A high pulse with high blood pressure is observed quite often, but the relationship between both indicators in hypertension is not natural. A simultaneous increase in indicators occurs with excessive load on the myocardium, which may indicate the development of complications from the cardiac and vascular systems. The combination of both disorders provokes the occurrence of stroke and heart attack - dangerous pathologies that cause death. To prevent the progression of the disorder and reduce the risk of negative consequences, it is necessary to consult a specialist in a timely manner. What are the causes of rapid heartbeat with elevated blood pressure and how to stabilize the indicators?
The relationship between high heart rate and hypertension
High pulse with high blood pressure is a fairly common phenomenon that often occurs simultaneously. Constantly elevated levels of blood pressure contribute to pumping a large volume of circulating blood, as a result of which the heart muscle is subjected to excessive stress. As a result, myocardial contractile activity increases, provoking the formation of tachycardia. An increased number of heart contractions is characterized by a strong and intense pulse wave with an indicator higher than 90 beats per minute, which indicates a possible disorder if the patient is at rest.
Why is heart rhythm disorder most often recorded in hypertension? Arterial hypertension reflexively provokes the development of tachycardia. Thus, in most hypertensive patients, the first sign of the negative impact of increased blood pressure on the body is a heart rhythm disorder. With hypertension, paroxysmal tachycardia is most often recorded, manifested by a sharp attack of rapid heartbeat up to 120 beats/min, while the rhythm is maintained, since electrical impulses come from one area. Frequent attacks of this form of tachycardia lead to the formation of acute vascular and heart failure. An unfavorable course of hypertension can cause the formation of arrhythmia, which is provoked by a hypertensive attack of the cardiac form, when an increase in blood pressure is combined with acute cardiac left ventricular failure.
Important! The appearance of a rapid pulse in hypertension is a poor diagnostic sign, indicating the transition of the disease to the third stage, when irreversible changes form in the organs.
Why should tachycardia be eliminated?
Rapid heartbeat is a rather dangerous symptom that must be eliminated as soon as possible. Due to frequent contractions, the heart does not get enough rest and quickly becomes exhausted. The result is heart failure - a discrepancy between the body's oxygen needs and the work of the heart.
Therefore, if tachycardia occurs, you should consult a doctor. Even in the absence of specific symptoms that would accompany a rapid heartbeat, it is enough to first visit a therapist. After conducting the necessary examinations, he will refer you to the appropriate specialist.
Physiological causes of the disorder
Against the background of hypertension, high pulse pressure of a physiological nature can be observed, which affects patients with an unstable nervous system. As a rule, the disorder is short-lived, about 20–25 minutes. Heart rate reaches 100/140 beats/min, after which it stabilizes.
A physiological number of factors that provoke an attack of tachycardia:
- increase in body temperature;
- overdose or individual intolerance to medications;
- long stay in a stuffy room;
- consumption of alcoholic beverages, nicotine;
- excessive mental stress;
- eating large amounts of fatty foods;
- excessive consumption of caffeinated drinks.
Stress causes a sharp increase in the concentration of catecholamines, an increase in heart rate and pressure, the stabilization of which occurs over a long period of time.
Physical activity can also increase the number of heart contractions, but the level of blood pressure should remain within the original limits.
No ads 1
Pathological causes of the disorder
The development of the pathological form of the disease is associated with functional changes in the functioning of the heart, kidneys, thyroid gland or the presence of infectious agents in the body. The attacks are longer and are not caused by physiological factors.
The group of main pathologies that cause increased heart rate and increased blood pressure includes:
Can there be a fever with high blood pressure?
- Hypertensive crisis of the first type (sympatho-adrenal crisis). When the regulation of the autonomic system is disrupted, the body's normal reaction to stimuli is disrupted, which is associated with diseases of the cardiovascular system.
- Arterial hypertension of various etiologies. It is observed in cases of hormone imbalance, renal failure, and vascular regulation disorders.
- Hyperthyroidism. An increase in sympathetic activity occurs when the metabolism of thyroid hormones is disrupted. The pathology is characterized by sinus tachycardia, provided that foci of ectopic activity remain in the myocardium.
- Hypercorticism. The pathological condition is caused by hormonal imbalance due to excessive activity of adrenal hormones. The disease is characterized by a mechanism of increased automatism of the sinus node.
- Diseases of neurogenic and psychogenic nature. Minor positive or negative emotions provoke tension in the nervous system. Cardiovascular neurosis causes increased heart rate as a result of dysregulation of the autonomic nervous system with increased sympathetic nerve activity.
In cases where an increased pulse is diagnosed with increased pressure, the risk of developing vascular complications increases, which can cause rupture of blood vessels in the brain or heart. This pattern affects people aged 45 to 55 years, so the higher the pulse and blood pressure, the higher the risk of negative consequences.
Excessive blood pressure response to CST
In addition to establishing an upper BP threshold for exercise cessation, the AHA established an excessive BP response to exercise >210 mmHg. Art. for men and >190 mm Hg. Art. for women, as well as an increase in DBP >10 mm Hg. Art. compared to the resting value or above the value of 90 mmHg. Art., regardless of gender (3). Validation of the systolic criterion appears to be based on data described in a review (52), whereas the criteria for abnormal DBP response arose from a series of studies predicting an increase in resting DBP (53). ACSM currently defines excessively elevated BP as an absolute SBP >250 mmHg. Art. or relative increase >140 mm Hg. Art. (2), however, the source of these values is unknown and the criteria have changed over time. For example, the AHA confirmed the clinical need for excessive BP values but refrained from proposing threshold values (54), whereas previous ACSM recommendations cited systolic and DBP >225 and >90 mmHg as response criteria. Art., respectively (55).
Many studies linking exaggerated BP responses to exercise with latent hypertension have not used recommended thresholds but have used arbitrary thresholds (8, 14, 15, 53, 56 – 59), values >90th or 95th percentile (11 – 59). 13) or the values of people from the top tertile (10, 60). Figure 4 provides a summary of BP thresholds used in previous hypertension-related studies of individuals with excessive BP. To date, the lowest threshold has been established by Jae et al (17) - 181 mmHg. Art. – as the most selective SBP threshold for predicting hypertension in men during a five-year follow-up. Several studies have used magnitude of change rather than absolute value to define excessive BP. Matthews et al (9) used a change in SBP >60 mmHg. Art. at 6.3 MET or >70 mm Hg. Art. at 8.1 MET; Lima et al (61) used an increase in SBP >7.5 mmHg. st./MET. For DBP, several studies have used increases >10 mmHg. Art. (9, 53, 56) or 15 mm Hg. Art. (61) with CST. Not surprisingly, the lack of consensus on the definition of excessive BP has led to discrepancies in incidence estimates ranging from 1 to 61% (59, 62).
Rice. 4. Generalized thresholds for systolic blood pressure (SBP; a) and diastolic blood pressure (DBP; b), which are used to identify excessive blood pressure responses.
Dashed lines are sex-specific thresholds recommended by the American Heart Association (AHA) (3) and the American College of Sports Medicine (ACSM) (2). Source studies are listed at the bottom of each column.
Most studies assessing excessive BP during exercise have included a narrow age group of men (middle-aged), which limits the applicability of the results to all people. A single study of young adults (25 ± 10 years), involving 76–77% of competitive male athletes, concluded that exercise BP was the best predictor of future BP (53). Several studies have assessed men and women, and similar thresholds have been applied to both sexes (8, 13, 59). Only one study examined age- and sex-specific criteria for excessive BP based on values above the age/sex 95th percentile (12). The values used were obtained from the second stage of the Bruce protocol, for both sexes, only excessive BP was associated with an increased risk of hypertension.
In addition to emphasizing the importance of DBP in predicting future events, this study poses two key questions: is the best criterion for BP, and how to obtain BP values during exercise? Limited evidence suggests that the excessive increase in blood pressure seen early in CST may be more clinically significant. Holmqvist et al (16) observed people who reached their maximum BP late in the CST without having the same risk of hypertension as people who reached that BP early in the test. To date, studies have performed manual auscultation with various sphygmomanometers or used automatic oscillometric devices. Auscultation is complicated by motion artifacts and ambient noise, and oscillometric devices assessed DBP through measurement of mean arterial pressure (63). In all cases, numerous errors and assumptions are possible, including the validity and reliability of data from each device, which are typically obtained in a homogeneous population and are not valid in others (64), and the use of DBP estimates to attribute risk.
Although there is sufficient evidence to support the association between exaggerated BP responses to exercise and the risk of latent hypertension, more rigorous methodology for identifying “abnormal” responses is required for additional factors of age, sex, fitness and comorbidities, particularly the use of a single value at peak exercise. The rate of change in BP, plotted as the slope of the curve in Figure 5, provides the most reliable approach to classifying individuals as normal or overresponsive. However, the hypertensive response to exercise will help uncover pathologies (eg, coarctation of the aorta), improve risk stratification, increase the sensitivity of exercise imaging studies, and improve the identification of strategies in cases of borderline hypertension.
Rice. 5. Changes in systolic blood pressure (SBP) relative to metabolic equivalent (MET) - shown as different colored lines for three hypothetical respondents.
Dashed lines indicate sex-specific thresholds recommended by the American Heart Association (AHA) (3) and the American College of Sports Medicine (ACSM) (2). Red and green reactions are stopped at similar levels determined by the AHA. However, the theoretical response shown in green appears to be more clinically significant. Likewise, although the red and blue lines reach similar MET (training) levels, there are clear differences in response patterns.
By what signs can a deviation be identified?
Every hypertensive person has the concept of “working” pressure, which means pressure indicators at which the general condition is within normal limits. This indicator is individual for each person, since it can be either normal or elevated (135/100). However, a slight excess of the norm can cause a number of uncomfortable sensations. A short-term and slight acceleration of the heart rate does not provoke pronounced symptoms, but is accompanied only by the occurrence of tinnitus and uncomfortable feelings.
A prolonged attack of high blood pressure and high pulse is characterized by the following symptoms:
- Throbbing headache localized in the temporal and occipital region.
- Dizziness with concomitant loss of coordination of movements.
- Visual impairment (darkening, flickering “flies” before the eyes).
- Cardiac dysfunction (irregular rhythm, feeling of rapid heartbeat).
- Increasing shortness of breath, feeling of lack of air.
- Unreasonable muscle weakness, a feeling of trembling throughout the body.
- Nausea followed by vomiting.
The severity of symptoms depends on the state and sensitivity threshold of the autonomic nervous system, as well as on the stage of hypertension. Thus, an increase in cardiac activity can lead to the development of heart failure and angina.
Possible consequences and complications
Dissonance between pulse and blood pressure is dangerous for the functional state of the body, since with a rapid heartbeat, hypoxia of tissues and organs occurs, which entails the development of irreversible changes in them.
With a simultaneous increase in diagnostic indicators, the following very dangerous conditions may occur:
- disorder of the digestive tract;
- ischemic brain damage;
- necrosis of the cardiomyocyte area;
- arrhythmic shock.
A prolonged and constant increase in heart rate can significantly reduce the performance of a hypertensive patient. The patient experiences a feeling of irritability and complains of causeless weakness and malaise.
Under conditions of excessive load, the myocardium requires more oxygen, which leads to its increased waste. In vessels of small diameter, a deficiency of nutrients occurs, provoking the formation of cardiomyopathy.
Low performance is always a problem.
NO. Don't rely only on optimal values. For some, a heart rate of 40-50 beats per second is a serious problem, and for some healthy young people it is a sign that they are in good shape. Low blood pressure is a little more complicated, especially in people with heart disease and the elderly. However, if the decrease is abnormal, you will feel weak and dizzy. The numbers themselves do not have much meaning, what is important is how you feel under these parameters.
Providing self-help
What to do if there is a sharp increase in heart rate against the background of high blood pressure? In this situation, you should contact a specialist to clarify the diagnosis and identify the root cause of the disorder. However, functional etiological factors can also cause tachycardia, for which first aid can be provided independently.
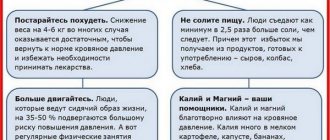
First you need to determine the source causing the violation. The patient is recommended to rest, have a good night's sleep, and also have a fasting day that excludes fatty, spicy, and sweet foods. To prevent worsening of the pathology, caffeine drinks, smoking and alcohol should be avoided.
Algorithm for providing assistance:
- Remove constrictive clothing and provide fresh air.
- Take a horizontal position or half-sitting with support under your spine.
- Take sedatives (Persen, Validol, Fitosed, motherwort tincture).
- To lower your blood pressure, take the prescribed antihypertensive pills (Captopril, Captopress, Enap).
- Use a breathing technique with deep inhalation and slow exhalation.
- Massage the area of your eyeballs and temples if you have a headache.
Important! Monitor indicators every 30 minutes. If the use of therapeutic measures does not have the desired effect, then a medical team should be called.