Causes of renovascular hypertension
Narrowing of the renal artery leads to insufficient blood supply to the renal tissue. Blood supply to the kidney is critically important for the body, otherwise urine is not produced and kidney failure develops. When there is a lack of blood flow in the kidney, the special kidney hormone renin is released, which promotes the conversion of angiotensin I to angiotensin II, which causes a strong narrowing of the arteries and the release of the hormone aldosterone, which promotes sodium retention and increases circulating blood volume and water retention.
If the second kidney functions normally, then this effect can be neutralized and there will be no stagnation of fluid in the systemic circulation, however, with bilateral damage, the volume of fluid in the body and the level of blood pressure increase.
Main diseases leading to renovascular hypertension
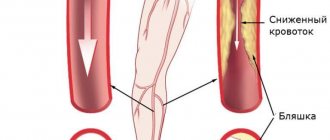
- Obliterating atherosclerosis of the aorta and renal arteries. Most often, atherosclerosis is the cause of renovascular hypertension in elderly men. The examination reveals multifocal atherosclerotic lesions in the coronary arteries and vessels of the lower extremities.
- Fibromuscular dysplasia is the development of narrowing of the arteries due to connective tissue, without atherosclerotic plaque. A uniform narrowing develops in the affected segment, which can then turn into expansion. Young women are most often affected.
- Renal artery aneurysm. Leads to constant embolization of renal tissue by microthrombi, which leads to the development of renovascular hypertension.
- Aortic coarctation is a congenital narrowing in the thoracic aorta leading to decreased perfusion of organs below the narrowing. Most often, arterial hypertension with coarctation of the aorta is of mixed origin.
3. Symptoms and diagnosis
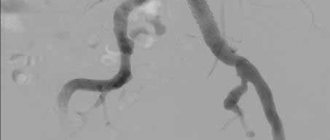
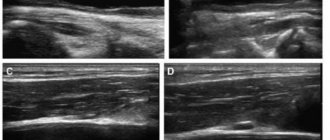
There are some symptoms that are very characteristic of nephrogenic hypertension, but none of them are pathognomonic (characteristic of only one disease and not found in others). Thus, there are sharp and sudden increases in pressure against the background of normal heart rate, therapeutic resistance to conventional antihypertensive treatment (even intensive). However, in general, the symptoms can correspond to any form of arterial hypertension, so diagnosis in this case usually requires the involvement of several related specialists (cardiologist, vascular surgeon, endocrinologist, always an ophthalmologist, etc.). The primary task is to differentiate the renoparenchymal form of hypertension from the renovascular one. The anamnesis is carefully studied, examination, auscultation and percussion are performed, and a detailed and multifaceted laboratory examination is carried out. Of the instrumental diagnostic methods, the most informative are ultrasound, MSCT, various types of contrast urography and angiography (X-ray examination of blood vessels), kidney scintigraphy, radioimmunoassay of renin concentration in the blood, captopril test, etc. It should be noted that if a parenchymal form of renal hypertension is suspected, X-ray examinations should be prescribed with great caution and strictly according to indications, since both radiation exposure and X-ray contrast agents can aggravate damage to renal tissues and structures.
About our clinic Chistye Prudy metro station Medintercom page!
Development mechanism
In the first stage, the immediate increase in blood pressure is a direct consequence of the increase in renin levels in response to impaired renal blood flow. For several weeks, blood pressure remains elevated, but the effect of increased renin levels depends on the function of the contralateral kidney.
Normal functioning of the contralateral side avoids an increase in circulating blood volume despite increased renin levels. Both kidneys are in opposition: the stenotic kidney retains sodium and releases excess renin in response to renal ischemia, while the unaffected kidney excretes excess sodium and water to maintain normal body fluid volume. Thus, there are symptoms of hypertension and elevated renin levels without a significant increase in circulating blood volume (CBV).
In the second stage, ischemia of the affected kidney leads to the retention of sodium and water, which increases the volume of blood volume and allows maintaining perfusion pressure in the kidney. Hypertension becomes less dependent on angiotensin II and is associated with increased sodium and water levels. Renin levels may decrease at this stage.
If blood circulation in the kidneys can be restored during these two stages, then blood pressure soon returns to normal levels.
In the third phase of development of vasorenal hypertension, changes develop in the renal parenchyma, so even elimination of renal artery stenosis no longer leads to complete normalization of systemic blood pressure.
An increase in blood pressure with narrowing of the renal artery is a compensatory mechanism that allows maintaining the filtration and excretory function of the kidney in conditions of reduced perfusion. Therefore, the use of drugs that block the production of angiotensin II (ACE inhibitors) to lower blood pressure can lead to the development of renal failure.
Materials
Arterial hypertension
What is blood pressure?
Blood pressure (BP) refers to the force with which blood presses against the walls of the arteries.
Arteries are blood vessels that carry blood from the heart to all organs. The level of blood pressure is determined by the work of the heart and the diameter of the blood vessels. The optimal blood pressure level is 120/80 mm Hg. Art. A blood pressure level below 130/85 mm Hg is considered normal. Art. High normal pressure is considered to be a pressure of 130-139/85-89 mmHg. Art.
Blood pressure is described by two numbers. The top number indicates the maximum pressure in the arteries during each contraction of the heart, that is, when the heart “works” and throws blood into the vascular bed - this is systolic blood pressure (SBP). The bottom number shows the lowest pressure in the arteries in the interval between heartbeats, i.e. when the heart “rests” and fills with blood before the next contraction is diastolic blood pressure (DBP).
Blood pressure may change throughout the day. Blood pressure is lower when you sleep or lie down, but it rises when you stand up. Physical activity, pain, anxiety or stress can cause a temporary rise in blood pressure, which is completely normal and has nothing to do with arterial hypertension.
What is arterial hypertension?
Hypertension means persistently elevated blood pressure. It is impossible to diagnose high blood pressure using one measurement. To make a diagnosis of hypertension, it is necessary that blood pressure is constantly above normal and that the doctor repeatedly (at least three times) during different visits notes elevated blood pressure numbers.
Arterial hypertension (AH) is a condition in which SBP is 140 mm. rt. Art. or more and/or DBP 90 mm. rt. Art. or more, and these values are obtained as a result of at least three measurements made at different times in a quiet environment without previous use of drugs that change blood pressure.
Increased blood pressure may be a consequence of another disease and then it will be called symptomatic arterial hypertension.
In hypertension, an increase in blood pressure is a symptom of the disease, not its consequence, and is caused by a violation of blood pressure regulation. This type of hypertension is the most common. It accounts for up to 95% of all types of arterial hypertension. The causes of essential hypertension are diverse, that is, many factors influence its occurrence.
Why is high blood pressure harmful to health?
With hypertension, clinical symptoms may be absent, and you may not be aware of high blood pressure for a long time. This is dangerous, because in the blood vessels, and then in the vital organs that they nourish - the heart, brain, kidneys, eyes - serious irreversible damage to their structure and function occurs. Therefore, it is necessary to regularly check your blood pressure at a doctor’s appointment or measure it yourself at home using special devices.
Even a slight increase in blood pressure, despite feeling well, is a reason to take it seriously, since hypertension leads to hypertensive crises, during which the risk of developing a cerebral stroke, myocardial infarction, cardiac asthma and pulmonary edema increases many times over.
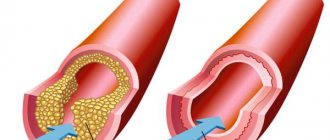
High blood pressure promotes earlier and more active deposition of cholesterol (CH) in the form of plaques in the vessel wall, which accelerates the development of atherosclerosis in the arteries of the heart, brain, organs of vision, and kidneys. An atherosclerotic plaque narrows the lumen of the vessel and impedes blood flow, as a result of which the delivery of oxygen and nutrients to the organs decreases or even partially stops. This aggravates the course of hypertension and leads to the development of coronary heart disease (angina pectoris, myocardial infarction). With hypertension, the walls of the myocardium of the heart thicken (hypertrophy) and the risk of heart failure increases. In the future, in the absence of adequate treatment for hypertension, the walls of the heart may become thinner, their blood supply may be disrupted, shortness of breath, fatigue, and swelling in the legs may appear, i.e. heart failure may develop. Often hypertension leads to impaired renal function or aggravates the course of existing kidney diseases. In the elderly, elevated blood pressure contributes to memory impairment.
High blood pressure, despite the absence of any symptoms, has an adverse effect on target organs.
Types of symptomatic arterial hypertension
Renovascular hypertension
Renovascular (renal) hypertension occurs when the renal artery narrows, when an insufficient amount of blood enters the kidneys and the kidneys synthesize substances that increase blood pressure. Narrowing of the renal artery occurs with atherosclerosis of the abdominal part of the aorta, if the lumen of the renal artery is blocked, atherosclerosis of the renal artery itself with the formation of plaques narrowing its lumen, blockage of the artery by a thrombus, compression of the artery by a tumor or hematoma, trauma, inflammation of the wall of the renal artery. Congenital renal artery dysplasia is possible, when one or two arteries are narrowed from birth.
Renal arterial hypertension
Kidney diseases such as pyelonephritis, glomerulonephritis, and renal amyloidosis also lead to renal hypertension. The course of such arterial hypertension largely depends on the underlying disease, the speed and degree of blockage of the renal artery. Patients with renovascular arterial hypertension often feel well even with very high blood pressure numbers and do not lose their ability to work.
Renal hypertension usually responds poorly to antihypertensive drugs. During examination, patients may complain of lower back pain, after which an increase in blood pressure occurs. Sometimes a murmur is heard over the renal artery when listening to the abdomen. The x-ray may show different sizes of the kidneys. With excretory and isotope renography, the excretory function of one of the kidneys is reduced. Reliable evidence of the existence of renovascular hypertension in a patient is obtained from aortography and renal angiography (examination of the aorta and renal arteries using contrast agents). Treatment of renal arterial hypertension consists of treating the underlying disease.
Endocrine arterial hypertension
Endocrine arterial hypertension develops in diseases of the endocrine system: pheochromocytoma, primary hyperaldesteronism, Itsenko-Cushing syndrome, hyperparathyroidism (increased production of parathyroid hormones), hyperthyroidism.
Hemodynamic arterial hypertension.
Hemodynamic (mechanical) arterial hypertension occurs with coarctation of the aorta, aortic valve insufficiency, unclosed ductus arteriosus, and in the late stages of heart failure. Most often, hemodynamic arterial hypertension occurs with coarctation of the aorta, a congenital narrowing of the aorta. At the same time, in the vessels extending from the aorta above the site of narrowing, blood pressure is sharply increased, and in the vessels extending below the site of narrowing it is reduced.
A large difference between blood pressure in the upper and lower extremities is important for diagnosis. The diagnosis is finally established by contrast examination of the aorta. Treatment for high degrees of aortic stenosis is surgical.
Neurogenic arterial hypertension
Neurogenic arterial hypertension occurs in diseases of the nervous system. Brain tumors, strokes, injuries and increased intracranial pressure lead to increased blood pressure.
Drug-induced arterial hypertension
Drug-induced hypertension occurs when taking certain medications. These may be oral contraceptives, non-steroidal anti-inflammatory drugs, ephedrine, nervous system stimulants.
Risk factors for developing essential hypertension
Essential hypertension is the most common type of hypertension, although its cause is not always identified. However, in people with this type of hypertension, some characteristic relationships, so-called risk factors, have been identified.
Excess salt in food
Currently, scientists have reliably established that there is a close connection between the level of blood pressure and the amount of salt consumed daily by a person. Essential hypertension develops only in groups with high salt intake, more than 5.8 g per day.
In fact, in some cases, excessive salt intake may be an important risk factor. For example, excessive salt intake may increase the risk of hypertension in the elderly, Africans, obese people, genetic predisposition and kidney failure.
Sodium plays an important role in hypertension. About a third of cases of essential hypertension are associated with increased sodium intake. This is due to the fact that sodium is able to retain water in the body. Excess fluid in the bloodstream leads to increased blood pressure.
Heredity
The genetic factor is considered to be the main factor in the development of essential hypertension, although scientists have not yet discovered the genes responsible for the occurrence of this disease. Scientists are currently investigating genetic factors that affect the renin-angiotensin system, the same one that is involved in the synthesis of renin, a biologically active substance that increases blood pressure. It is located in the kidneys.
Approximately 30% of cases of essential hypertension are associated with genetic factors. If there are first-degree relatives (parents, grandparents, siblings), then the development of arterial hypertension is highly likely. The risk increases even more if two or more relatives have high blood pressure. Very rarely, a genetic disease of the adrenal glands can lead to hypertension.
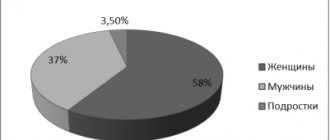
Floor
Men are more predisposed to developing arterial hypertension, especially at the age of 35-55 years. However, after menopause, the risk increases significantly in women. The risk of developing hypertension increases in women during menopause. This is due to a hormonal imbalance in the body during this period and an exacerbation of nervous and emotional reactions. According to research, hypertension develops in 60% of cases in women during menopause. In the remaining 40%, blood pressure is also persistently elevated during menopause, but these changes disappear when the difficult time for women is left behind.
Age
This is also a fairly common risk factor. With age, there is an increase in the number of collagen fibers in the walls of blood vessels. As a result, the wall of the arteries thickens, they lose their elasticity, and the diameter of their lumen decreases.
High blood pressure most often develops in people over 35 years of age, and the older the person, the higher their blood pressure numbers usually are. In men aged 20-29 years, hypertension occurs in 9.4% of cases, and in men aged 40-49 years - already in 35% of cases. When they reach 60-69 years of age, this figure increases to 50%.
It should be taken into account that under the age of 40, men suffer from hypertension much more often than women. After 40 years, the ratio changes in the other direction. Although hypertension is called “the disease of the autumn of a person’s life,” today hypertension has become much younger: more and more often people who are not yet old are suffering from it.
Arterial pathology
In a large number of patients with essential hypertension: there is an increase in resistance (that is, loss of elasticity) of the smallest arteries - arterioles. The arterioles then become capillaries. Loss of elasticity of arterioles leads to increased blood pressure. However, the reason for this change in arterioles is unknown. It has been noted that such changes are typical for individuals with essential hypertension associated with genetic factors, physical inactivity, excessive salt intake and aging.
Renin
Renin is a biologically active substance produced by the juxtaglomerular apparatus of the kidneys. Its effect is associated with an increase in arterial tone, which causes an increase in blood pressure. Essential hypertension can be either high or low renin. For example, African Americans have low renin levels in essential hypertension, so diuretics are more effective in treating hypertension.
Stress and mental strain
Stress is understood as the presence of changes that occur in the body in response to extremely strong irritation. Stress is the body's response to strong environmental factors. Under stress, those parts of the central nervous system that ensure its interaction with the environment are included in the process. But most often, a disorder of the functions of the central nervous system develops as a result of prolonged mental stress, which also occurs in unfavorable conditions. With frequent mental trauma or negative stimuli, the stress hormone adrenaline causes the heart to beat faster, pumping a larger volume of blood per unit of time, as a result of which the pressure increases. If stress continues for a long time, then the constant load wears out the blood vessels, and the increase in blood pressure becomes chronic.
Smoking
The fact that smoking can cause the development of many diseases is so obvious that it does not require detailed consideration. Nicotine primarily affects the heart and blood vessels.
Obesity
A very common risk factor. Overweight people have higher blood pressure than thin people. Obese people are 5 times more likely to develop hypertension compared to those who are of normal weight. More than 85% of patients with arterial hypertension have a body mass index greater than > 25 kg/m2.
Diabetes
It has been established that diabetes mellitus is a reliable and significant risk factor for the development of atherosclerosis, hypertension and coronary heart disease.
Insulin is a hormone produced by the cells of the islets of Langerhans in the pancreas. It regulates blood glucose levels and promotes its passage into cells. In addition, this hormone has some vasodilating properties. Normally, insulin can stimulate sympathetic activity without causing an increase in blood pressure. However, in more severe cases, such as diabetes, stimulatory sympathetic activity may exceed the vasodilatory effect of insulin.
Snore
It has been noted that snoring may also be a risk for essential hypertension.
How to determine the severity of hypertension?
The severity of essential hypertension is determined by the degree of increase in blood pressure, target organ damage, and determination of the risk of cardiovascular complications.
Degrees of arterial hypertension
| Degree | I | II | III |
| Systolic blood pressure level, mm Hg. Art. | 140-159 | 160-179 | >180 |
| Diastolic blood pressure level, mm Hg. st | 90-99 | 100-109 | >110 |
If the SBP or DBP value falls into different categories, then the higher category is set.
The degree of hypertension is established in cases of newly diagnosed hypertension and in patients not receiving antihypertensive drugs. When determining risk, many factors are taken into account: gender, age, cholesterol levels in the blood, obesity, the presence of diseases with arterial hypertension in relatives, smoking, sedentary lifestyle, target organ damage.
Heart
Since the load on the heart muscle increases during arterial hypertension, compensatory hypertrophy (increase) in the thickness of the heart muscle of the left ventricle occurs. Left ventricular hypertrophy is considered a more important risk factor than diabetes, high blood cholesterol and smoking. In conditions of hypertrophy, the heart needs increased blood supply, and the reserve in arterial hypertension is reduced. Therefore, patients with hypertrophy of the wall of the left ventricle of the heart are more likely to develop myocardial infarction, heart failure, rhythm disturbances, or sudden coronary death.
Brain
Already in the early stages of arterial hypertension, blood supply to the brain may decrease. Headache, dizziness, decreased performance, and noise in the head appear. In the deep parts of the brain, with long-term arterial hypertension, small infarctions (lacunar) occur; due to impaired blood supply, the brain mass may decrease. This is manifested by intellectual decline, memory impairment, and in advanced cases, dementia (dementia). Kidneys There is a gradual sclerosis of the vessels and tissues of the kidneys. Their excretory function is impaired. The amount of urea metabolic products in the blood increases, and protein appears in the urine. Ultimately, chronic renal failure is possible. In arterial hypertension, almost all vessels are also affected. Depending on the presence of these risk factors, there are 1, 2, 3 or 4 degrees:
• Risk grade 1 (low risk) means that the patient has less than a 15% chance of having a cardiovascular event over the next 10 years.
• Risk level 2 (medium risk) assumes that the probability of cardiovascular complications in this patient is 15%-20% over the next 10 years
• Risk grade 3 (high risk) assumes that the likelihood of cardiovascular complications in this patient is 20-30% over the next 10 years
• Risk level 4 (very high risk) implies a probability of cardiovascular complications of more than 30% over the next 10 years.
Main symptoms of hypertension
Arterial hypertension often does not manifest itself in any way, which is why this disease has been called the “silent killer.” This is due to the fact that very often a person does not even suspect that he has high blood pressure, and only learns about it when complications occur, often fatal, such as a stroke or myocardial infarction.
Such asymptomatic manifestations of hypertension can last up to several years or even decades.
In some cases, manifestations of arterial hypertension include headaches, dizziness, shortness of breath and blurred vision.
It should be noted that the presence of symptoms of arterial hypertension is a reliable sign in comparison with its asymptomatic course, since the patient consults a doctor earlier, learns about his disease and begins treatment.
Headache. Therefore, it is not for nothing that doctors recommend checking your blood pressure when you have headaches; this diagnostic method is very simple, but at the same time informative.
Headache with increased blood pressure is mainly associated with vasoconstriction of the soft tissues of the head. The most characteristic symptom of arterial hypertension is a headache in the back of the head, as well as in the temples with a sensation of beating in them.
In addition, tinnitus may also be felt, which is associated with narrowing of the vessels of the hearing aid.
Double vision and blurred vision, such as pins and needles, are usually associated with vasoconstriction of the optic nerve, as well as the retina. This can sometimes even lead to temporary blindness. Vasoconstriction and impaired blood flow cause dysfunction of the retina with high blood pressure.
Nausea and vomiting during a hypertensive crisis are associated with increased intracranial pressure.
Shortness of breath may indicate ischemic events in the heart when there is a disturbance in blood flow in the coronary arteries.
In some cases, with arterial hypertension, a hypertensive crisis (or, as they say, hypertensive crisis) may occur. This is a condition in which there is a sharp increase in blood pressure, most often in combination with neurological manifestations in the form of severe headache, dizziness, double vision.
In addition, during a crisis, nausea and even vomiting may occur. Pain in the chest may also be observed, which is associated with ischemic phenomena in the coronary arteries (remember that when blood pressure increases, the arteries narrow).
The appearance of such a patient may be characteristic, with redness of the skin, and emotional agitation is often observed.
Methods for diagnosing hypertension
Diagnostic methods that allow you to determine the presence of arterial hypertension in a person are:
Blood pressure is measured using a special device - a tonometer, which is a combination of a sphygmomanometer and a phonendoscope.
Before measuring blood pressure (BP), you should not smoke or drink tea or coffee for 30 minutes, and you must rest for 5 minutes. The room should be quiet and warm.
The hand selected for measuring blood pressure must be relaxed and freed from clothing. This arm should be free of arteriovenous fistulas for dialysis, brachial artery incision scars, and lymphedema that may result from axillary lymph node removal or radiation therapy.
If you have not yet felt the pulse on the radial artery, then do so to make sure that it is not changed. Position your arm so that the brachial artery (in the elbow area) is at the level of the heart (fourth intercostal space at the edge of the sternum).
Position the cuff bladder over the brachial artery. The lower part of the cuff should be located 2.5 cm above the elbow. Attach the cuff so that it fits snugly around your shoulder. The arm must be slightly bent at the elbow joint.
To determine how high to raise the cuff pressure, first assess your systolic blood pressure. While monitoring the radial pulse with one finger, quickly inflate the cuff until the radial pulse disappears.
Note the pressure gauge readings and add another 30 mmHg. This method is used to ensure that too high pressure in the cuff during further inflation does not cause discomfort in the patient. This also avoids the error caused by the appearance of an auscultatory gap - a silent interval between systolic and diastolic blood pressure.
Quickly release all the air from the cuff and wait 15-30 seconds.
Place the stethoscope over the brachial artery. Quickly inflate the cuff to the previously determined level, and then slowly deflate the air at a rate of approximately 2-3 mmHg. in 1 second. Note the level at which you heard the sound of at least two consecutive contractions. This value corresponds to systolic blood pressure.
Continue decreasing the pressure in the cuff until the sound fades and disappears. To make sure that the sounds have really disappeared, continue listening until the pressure drops another 10-20 mmHg.
Then quickly release all the air from the cuff until the pressure drops to zero. The vanishing point, which is just a few millimeters of mercury below the fading point, provides the most accurate estimate of diastolic blood pressure in adults.
For some people, the muting point and the vanishing point are quite far apart. If the difference is more than 10 mmHg. Art., write down both values (for example, 150/80/68 mmHg).
Round systolic and diastolic pressure values within 2 mmHg. Wait 2 minutes. and then repeat.
Calculate the average. If the first two readings from the device differ by more than 5 mmHg, you need to measure your blood pressure again.
Avoid inflating the cuff with slow, repetitive movements, as the resulting venous congestion may cause incorrect readings.
It is worth noting that in a family where there is a patient with arterial hypertension, it is advisable to always have a device for measuring blood pressure; it is necessary that one of the relatives knows how to use it.
The patient himself can also measure his own blood pressure. In addition, there are currently special electronic devices on the market that measure blood pressure, pulse rate, and also allow you to enter blood pressure readings into the device’s memory.
Normal blood pressure limits for an adult are 110-139/70-89 mmHg.
Diagnosis of arterial hypertension also involves interviewing the patient with a doctor. The doctor asks the patient what diseases he previously suffered from or is currently suffering from.
An assessment of risk factors is carried out (smoking, high cholesterol, diabetes mellitus), as well as hereditary history, i.e., whether the patient’s parents, grandparents and other close relatives suffered from arterial hypertension.
A physical examination of the patient includes, first of all, examination of the heart using a phonendoscope. This method allows you to detect the presence of heart murmurs, changes in characteristic tones (increase or, conversely, weakening), as well as the appearance of uncharacteristic sounds. These data, first of all, indicate changes occurring in the heart tissue due to increased blood pressure, as well as the presence of defects.
An electrocardiogram (ECG) is a method that allows you to record changes in the electrical potentials of the heart over time on a special tape. This is an indispensable method for diagnosing, first of all, various heart rhythm disorders. In addition, the ECG allows us to determine the so-called hypertrophy of the left ventricular wall, which is characteristic of arterial hypertension.
Echocardiography (ultrasound examination of the heart) - allows you to determine the presence of defects in the structure of the heart, changes in the thickness of its walls and the condition of the valves.
Arteriography , including aortography, is an x-ray method for studying the condition of arterial walls and their lumen. This method allows you to detect the presence of atheromatous plaques in the wall of the coronary arteries (coronary angiography), the presence of coarctation of the aorta (congenital narrowing of the aorta in a certain area), etc.
Dopplerography is an ultrasound method for diagnosing the state of blood flow in vessels, both in arteries and veins. In case of arterial hypertension, first of all, the doctor is interested in the condition of the carotid arteries and cerebral arteries. Ultrasound is used for this widespread purpose, since it is absolutely safe to use and is not characterized by complications.
Biochemical blood tests are also used in the diagnosis of arterial hypertension. First of all, the level of cholesterol, triglycerides and low- and very low-density lipoproteins is determined, as they are an indicator of susceptibility to atherosclerosis. In addition, blood glucose levels are determined.
Study of the condition of the kidneys , for which methods such as a general urine test, a biochemical blood test (for creatinine and urea levels), as well as ultrasound of the kidneys and its vessels are used. Ultrasound of the thyroid gland and blood test for thyroid hormones. These research methods help to identify the role of the thyroid gland in the occurrence of high blood pressure.
It is possible that the list of studies offered to you will be different. This is natural. Your doctor will prescribe the necessary examination based on the characteristics of your body and the course of your arterial hypertension.
Complications of renovascular hypertension
Renovascular hypertension leads to both complications characteristic of arterial hypertension and specific problems associated with poor blood flow in the renal arteries. If blood pressure is poorly controlled, the following complications may develop:
- Aortic aneurysm
- Myocardial infarction
- Heart failure
- Chronic kidney disease
- Stroke
- Vision problems (retinopathy)
- Poor blood supply to the legs - critical ischemia.
Types of pathology
The nature of symptomatic hypertension developing against the background of renal diseases can be of two types: parenchymal and renovascular.
The first type is noted when the renal parenchyma is damaged. The parenchyma of an organ is the tissue that fills it. The cells of the kidney tissue are represented by the medulla and cortex, located in the capsule; they are surrounded on all sides by intertwined capillaries. The parenchyma is responsible for performing the main function - removing urine from the body, and also cleanses the blood of toxic substances.
When inflammation of the renal tissue occurs, diseases such as chronic pyelonephritis, kidney stones, tuberculosis, the formation of renal cysts, hydronephrosis, and degenerative changes caused by organ injury are diagnosed. The development of hypertension is noted at the stage of an already formed chronic process - renal failure. Such problems occur more often in young people. Increased pressure is malignant and can lead to disruption of brain and heart functions.
Renal renal hypertension is the result of damage to the walls of the renal vessels, which narrow and reduce the passage for blood flow. This happens for various reasons, the most common of which is the occurrence of blood clots or atherosclerotic plaques that block the lumen in the artery.
Forecast
The prognosis in patients with renovascular hypertension is difficult to determine, and it depends on the degree of atherosclerotic lesions in other areas, individual sensitivity to antihypertensive therapy, and the effectiveness of surgical intervention. In patients with arterial hypertension, the presence of renal artery atherosclerosis is a factor in a significant increase in mortality compared with the general population. As kidney failure develops, the risk of death increases even more.
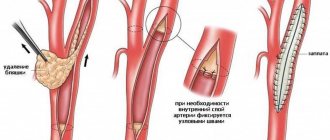
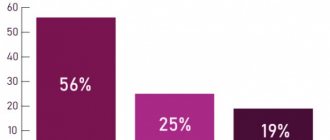
Surgery of the renal arteries (angioplasty and stenting) provides a very good prognosis for patients with renal vasoretension. In more than 70% of patients, blood pressure is normalized, without the need to take medications. In another 25%, the level of hypertension decreases, but still requires some drug therapy. Thus, in less than 5% of patients, restoration of blood flow through the renal artery is ineffective.
4.Treatment
As statistical analysis of the data accumulated in the world shows, conservative methods (medication, nutrition, etc.) are much less effective than active therapy and can only be used as auxiliary, preoperative, supportive measures, as well as palliative treatment in the presence of contraindications to surgical intervention. Surgical correction of renal arterial hypertension in most cases brings a lasting and pronounced positive result and significantly increases the life expectancy of such patients. Abdominal, endoscopic or percutaneous surgery is performed (depending on the clinical characteristics of a particular case) to restore the patency of stenotic arteries, eliminate congenital defects, or completely remove the affected and non-functioning kidney, which in some cases is the only effective answer. Approximately one third of patients may no longer take maintenance antihypertensive drugs.
Palliative antihypertensive therapy as an alternative to surgery, however, is also characterized by fairly high efficiency (although we can only talk about constant drug control of blood pressure) and allows one to normalize blood pressure to one degree or another in more than 90% of cases.