Angioma is classified as a benign neoplasm. It is located along the venous and lymphatic vessels. More often it is a congenital tumor, which for the time being does not make itself felt.
Venous angioma is a type of lesion of the vein wall. Together with the cavernous appearance, it represents 2 types of structural changes. Some authors consider them to be a single form, at different stages of development.
The danger of this neoplasm is associated with possible complications in the form of rupture with hemorrhage and compression of important centers when the venous angioma is located inside the brain. There are descriptions of cases of thrombosis.
In ICD-10, hemangiomas, regardless of location, are coded D18.0 and classified as neoplasms.
Why do angiomas form?
Angiomas can be either congenital (95% of cases) or acquired (5%). The exact reasons have not yet been clarified. The most proven versions are:
- disruption of the intrauterine formation of the vascular system due to maternal illness, vitamin deficiency, pathological pregnancy;
- concomitant pathology of organs with a high risk of cancer (stomach, liver, mammary glands, lungs, uterus and prostate), this confirms the connection with liver cirrhosis;
- head injuries;
- infectious diseases suffered in early childhood.
It has been proven that children are more prone to the spread and growth of angiomas than adults. This is associated with the functional inferiority of various body systems and insufficient immunity.
Causes of angioma formation
Angioma in newborns is a standard clinical picture, since this disease in most cases is congenital. The source of the development of neoplasms in adulthood are persistent fetal anastomoses located between the veins and arteries. The proliferation of blood vessels in a benign tumor leads to the growth of the tumor itself.
The causes of angioma are as follows:
- hereditary predisposition;
- changes in hormonal levels;
- diseases of the gastrointestinal tract;
- dysfunction of lipid metabolism;
- skin pigmentation disorders.
In rare cases, venous angiomas of the skin occur after trauma to the skin area (bruises, cuts). They can also accompany malignant neoplasms of internal organs and cirrhosis of the liver.
How does a vascular tumor form?
More often, angiomas are formed by purely venous channels. But the process can also affect the arterial network. A normal vasculature connects arteries and veins through extensive branching of capillaries.
In 5% of cases of disease, the arterial part is directly connected to the vein, it turns out that the affected vessel “steals” other branches and disrupts the general blood flow in the area of location, and each tumor is an arteriovenous fistula
Pathology occurs in the late stage of formation of cerebral vessels in the fetus, from 40 to 90 days of pregnancy.
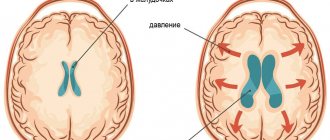
Forming angiomas have rays, so they are compared to a bicycle wheel. Due to increased filling, thinning of the vein walls occurs. The pressure in them increases and bleeding occurs (red blood cells leak out) if the tumor is located on the surface of the body. But with a deep location in the substance of the brain, hemorrhage occurs in the surrounding tissues.
Vascular malformations of the brain
Types of vascular malformations differ based on their macroscopic and microscopic characteristics. Typically, intracranial vascular malformations are divided into the following 4 groups:
- Capillary malformations (or telangiectasias)
- Cavernous malformations (cavernous angiomas/hemangiomas)
- Venous malformations
- Malformations with arteriovenous shunts
According to the newer classification, 2 more categories have been added: arterial malformations (without the formation of an arteriovenous shunt) and mixed malformations.
Cavernomas can be found in any area of the brain because they can arise anywhere along the vascular bed. Intracranial extracerebral cavernous angiomas sometimes occur, but they are quite rare. Cavernous angiomas are also sometimes found in the spinal cord, most often in association with multiple vascular lesions of the brain.
Main symptoms
Angiomas do not always manifest clinical symptoms. With small sizes and lack of growth, a person does not feel the presence of a vascular tumor (half of the cases); it is discovered by chance. It is very important to suspect the disease at the first signs in order to confirm the diagnosis in time using a hardware examination of the brain and begin therapy.
The main clinical sign is headache. It is permanent in nature and is provoked by overload in physical education and studies. Over time it becomes more intense. Accompanied by:
- dizziness;
- feeling of heaviness, noise in the head;
- impaired sensitivity of the skin;
- nausea and vomiting;
- violation of taste sensations;
- spasms in the limbs, less often epileptic seizures;
- decreased vision;
- impaired speech.
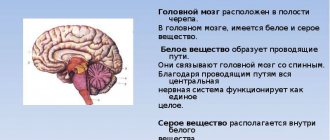
Based on the totality of signs, neurologists can assume the localization of venous angioma. Both hemispheres of the brain, divided into lobes, stem formations have nuclear structures responsible for different functions of the body.
Angioma of the left frontal lobe appears on tomographic sections
In the frontal lobes there are centers that provide analysis of the situation, development of decisions, initiative, assimilation of information and skills.
Venous angioma of the right frontal lobe is accompanied by:
- disturbed by unconscious human behavior;
- decreased performance;
- not depressed mood.
The left frontal localization is characterized by:
- decreased ability to think;
- lack of concentration;
- loss of motivation, unclear reasons for striving for something;
- lack of self-critical assessment of one’s own behavior;
- impaired speech control.
A lesion in the parietal lobe manifests itself:
- impairment or loss of all types of sensitivity (to pain and temperature stimuli, touch);
- when localized in the area of the speech center, misunderstanding of the text read occurs.
The cerebellum is divided into two hemispheres in its structure. They control various functions of the body. Accordingly, venous angiomas located here manifest themselves in different ways.
If there is compression of the right hemisphere by the tumor, the following are observed:
- hand tremors when working;
- impaired handwriting (letters become uneven and of different sizes);
- speech and any movements slow down.
The nature of speech is called “chanted”; it is a slow pronunciation of phrases without intonation.
Symptoms of damage to the left hemisphere are more associated with a stable position in space:
- the patient is worried about dizziness;
- a shaky gait appears;
- inability to maintain balance;
- examination shows nystagmus of the eyeballs (deviation and twitching), impaired skeletal muscle tone.
Another dangerous localization of angiomas is the choroid plexus of the spinal cord
The patient experiences intense back pain, partial or complete paralysis.
Tumor formation and its types
With angioma, the cells of the vascular body divide, increasing the growth of venous tissue. A benign process occurs in vascular and lymphoid tissues:
- On the inside;
- On the outer surface;
- Simultaneously in both types of epithelium.
The neoplasm is divided by type into two classifications:
- In appearance;
- By source of education.
Division of neoplasms by appearance
- Flattened - a spot of varying sizes with a reddish tint. The main place of distribution is in the neck and face.
- Lumpy - an irregularly shaped speck of dark color. Affects the epidermis and mucous membranes. Inherent in childhood, resolves after eight years.
- Cavernous, or deep, type - growth is directed deep into the layers of the skin. In superficial places, the color varies from reddish to flesh-colored. The preferred location is internal organs.
Venous angioma
Division by origin
- Normal – the tissue of the vascular channels for blood flow grows.
- Capillary, vascular - formed by the plexus of capillary vessels rising above the dermis layer.
- Pustular or inflamed - mainly formed on the mucous membrane of the inner side of the cheek, tongue or gum.
- Lymphangiomas.
- Glomangiomas - formed from arterioles, usually under the nails of the upper and lower extremities.
- Telangiectasia - small blood vessels on the skin become tortuous, tangled, and red. They are clearly visible through the skin.
- Cobweb-like - looks like a cobweb. The color depends on the pressure in the circulatory system.
- Bacterial – bacterial infection caused by microorganisms of a certain type.
- The cavernous is the main place of formation of a blood vessel; it expands and does not narrow, slowing down the flow of blood. The appearance of new cells increases the risk of bleeding due to abnormal connection with the rest. The main localization is internal organs.
What can provoke hemorrhage?
According to neurosurgeons, the risk of hemorrhage in the case of venous angioma is quite low. It is found in 0.22–0.34% of patients. But when analyzing information from pathologists, it turns out that among all vascular causes of death in patients, rupture of brain angiomas accounts for 60%.
Increase the risk of hemorrhage:
- arterial hypertension;
- physical activity (for women – labor);
- sudden bends, jumps;
- turning the head;
- minor head injuries (bruises);
- stressful situations.
Types of tumors
D18 is a code according to ICD 10, which means any type of angioma by location and origin.
For successful treatment, it makes sense to distinguish between venous and cavernous angiomas. The first type occurs in the veins, as an expansion of one or more venous vessels. The pressure in the veins is low and the walls are quite strong, so the risk of rupture is low.
The cavernous type includes in its structure not only blood vessels, but also small cavities of the brain. The tumor completely fills the caverns, and its boundaries are thin membranes. With this type of disease, there remains a high risk of hemorrhagic stroke with profuse hemorrhage.
For treatment, the location of the tumor, the type of benign or malignant, and the activity of changes in size (constantly growing or has clear, unchanged boundaries) are important.
Diagnostic methods
Medical institutions have sufficient equipment to diagnose venous angiomas of the brain. The most complete information is obtained using the following methods:
- Angiography is a combination of X-ray examination of the skull with the introduction of a contrast agent into the vessels. The image reveals abnormalities in the blood supply to the brain, the location, size of the angioma, and its connection with the vessels.
- Computed tomography is a recognized non-invasive method (does not involve penetration into blood vessels) and is painless. The results are layer-by-layer images of different depths in a two-dimensional version. This increases the diagnostic capabilities of the method.
- MRI (magnetic resonance imaging) - using magnetic radiation and radio waves, images are more accurate and fine details are highlighted.
- For the purpose of differential diagnosis with different types of intracranial hemorrhage (stroke, rupture of aneurysm), a spinal puncture and examination of fluid from the brain canal are performed in specialized hospitals.
The choice of treatment depends on the diagnostic results.
Cavernous angioma or tumor?
Brain scanning using CT and MRI in most cases allows one to clearly distinguish a cavernoma from other brain formations, including tumors of varying degrees of malignancy. However, in some cases, differentiation of these formations represents a diagnostic problem, the solution of which requires extensive experience. In this regard, the ability to attract a highly qualified diagnostician is critical. In addition, high-quality interpretation of CT and MRI images provides a solution to other diagnostic problems: exclusion of surrounding cerebral edema, identification of the severity of hemorrhage, description of details affecting the operability of the cavernoma. If you are in doubt about the diagnosis, you should consult a radiologist from a leading center specializing in brain pathology. A second opinion from such a diagnostician can be very valuable in the differential diagnosis of angiomas and other pathological conditions.
Treatment options for brain angiomas
Predicting the potential severity of angioma is extremely difficult. Doctors focus on the individual location of the tumor and its proximity to the most important centers. They are more relaxed about single asymptomatic small angiomas. With them, people live to old age.
Drug therapy serves as prevention rather than treatment. There are no drugs yet that can destroy the tumor. Painkillers and sedatives are prescribed. They bring at least temporary relief to the patient's condition.
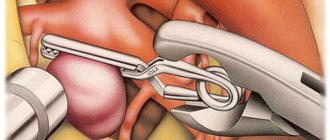
Using stereotaxy, the optimal zone for placing a catheter to the angioma is determined
Surgical removal methods
If the angioma is superficial, it is removed using a gamma knife. The stream of rays stops blood circulation in the angioma area and clogs the blood vessels.
The sclerotherapy technique is based on the introduction of a special sclerosant substance into the affected vessel by a catheter, which promotes sealing and further scarring of the angioma. It stops filling with blood and does not compress the brain tissue.
Selection methods can be:
- vascular plastic surgery;
- embolization or coiling of a vessel by introducing a platinum spiral into the lumen.
Detection of cavernous angiomas
Despite the fact that cavernous angiomas are visualized using computed tomography (CT), this method is not the method of choice: the fact is that the identified signs in a CT study may correspond not only to cavernous angioma, but also, among other possible options, poorly differentiated tumor.
The sensitivity of magnetic resonance imaging (MRI) is much higher, due to its higher contrast resolution, as well as its greater ability to image flowing blood and its breakdown products. The combination of different MRI pulse sequences has largely solved the problem of misdiagnosis or under-detection of cavernous angiomas, since these lesions have quite specific features on MRI.
Get an MRI of the brain in St. Petersburg
CT and MRI can be used for follow-up of patients with already diagnosed cavernous angiomas, especially in cases where there is a risk of hemorrhage. Although the MR image of cavernous angiomas does not predict the occurrence of bleeding, MRI is the method of choice for long-term follow-up of patients with cavernous angiomas, as well as for the evaluation of family members of the patient who are at risk of having such malformations. In addition, MRI is extremely useful in planning surgical intervention, as it allows you to assess the size of the formation, its boundaries, and thus determine the type of operation and surgical approach.
With classical angiography, most cavernous malformations are not visualized, and even when signs are detected, they are extremely nonspecific. If the lesion develops in combination with other vascular malformations, which occurs in approximately 30% of patients with venous malformations, then its MR characteristics become much more complex and less specific. In such patients, angiography may be useful to further clarify the diagnosis.
Prevention
We can only talk about secondary prevention for patients with an already established diagnosis, since primary prevention does not exist. Recommended:
- control blood pressure;
- stop smoking and do not indulge in alcohol;
- women should be careful when choosing contraceptives, oral hormonal drugs contribute to circulatory problems;
- take painkillers and antipyretics only after consulting a doctor; all tablets containing Aspirin increase the risk of hemorrhage;
- avoid severe stress and physical tension;
- organize a good rest.
Possible complications
Due to the growth of venous angioma of the right hemisphere of the cerebellum, a rupture of the wall of the damaged vessel may occur, which will provoke the opening of intracranial hemorrhage with all the ensuing consequences: paralysis on the right side, impaired facial expressions on the side of the damage and other disorders of the motor function of the body.
Therefore, if a patient has been diagnosed with a similar vascular pathology, then he should be as attentive as possible to his health. Namely, it is necessary to eliminate stress from life, prevent an increase in blood pressure, reduce physical stress on the body and not make sudden turns and tilts of the head.
Forecast
The prognosis of the disease depends on:
- patient’s age (presence of other vascular changes);
- concomitant arterial hypertension;
- the nature of professional activity;
- location and size of angioma.
With timely diagnosis and treatment, a person continues to live a full life. Rehabilitation after surgery lasts up to several months. Typically, headaches quickly stop and impaired brain functions are restored. You should not endure headaches and use folk remedies for such a serious illness.
Causes of tumor appearance
The etiology of angiomas is constantly being studied as the disease becomes more common. There are several possible ways for this type of formation to appear in the body:
- congenital defect (hereditary factor), in which the epithelial tissue of the vascular walls grows uncontrollably;
- mechanical injury;
- diseases in which demyelination of the membranes of the brain occurs;
- previous infectious brain disease;
- constant contact with chemicals;
- other types of cancer that have migrated to the brain.
Uncontrolled division of vascular cells (mutation) can stop or accelerate under the influence of external factors (hormonal changes, chemical exposure).
Consequently, symptoms can appear at any age, but it is worth paying special attention to neurological complaints during transitional periods (puberty, menopausal disorders, pregnancy).
Degeneration into a malignant tumor occurs if there has been prolonged contact with a negative environment, a hormonal imbalance has occurred, or malignant neoplasms have appeared in another organ.
Treatment
There are cases when angioma resolves on its own. But often it is necessary to resort to radical methods of treatment, since other methods are ineffective. For example, medications can help relieve painful symptoms, but they cannot untangle the vascular tangle. For this, patients are prescribed painkillers, antihypertensives, and sedatives.
The operation is not performed when diagnosing a small tumor that does not threaten human life, as well as for people with venous angioma, which is characterized by a low risk of choroid plexus rupture.
If the tumor is large and rapidly growing, the following is carried out:
- Traditional way. Removal using a method in which the choroid plexuses are excised.
- Radiosurgical method. Removal of the tumor by blocking the vessels that formed the tangle. In this case, blood will not enter their cavity.
- Sclerotherapy . This method involves blocking the vessels using special catheters through which sclerosing drugs are administered.
- Angioplasty . Allows you to restore the vascular lumen by reconstructing veins and arteries. To restore cerebral circulation and expand the lumen, special metal meshes and balloons are implanted into the affected arteries.
- Liquid embolization . Involves the introduction of a substance into the problem vessels, disconnecting them from the general blood flow. Over time, the damaged vessel is replaced by connective tissue.
- Embolization . This method of treatment allows you to clog and “disconnect” blood vessels from the general circulation by introducing a special spiral.
The choice of one or another method of operation depends on the clinical manifestations, location, size of the tumor, age, and general condition of the patient. Modern specialists try to use minimally invasive treatment methods, as they minimally injure surrounding healthy tissue and significantly reduce the rehabilitation period. Radiosurgical methods using a Gamma Knife or Cyber Knife destroy pathology by exposing it to radio wave beams of radiation.