shortness of breath, spots in the eyes, angina pectoris, decreased ability to work;
- 200/120 and above – stage of complications: symptoms of affected target organs: deterioration of hearing, vision, memory, heart failure, nephropathy.
At night there may be attacks of suffocation and a feeling of fear.
Factors that provoke a rise in pressure
Systolic and diastolic pressure varies from person to person. The norm is considered to be the numbers at which he feels comfortable. The most dangerous period for the patient is between three in the morning and six in the morning.
A constant increase in pressure at this time leads to vascular disasters.
Hypertension is called an indicator of the social well-being of society. This is true, since today it is diagnosed in almost half of the world's inhabitants. But nocturnal hypertension illustrates this statement especially accurately. Provoke its development:
- heredity (especially in the first line: mother, father, brother, sister, grandfather, grandmother);
- gender - hypertension is gender-specific and more often affects men, since male sex hormones stimulate a rise in blood pressure, men have more muscle mass, which means the volume of blood flow, which naturally increases blood pressure, they work harder physically, and do not always have time during the night recover;
- stress - adrenaline, norepinephrine (stress hormones) cause tachycardia, which automatically creates a load on the myocardium, forcing it to pump more blood, leaving a minimum of time for rehabilitation;
- bad habits - drinking alcohol in the evening or smoking a cigarette at night increases blood pressure by 5 units per year, based on vasospasm, hypoxia of tissues and organs;
- physical inactivity – lack of regular physical activity increases the risk of hypertension by 50%; an untrained heart is not able to fully recover overnight;
- excess weight is the scourge of modern society: overeating at night increases the risk of arterial hypertension by 6 times (!) - every extra 500 g causes an increase in blood pressure by one (in Russia, 30% of the population suffers from obesity);
- salt - love for salted cabbage, cucumbers, vobla, caviar, mayonnaise - the national eating habits of Russians, all this leads to water retention in the body and stress on blood vessels; salty food at night increases the risk of developing serious complications three times.
The conclusion is obvious: the higher the quality of life of an ordinary person, the lower the risk of developing hypertension.
Treatment methods for nocturnal hypertension
How to treat nocturnal hypertension depends on the stage of the disease. At the initial stage, lifestyle changes, diuretics (Clopamide, Furosemide) and sedatives of plant origin are sufficient. The main goal is to reduce the load on the blood vessels. Patients should completely review their diet and limit salt intake, especially after lunch. Avoid consuming caffeinated drinks and strong tea.
As a diuretic, you can use a decoction of rose hips, tansy, and mint. Taking sedatives can reduce brain activity and relax the central nervous system, thereby normalizing blood pressure. Alcohol tinctures of peony, valerian, and motherwort improve the natural process of falling asleep.
Drug therapy for stages 2-3 of nocturnal hypertension
Treatment of nocturnal hypertension in the second and third stages is carried out with medications. Shown:
- calcium antagonists (Corinfar, Felodipine) - help improve the condition of the tissues of the vascular walls;
- direct renin inhibitor (Methiopril, Capoten) - reduces the secretion of renin by the kidneys, helps reduce the rate, reduce the volume of circulating plasma;
- beta blocker (Matoprolol, Viske) - affects the receptors, the vessels deflate, weaken, and cease to provide resistance to the periphery.
Medicines that lower blood pressure should be taken schematically.
In each individual case, the duration of use and dosage are determined by the doctor. Independent uncontrolled use of such drugs can cause a crisis. Calcium antagonists should be taken with caution. The medicine has many side effects and can cause swelling of the face, arms, legs, and dizziness.
In addition, B vitamins are prescribed to restore central nervous system cells, and magnesium to normalize heart rate.
Diet
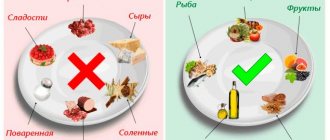
Table No. 10 is recommended for hypertensive patients. The diet allows for consumption:
- any types of vegetable crops, raw, boiled, steamed, stewed;
- fruit salads, fresh juices, smoothies;
- meat, fish and dairy products with reduced fat content;
- whole grain bread made from rye flour, crispbread;
- legumes, mushrooms, cereals;
- It is better to replace sweets with jam, honey, pure sugar (allowed to be consumed in small quantities).
Nocturnal hypertension of 2-3 degrees uses a salt-free diet as an additional measure in treatment. Everything that comes to the table of a hypertensive patient must be carefully checked. Severe swelling can be relieved by reducing your daily water intake.
After suffering a hypertensive crisis, it is better to refuse food for a day. You can eat fruits or vegetables; meat and fish broths are strictly prohibited. Dishes are prepared without salt. Together with the first courses, the daily water consumption rate is 1 liter.
Arterial hypertension - features
The disease can be completely asymptomatic, then the person is not aware of the presence of high blood pressure. But in the absence of symptoms, the risk of complications is just as high as with negative symptoms (headache, dizziness, nausea, vomiting, etc.)!
An advanced condition means a high risk of stroke and heart attack, which can lead to disability and even death (according to WHO, death from cardiovascular pathologies ranks first in the world). The early stage of the disease, controlled by measuring blood pressure and taking special antihypertensive drugs, vitamin complexes and natural dietary supplements for the heart and blood vessels, is reversible, in contrast to advanced forms of the disease, which are dangerous to health and life.
The home medicine cabinet must contain first aid for a hypertensive crisis and antihypertensive drugs for regular use if a diagnosis of arterial hypertension is made. If your condition worsens, when your blood pressure rises sharply and suddenly, there is no way to urgently run to the pharmacy or see a doctor. Medicines for hypertension should always be available! Buy quality medications at affordable prices in Stolichka pharmacies.
Diagnostic methods
Headache, nausea and vomiting, chills and fever are signs of infectious and non-infectious diseases that require different treatment methods. To prescribe the optimal regimen, it is important to determine the cause of these symptoms. After the examination, the doctor prescribes additional examinations that will help make a final diagnosis:
- Ultrasound of the stomach and intestines is the first way to determine inflammatory processes;
- endoscopic examination of the mucous membrane of the stomach and intestines;
- magnetic resonance or computed tomography – methods for diagnosing the brain to detect tumors;
- measuring blood pressure during the day;
- Ultrasound of the heart, electrocardiography - prescribed for suspected heart failure and other diseases;
- blood tests - will help determine inflammatory diseases and dysfunction of individual organs;
- specific blood tests to determine glucose levels.
At the Clinical Brain Institute, the examination regimen is prescribed individually. It does not include any unnecessary, insufficiently informative tests that will not help assess the overall picture of the disease. Modern equipment allows you to obtain the most accurate data necessary for diagnosis.
Complications
A nocturnal rise in blood pressure can provoke:
- spontaneous cardiac arrest;
- AMI (acute myocardial infarction);
- ACVA (acute cerebrovascular accident of ischemic and hemorrhagic type);
- myocardial fibrillation or fibrillation;
- PE (pulmonary embolism).
The reason is simple: if the pressure rises, but it does not naturally decrease, the internal organs do not have time to recover from overload during the day, so the heart, brain, kidneys, and liver experience hypoxia and do not receive the necessary nutrients. The risk of death with hypertension increases by 30%.