The use of angiotensin receptor blockers in the treatment of arterial hypertension
What is the advantage of angiotensin receptor blockers over other classes of antihypertensive drugs, in particular over ACE inhibitors? What is the comparative effectiveness of various angiotensin receptor blockers?
Based on a representative sample (1993), it can be stated that the prevalence of arterial hypertension (AH) in Russia is 39.2% among men and 41.1% among women. At the same time, only 58.9% of women and 37.1% of men know about the presence of the disease; 46.7% and 21.6% receive treatment (including effective treatment - 17.5% and 5.7%), respectively (first report experts of the Scientific Society for the Study of Arterial Hypertension, the All-Russian Scientific Society of Cardiologists, the Interdepartmental Council on Cardiovascular Diseases, 2000). The management of patients with hypertension is currently regulated by the recommendations of experts from the World Health Organization (WHO) and the International Society of Arterial Hypertension (ISH) (WHO-SOG recommendations, 1999) and the National Guidelines for the diagnosis and treatment of arterial hypertension developed on this basis (All-Russian Scientific Society of Cardiology, Arterial Hypertension Section, 2001). According to these recommendations, the goal of hypertension treatment is to reduce the overall risk of cardiovascular morbidity and mortality, which involves reducing blood pressure to the target level (less than 140/90 mm Hg), as well as correcting all identified risk factors (for example, adequate treatment of hypercholesterolemia , diabetes mellitus). Since course treatment of hypertension is ineffective (in most cases, hypertension cannot be cured), the patient must receive individually selected antihypertensive therapy constantly.
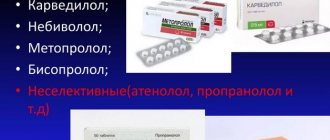
For long-term treatment of hypertension, β-blockers, diuretics, angiotensin-converting enzyme (ACE) inhibitors, angiotensin receptor blockers, calcium antagonists, and α-blockers are currently used. As is known, in the pathogenesis of arterial hypertension, angiotensin II plays a crucial role, causing vasoconstriction, stimulation of aldosterone synthesis and its release, sodium reabsorption in the kidneys, cardiac muscle growth, proliferation of smooth muscle cells of blood vessels, increased peripheral noradrenergic activity and a number of other effects. Therefore, the most promising in the drug correction of hypertension are currently considered to be angiotensin-converting enzyme (ACE) inhibitors, which prevent the transition of angiotensin I to angiotensin II, and angiotensin receptor blockers. Widely used ACE inhibitors, although highly effective, have a number of side effects (including cough, angioedema) due to their effect on the metabolism of bradykinin and substance P [4].
Angiotensin receptor blockers have a number of advantages over ACE inhibitors - they more specifically and effectively suppress the cardiovascular effects of activation of the renin-angiotensin system. Currently, this “youngest” group of antihypertensive drugs (the first of them is losartan, synthesized in 1988) is represented by a number of drugs that differ slightly from each other in their mechanism of action and pharmacokinetic properties.
Based on their chemical structure, they distinguish between biphenyl tetrazole derivatives (losartan, irbesartan, candesartan), non-biphenyl non-tetrazole compounds (eprosartan, telmisartan) and non-heterocyclic compounds (valsartan); depending on the presence of the active metabolite - prodrugs (losartan, candesartan) and active medicinal substances (valsartan, irbesartan, telmisartan, eprosartan); depending on the type of antagonism with angiotensin II - competitive antagonists (losartan, eprosartan) and non-competitive (valsartan, irbesartan, candesartan, telmisartan). The main characteristics of various angiotensin receptor blockers are given in table. 1.
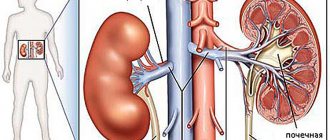
The hypotensive effect of angiotensin receptor blockers is primarily associated with the suppression of the vasoconstrictor effect of angiotensin II, realized through receptors in the walls of blood vessels. In addition, blockade of angiotensin II receptors leads to a decrease in the secretion of aldosterone, a decrease in the reabsorption of sodium and water in the proximal segment of the renal tubules.
Stimulation of type 2 angiotensin receptors may play a certain role in the hypotensive effect when the level of angiotensin II is elevated (due to blockade of type 1 receptors). It is assumed that stimulation of angiotensin II type II receptors can lead to vasodilation and suppression of proliferative processes.
At the same time, electrophysiological studies in animals have shown that angiotensin II, by activating presynaptic angiotensin receptors of noradrenergic neurons of the sympathetic nervous system, increases the release of norepinephrine. When studying the effect of various angiotensin receptor antagonists (valsartan, irbesartan, losartan, eprosartan) on the sympathetic release stimulated in decerebrate normotensive rats by spinal cord irritation, an inhibitory effect was noted only for eprosartan [6]. Thus, in clinical practice, eprosartan (teveten) is the only drug in its group that can block both presynaptic receptors and angiotensin receptors in blood vessels in therapeutic doses.
Angiotensin receptor blockers, used in therapeutic doses, on average reduce systolic blood pressure by 10-20 mmHg. Art. and diastolic - by 10-15 mm Hg. Art., as shown in a large number of studies. The maximum reduction in blood pressure is achieved in most patients after 3-4 weeks of treatment.
As an example, here are several clinical studies on the effectiveness of eprosartan. An 8-week, double-blind, placebo-controlled, randomized, clinical (243 patients with mild to moderate hypertension) study of eprosartan (teveten at a dose of 600 mg once daily) showed that the drug lowered blood pressure significantly more effectively than placebo [3 ]: in the eprosartan group, systolic blood pressure decreased by 6 mmHg. Art., diastolic - by 7.5 mm Hg. Art.; the difference compared to the results in the placebo group was statistically significant. Therapy was considered effective if diastolic pressure in the sitting position decreased to 90 mmHg. Art. or the decrease in diastolic blood pressure from the initial level was 10 mm Hg. Art. and more. In the eprosartan group, therapy was effective in 42% of patients, in the placebo group - in 21%.
The relationship between the dose of eprosartan and the level of blood pressure reduction was assessed in a multicenter, double-blind, parallel, placebo-controlled study that included 364 patients with a baseline diastolic blood pressure of 95-114 mm Hg. Art. The effectiveness of eprosartan therapy was assessed at doses of 400, 600, 800, 1200 mg once a day compared with placebo; the duration of treatment was 8 weeks. According to the results obtained, the optimal initial dose of the drug was 600 mg per day [10].
In a 13-week, double-blind, placebo-controlled, parallel-group study [4], 243 patients received eprosartan at a daily dose of 400–800 mg once or twice daily. The dose of the drug was adjusted during the first 9 weeks until the optimal hypotensive effect was achieved, after which drug therapy at an effective dose continued for another 4 weeks. The hypotensive effect of eprosartan was once again confirmed (diastolic blood pressure decreased in the treatment group by an average of 9 mm Hg versus 4 mm Hg in the placebo group), and the therapeutic effect was the same when taking the drug once or twice a day. Therapy with eprosartan (once daily) was effective in 46.8% of cases.
A number of studies have shown that angiotensin receptor blockers are at least as effective as ACE inhibitors (Table 2). For example, in a 26-week, double-blind, clinical (528 patients aged 21-78 years with mild to moderate hypertension) study [2], therapy with eprosartan at a dose of 400-600 mg per day was more effective than treatment with enalapril in dose 5-20 mg per day. There were more patients in whom antihypertensive therapy was found to be effective in the eprosartan group (81.7%) compared to the enalapril group (73.4%). When analyzing the results obtained, it turned out that in the subgroup of elderly patients, the frequency of cases of “response to treatment” was the same as in young patients [1]. Similar results were obtained in another study devoted to a comparative assessment of the hypotensive effects of eprosartan and enalapril in mild to moderate arterial hypertension [7].
The comparative effectiveness of eprosartan (400-800 mg per day in two divided doses) and enalapril (10-40 mg per day in one dose) in severe arterial hypertension was studied in a 10-week double-blind study involving 118 patients (78% of them in over 65 years of age) [8]. The dose was titrated every two weeks; If necessary, hydrochlorothiazide (hypothiazide 25 mg per day) was added to therapy. Therapy with eprosartan led to a more significant reduction in systolic and diastolic blood pressure compared with enalapril; additional prescription of diuretics was required in both groups in almost the same number of patients (39% of patients in the eprosartan group, 37% in the enalapril group). Thus, compared with enalapril, eprosartan is more effective in reducing elevated systolic blood pressure in severe arterial hypertension.
A number of studies have assessed the effectiveness of various angiotensin receptor blockers. For example, an 8-week study [5] included 567 patients with mild to moderate hypertension (Table 3). Therapy with irbesartan at a dose of 300 mg per day was slightly more effective than treatment with losartan at a dose of 100 mg per day; the proportion of patients who responded to treatment was 52% and 42%, respectively. In a 4-week, double-blind, randomized, clinical trial involving 60 patients, eprosartan (600 mg once daily) was found to be more effective than losartan (50 mg once daily). Patients in whom therapy was considered effective were 73% in the eprosartan group and 53% in the losartan group [9].
The most important requirement for modern antihypertensive drugs is a high duration of exposure, allowing control of blood pressure for 24 hours. To assess the severity and duration of the antihypertensive effect of long-acting drugs, the US Food and Drug Administration (FDA) proposed in 1988-1990 . use the “trough:peak” (T/P) coefficient, that is, the ratio between the smallest decrease in systolic or diastolic pressure at the end of the interdose interval and its maximum decrease at the height of the drug’s effect. Antihypertensive therapy seems optimal, in which there are no significant fluctuations in blood pressure during the day, that is, this coefficient should tend to unity, or 100%. According to FDA recommendations, the final:peak ratio should be at least 50%; this means that modern antihypertensive drugs should provide a reduction in blood pressure 24 hours after administration by at least 50% of the reduction in values during the period of maximum hypotensive effect. This allows for effective blood pressure control between doses of the drug; low fluctuations in blood pressure help reduce damage to the vascular wall, and consequently, the frequency of cardiovascular complications of arterial hypertension decreases.
The T/P ratio values for various angiotensin receptor blockers are presented in table. 4.
Using ambulatory blood pressure monitoring, it has been shown that a single dose of angiotensin receptor blockers provides control of blood pressure levels throughout the day, including in the morning, when the risk of developing vascular accidents (myocardial infarction and stroke) is especially high; Only losartan in some cases has to be used twice a day. The highest values of the T/P ratio (i.e., the longest duration of effective antihypertensive action) were found when using eprosartan, irbesartan and candesartan.
The high effectiveness of angiotensin receptor blockers is combined with good tolerability. According to data obtained from placebo-controlled clinical trials, the frequency of side effects during therapy with drugs of this group does not differ from this indicator in the placebo group. In particular, the incidence of side effects during therapy with losartan is 15.3% versus 15.5% in the placebo group, and during therapy with valsartan - 15.7% versus 14.5%; the frequency of side effects during therapy with eprosartan is given in table. 5. It is very important that drugs in this group, unlike ACE inhibitors, do not cause or worsen cough. Thus, angiotensin receptor blockers are quite safe; Contraindications to their use are only pregnancy, hyperkalemia and bilateral renal artery stenosis.
According to the National Guidelines for the Diagnosis and Treatment of Arterial Hypertension (2001), the absolute indication for the use of angiotensin receptor blockers is intolerance to ACE inhibitors (cough when using them), and the relative indication is congestive heart failure. The last recommendation is due to the fact that, as shown by Pitt B. et al. (1997), losartan can increase life expectancy in patients with chronic heart failure.
It should be noted, however, that inhibition of both the sympathoadrenal and angiotensin-aldosterone systems by eprosartan leads to a significant decrease in systolic blood pressure, therefore the use of this drug is promising for isolated systolic hypertension, arterial hypertension after a stroke, obesity, stress-induced, metabolic, alcoholic hypertension ( Kobalava Zh. D., Moiseev V. S., 2000).
Literature
- Argenziano L., Trimarco B. Effect of eprosartan and enalapril in the treatment of elderly hypertensive patients: subgroup analysis of a 26-week, double-blind, multicentre study. Eprosartan Multinational Study Group. Curr Med Res Opin 1999; 15(1):9-14.
- Gavras I., Gavras H. Effects of eprosartan versus enalapril in hypertensive patients on the renin-angiotensin-aldosterone system and safety parameters: results from a 26-week, double-blind, multicentre study. Eprosartan Multinational Study Group. Curr Med Res Opin 1999; 15(1):15-24.
- Gradman A.H., Gray J., Maggiacomo F., Punzi H., White WB Assessment of once-daily eprosartan, an angiotensin II antagonist, in patients with systemic hypertension. Eprosartan Study Group. Clin Ther, 1999; 21(3):442-453.
- Hedner T., Himmelmann A., for the Eprosartan Multinational Study Group. The efficacy and tolerance of once and twice daily doses of eprosartan in essential hypertension. J Hypertens, 1999; 17:129-136.
- Kassler-Taub K., Littlejohn T., Elliot W. et al., for the Irbesartan Study Investigators. Comparative efficacy of two angiotensin II receptor antagonists, irbesartan and losartan, in mild to moderate hypertension. Am J Hypertens. 1998; 11:445-53.
- Ohlstein EH, Brooks DP, Feuerstein GZ, Ruffolo RR Inhibition of sympathetic outflow by the angiotensin II receptor antagonist, eprosartan, but not by losartan, valsartan or irbesartan: relationship to differences in prejunctional angiotensin II receptor blockade. Pharmacology, 1997; 55(5):244-51.
- Oparil S. Eprosartan versus enalapril in hypertensive patients with angiotensin-converting enzyme inhibitor cough. Curr Ther Res, 1999; 60(1):1-14.
- Ponticelli C., for the Eprosartan Study Group. Comparison of the efficacy of eprosartan and enalapril in patients with severe hypertension. Am J Hypertens, 1997; 10:128A.
- Puig JG, Mateos F., Buno A., Ortega R., Rodriguez F., Dal-Re. R. Effect of eprosartan and losartan on uric acid metabolism in patients with essential hypertension. J Hypertens, 1999; 17(7):1033-1039.
- Weber M. Clinical efficacy of eprosartan. Pharmacotherapy. 1999; 19(4, part 2):95–101.
- Zanchetti A., Omboni S., Di Biago C. Candesartan cilexetil and enalapril are of equivalent efficacy in patients with mild to moderate hypertension. J Hum Hypertens 1997; 11 (suppl 2):57-9.
Features of the impact of the funds
The effect of drugs that belong to the group of ACE inhibitors is based on the fact that they slow down the body's production of angiotensin II. This hormone causes blood vessels to constrict, which leads to increased blood pressure. Under the influence of active substances in the composition of the drugs, the vessels remain dilated, which reduces the load on the heart muscle and lowers blood pressure.
Most ACE inhibitor drugs are intended for oral use. But if intensive therapy is necessary in severe cases, drugs in this group can be administered intravenously.
Indications for prescribing ACE inhibitors are varied. In addition to the treatment of arterial hypertension of any origin, drugs are prescribed for the following pathologies:
- Myocardial infarction in the acute phase. When used, it is possible to reduce the rate of tissue destruction.
- Coronary insufficiency. With the help of funds it is possible to reduce the risk of relapse.
- Ischemic stroke. During an emergency, blood pressure always increases and needs to be normalized.
ATP inhibitors are prescribed for kidney problems and to reduce certain symptoms of diabetes and migraines. When treating arterial hypertension, the doctor may prescribe an ACE inhibitor in combination with other drugs that lower blood pressure in order to obtain quick results.
There are many contraindications for the use of medications whose main purpose is to lower blood pressure. Therefore, they should be prescribed by a doctor taking into account the patient’s condition. It is not recommended to use ATP inhibitors during pregnancy and lactation.
2nd generation drugs
Second-generation ACE inhibitors are used very often today in the treatment of arterial hypertension. This is due to the combination of high efficiency and safety of medications. The main difference from first-generation drugs is that the effect after administration occurs no earlier than 20 minutes later. But at the same time it persists for a longer time - up to 5-8 hours.
Enalapril is often prescribed to treat elderly patients. The drug has the additional ability to prevent the formation of blood clots and remove cholesterol. Other representatives of the group of second-generation ACE inhibitors:
- Perindopril. An effective and safe drug for use in the complex treatment of hypertension, as well as the prevention of heart attack and stroke.
- Lisinopril. The drug is prescribed to patients without kidney pathologies, since it is completely excreted in the urine. The active substance does not accumulate in adipose tissue, so the medicine is prescribed when high blood pressure occurs due to excess weight.
- Ramipril. The medicine is considered effective only in the treatment of arterial hypertension at the initial stage of development. It is often prescribed for long-term use.
1st generation drugs
The first generation ACE inhibitors were developed in the mid-70s of the last century. Despite their high effectiveness, they are characterized by a large number of side effects. Therefore, it is very important not to deviate from the dosage recommended by the doctor. Using ACE inhibitors on your own, the list of drugs for which is not very large, is strictly prohibited.
Representatives of the first group are the following drugs:
- Captopril. The product guarantees a rapid reduction in blood pressure and is suitable for use in emergency situations. To avoid serious side effects, it can only be used in small doses. This is the only drug that is used to relieve hypertensive crisis.
- Benazepril. The medicine has a milder effect and can be used to correct blood pressure in moderate stage hypertension, as well as in congestive heart failure.
- Zofenopril. The most gentle drug with minimal side effects and antioxidant effect. But at the same time, it is indicated for use only in the initial stages of arterial hypertension.