Atherosclerosis: risk factors, prevention
Updated: 12/13/2016, 10:42 Published: 12/13/2016, 10:42
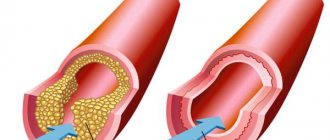
Atherosclerosis is a chronic disease of blood vessels, in which cholesterol and other fats are deposited on the inner wall of the arteries in the form of plaques and plaques, and the walls themselves become denser and lose elasticity . The vessels gradually become hard due to the settling of fats and lime on the walls, lose their elasticity and, as a result, narrow, which, as is known, reduces blood access to the organs. Eventually the vessel may close completely. And when this is accompanied by a blood clotting disorder, there is a tendency to thrombosis and ischemic damage to organs occurs.
Risk factors play a role in the development and progression of atherosclerosis
:modifiable (which can be eliminated or adjusted) and non-modifiable (they cannot be changed).
Modifiable factors include:
1. Lifestyle: physical inactivity, abuse of fatty, cholesterol-rich foods, personality and behavior characteristics - stressful character type, alcohol abuse, smoking.
2. Arterial hypertension, blood pressure 140/90 mm Hg. and higher.
3. Diabetes mellitus, fasting blood glucose level more than 6 mmol/l.
4. Hypercholesterolemia (blood cholesterol level more than 5 mmol/l).
5. Abdominal obesity (waist circumference in men is more than 102 cm and more than 88 cm in women).
Non-modifiable factors include:
1. Age: men over 45 and women over 55 or with early menopause.
2. Male gender (men develop atherosclerosis 10 years earlier than women).
3. A family history of cases of early atherosclerosis. Familial hypercholesterolemia with a genetic basis. Myocardial infarction, stroke, sudden death in close relatives under the age of 55 years for a man and 65 years for a woman.
What is atherosclerosis?
This is one of the most common vascular diseases that affects medium and large arteries. “Bad” cholesterol, or more precisely, low-density lipoproteins, accumulate on the walls of the arteries and form hard structures called atherosclerotic plaques
.
The ABCs of healthy eating
20 simple facts about how to eat right will help you build a balanced diet for health and well-being.
Gradually, plaques narrow the lumen of the arteries and make their walls less elastic, which impedes the flow of blood.
If the coronary (heart) arteries are affected, blood flow to the heart is slowed down or virtually stopped. This causes chest pain - angina
.
If the vessels are tightly clogged, then the lack of nutrition of the heart muscle causes the development of a heart attack - a heart attack
.
Symptoms of atherosclerosis
Vascular changes are often localized in the aorta, cardiac, cerebral, renal arteries and arteries of the extremities, most often the lower ones. The picture of the disease and the patient’s complaints depend on the damage to certain arteries. Thus, atherosclerosis of the coronary arteries (heart vessels) very often manifests itself in the form of angina pectoris and heart attack. At the heart of the pathological process, i.e. disease, there is a violation of the correspondence between the need of the heart for blood supply and its actual implementation. Often, severe forms of aortic atherosclerosis can be asymptomatic. The patient may experience pressing or burning pain behind the sternum, radiating to both arms, neck, back, and upper abdomen. But unlike angina, these pains last a long time, sometimes intensifying and sometimes weakening.
When the renal vessels are damaged, severe arterial hypertension occurs. Atherosclerosis of the cerebral arteries is manifested by decreased performance (especially mental), decreased memory, active attention, and fatigue. Over time, dizziness and insomnia appear, patients become fussy, obsessive, and picky. Their intelligence decreases. A complication of atherosclerosis of the cerebral arteries is a violation of cerebral circulation, hemorrhage (stroke), thrombosis. Atherosclerosis of the arteries of the extremities, most often the lower ones, manifests itself in the calf muscles when walking (“intermittent claudication”). Chilliness and coldness of the extremities appear. Thus, atherosclerosis leads to the development of most modern “diseases of civilization.”
If atherosclerotic changes are suspected, consultation with specialists is indicated:
cardiologist (for coronary heart disease); ophthalmologist (atherosclerosis of the fundus vessels); neurologist (cerebral atherosclerosis); nephrologist (atherosclerosis of the renal arteries); vascular surgeon (atherosclerosis of the vessels of the lower extremities, aorta). To clarify the degree of atherosclerotic lesion, additional instrumental research methods may be prescribed: electrocardiography, angiography, coronary angiography , intravascular ultrasound, duplex and triplex scanning, magnetic resonance imaging and others.
Prevention of atherosclerosis
Anti-atherosclerotic diet. Diet recommendations are given to all patients taking into account cholesterol levels and other risk factors: obesity, arterial hypertension, diabetes mellitus. The diet should be varied, in accordance with the cultural traditions of the patient. The calorie content of the daily diet should be sufficient to achieve and maintain normal weight.
Consumption of total fat should not exceed 30% of the calorie content of the diet. It is recommended to limit the consumption of animal fats (butter, cream, meat, lard), replacing them with vegetable fats. Daily consumption of fresh vegetables and fruits should be at least 500g per day.
It is recommended to consume lean meat and skinless poultry, fermented milk products, low-fat cottage cheese, grain bread, with bran, and foods enriched with unsaturated fatty acids (sea and ocean fish - salmon, mackerel, tuna, etc.). Limit the consumption of table salt to 6g per day, which corresponds to 1 teaspoon. Following a diet can reduce cholesterol levels by up to 10%.
Refusal to drink alcohol.
Health-safe alcohol consumption (no more than 20-30 ml of pure ethanol per day for men and no more than 20 ml per day for women) is permissible only for practically healthy individuals. Drinking 5 servings of alcohol (60g per day) increases the risk of cardiovascular complications by 65%.
Normalization of body weight indicators. Excess body weight and obesity, especially abdominal obesity (waist circumference in men more than 102 cm and more than 88 cm in women), increase the risk of developing cardiovascular diseases. To lose weight, an individual diet is selected taking into account age and concomitant diseases.
Physical activity for atherosclerosis. Increasing physical activity has a positive effect for patients with atherosclerosis. Patients without clinical manifestations of atherosclerosis are advised to exercise for 30 minutes daily. Patients with cardiovascular diseases require a constant regime of dynamic physical activity, taking into account the results of stress tests. Walking, swimming, and dancing of moderate intensity for 60-90 minutes a week are beneficial. Isometric (power) loads are unacceptable. It is recommended to use any opportunity for physical activity: walking, using a car less often.
Atherosclerosis: causes and prevention
What is this - a disease or a norm?
How does atherosclerotic plaque form? Prevention and treatment of atherosclerosis
What is it - a disease or a norm?
Unfortunately, most people do not attach due importance to the symptoms of the onset and development of atherosclerosis, and know little about the causes of its occurrence, measures for prevention and preservation of vascular health.
Atherosclerosis (more precisely, increased cholesterol in the blood) is one of the main risk factors for cardiovascular diseases. The consequences of atherosclerosis account for approximately half of deaths in most developed countries. It doesn’t hurt to remember this every time you want to eat a fried pie, ham or something “fatty”.
In healthy people, blood flows freely through the arteries to all parts of the body, supplying them with oxygen and other nutrients. With atherosclerosis, plaques form on the inner wall of the arteries, which can lead to complete blockage of the vessel.
How does atherosclerotic plaque form?
The word “atherosclerosis” comes from two ancient Greek words: athere – “mush” and sclerosis – “hard”, “dense”. This reflects the stages of development of an atherosclerotic plaque. There are three main stages of atherosclerotic plaque formation (atherogenesis):
- Formation of lipid (fat) spots and streaks (stage of lipoidosis).
- Formation of fibrous plaque (stage of liposclerosis).
- Formation of complicated atherosclerotic plaque.
Formation of lipid spots and streaks
The initial stage is characterized by the appearance of fatty deposits in the form of spots and stripes on the inner vascular wall of the arteries (arterial intima), which is a barrier between the arterial wall and the blood.
Why does fat deposit on blood vessels occur?
Under certain pathological conditions (trauma, some viral diseases, toxic influences, smoking, alcohol abuse and many others), damage to the integrity of the internal vascular wall
, accompanied by an increase in the permeability of this barrier.
Low-density lipoproteins (LDL - the so-called “bad cholesterol”) penetrate into sites of damage to the inner vascular wall of the arteries and undergo oxidation or glycosylation (modification), which further damages the inner layer of vessel cells.
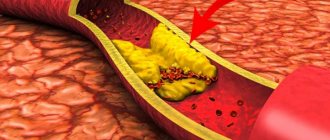
Our immune system does not ignore this pathological process. Trying to fix everything, monocytes (immune cells) penetrate the vascular wall of the arteries, transform into macrophages, which, with the help of so-called sequencer receptors (“scavenger receptors”), absorb modified LDL and accumulate cholesterol. Macrophages overloaded with fats turn into xanthoma (foam) cells. Some xanthoma cells that have absorbed lipoproteins from the intercellular substance leave the artery wall, thereby preventing the accumulation of fats in it. If the entry of lipoproteins (“bad cholesterol”) into the vascular wall prevails over their removal by macrophages (or other routes), fats accumulate, and ultimately an atherosclerotic plaque is formed. In a growing plaque, some xanthoma (foam) cells die and are destroyed. As a result, a cavity is formed in the center of the plaque, filled with rich fatty masses, which is typical for the later stages of the formation of an atherosclerotic plaque.
Formation of fibrous plaques
As the pathological process progresses, young connective tissue grows in areas of fat deposition, which leads to the formation of fibrous plaques, in the center of which a so-called lipid (fat) core is formed. As the connective tissue matures, a connective tissue framework of the atherosclerotic plaque is formed - a “tyre”, which separates the lipid core from the lumen of the vessel. A typical fibrous plaque is formed, protruding into the lumen of the vessel and disrupting the blood flow in it.
The clinical and prognostic significance of a formed atherosclerotic plaque largely depends on the structure of its fibrous cap and the size of the lipid core. In some cases (including in the relatively early stages of plaque formation), its lipid core is well defined, and the connective tissue capsule is relatively thin and can be easily damaged under the influence of high blood pressure, accelerated blood flow in the artery and other factors. These soft and elastic plaques are sometimes called “yellow plaques.” They, as a rule, slightly narrow the lumen of the vessel, but are associated with a high risk of damage and rupture of the fibrous capsule, that is, with the formation of the so-called “complicated” atherosclerotic plaque.
In other cases (usually in later stages), the fibrous cap is well defined, dense and less susceptible to damage and rupture. Such plaques are called “white”. They often protrude significantly into the lumen of the artery and cause a hemodynamically significant narrowing (by 50% or more of the internal diameter of the artery), leading to disruption of the blood supply to the organ supplied by the artery. In some cases, such plaques may be complicated by the occurrence of a mural thrombus.
The first two stages of atherogenesis culminate in the formation of an uncomplicated atherosclerotic plaque. The progression of the atheromatous process leads to the formation of a “complicated” atherosclerotic plaque, resulting in the formation of a wall thrombus, which can lead to a sudden and severe limitation of blood flow in the artery.
Formation of a “complicated” plaque
This stage of atheromatosis is characterized by a significant increase in the lipid core (up to 30% or more of the total volume of the plaque), the occurrence of hemorrhages in the plaque, thinning of its fibrous capsule and destruction of the cap with the formation of cracks, ruptures and atheromatous ulcers.
Particles of collapsing plaque falling into the lumen of the vessels can become a source of embolism - a condition in which the lumens of blood vessels are blocked by an embolus, that is, a particle brought with the bloodstream (a detached blood clot, fat from damaged tissue, etc.). The atheromatous ulcer itself serves as the basis for the formation of blood clots. The final stage of atherosclerosis is atherocalcinosis, the deposition of calcium salts in atherosclerotic masses.
The main consequence of the formation of a “complicated” atherosclerotic plaque is the formation of a parietal thrombus, which suddenly and sharply restricts blood flow in the artery. In most cases, it is during this period that clinical manifestations of exacerbation of the disease occur, corresponding to the localization of the atherosclerotic plaque (unstable angina, myocardial infarction, ischemic stroke, etc.).
Prevention and treatment of atherosclerosis
Atherosclerosis occurs in everyone. The only difference is in the degree and speed of its development, which is largely determined by people’s lifestyle, bad habits, and hereditary factors. This disease develops unnoticed, affecting more and more arteries over the years.
Until recently, atherosclerosis was considered a steadily progressive disease. In recent years, evidence has emerged that the development of atherosclerosis can be slowed or stopped.
This result can be achieved by regularly taking certain medications and changing your lifestyle and behavioral habits.
.
It is necessary to begin measures to prevent atherosclerosis as early as possible, without waiting for clinical manifestations of the disease.
The main recommendation is lifestyle changes. In other words, if there is a high risk of atherosclerosis, it is necessary to start leading a healthy lifestyle, which includes:
- to give up smoking;
- sufficient physical activity;
- normalization of body weight;
- maintaining normal blood pressure;
- change in nutritional pattern. Specific recommendations are displayed in the table: Table 1. Rules for the prevention of atherosclerosis
| AVOID | TRY |
|
|
|
|
|
|
|
|
|
|
For the development of atherosclerosis, the most important factor is elevated cholesterol levels in the blood, so the goal of treating atherosclerosis is to normalize cholesterol levels.
If, as a result of dietary changes (cholesterol-lowering diet) and lifestyle adjustments, it is not possible to achieve the desired cholesterol level, the doctor prescribes medications.
The key to success in the treatment of atherosclerosis is following the doctor’s instructions.
The reward for your efforts to change your lifestyle and take medications prescribed by your doctor is INCREASED HEALTHY LIFESPAN. Share on social media networks
To reduce blood cholesterol levels you need to:
— Reduce daily fat intake to 30% of total calories.
— There are fruits and vegetables. Start every meal with a vegetable salad. Eat foods low in fat. Replace butter with vegetable oil. Try to stew meat and vegetables rather than fry them.
Good to use
Fresh fruits and vegetables, greens, salad, low-fat cottage cheese, low-fat fish, cereals, bran
Should be consumed in moderation
Cereals, potatoes, legumes (peas, soybeans, beans, lentils), fruits and berries pureed with sugar, milk, fermented milk products (kefir, curdled milk, yogurt), low-fat hard cheeses, lean meat, chicken breast, turkey breast, eggs, bread, pasta, unsweetened juices
Should be avoided
Everything fried, lard, butter, margarine, mayonnaise, nuts, seeds, fatty meat, meat salads with mayonnaise, fatty sausages and meat products (bacon, brisket, ham, boiled pork, etc.), fatty fish, caviar, canned fish in oil , sour cream, cream, ice cream, fatty cheeses (more than 30% fat), sugar, candy, chocolate, jam, jam, marmalade, cakes, pastries, pies, sweet juices, cocoa, alcoholic drinks
- Move more. Let physical activity become regular. The more we move, the less cholesterol is deposited in our blood vessels.
- Quit smoking. Components of tobacco smoke increase blood cholesterol levels.
There are other fats that contribute to the development of atherosclerosis. These are triglycerides (TG). The desired blood TG level is less than 150 mg/dL (1.7 mmol/L). Controlling elevated TG levels is another important factor in helping prevent atherosclerosis.
What does it lead to?
An atherosclerotic plaque or part of it can break off and, along with the blood flow, begin traveling through the arteries. Plaques get stuck in smaller vessels, block the movement of blood through them and cause disruption of blood supply
to entire areas of tissue.
If a vessel in a limb becomes clogged, the muscles die due to lack of nutrition and oxygen, and gangrene
.
And if the plaque reaches the arteries of the brain and gets stuck in them, a stroke develops. In some cases, atherosclerotic plaques stretch certain parts of the artery, causing the formation of an aneurysm
- a bulge in the artery wall due to its thinning and stretching.
Symptoms of atherosclerosis are not noticeable until plaque restricts or blocks blood flow in the arteries. The possible onset of an atherosclerotic process is indicated only by an increase in systolic (upper) pressure
.
Depending on the location of the artery, the lack of blood flow can manifest itself in the form of different symptoms
. Starvation of the heart muscle leads to pain in the heart - angina. Lack of blood supply to the brain impairs memory. Clogged blood vessels in the extremities lead to muscle pain, first while walking, and then at rest.