Bacterioscopy is the most common gynecological test. Women and girls of different ages are required to undergo this procedure when undergoing a medical examination. In 50-60% of them, cocci are detected in a smear for flora. In men they are much less common. This is due to the structural features of the female reproductive system. Cocci can also be detected in a child’s smear.
Under certain circumstances, bacteria can provoke serious diseases of the genitourinary and other organs, so it is advisable to find out what they are, when they threaten health and how to deal with them.
What is cocci
There are many different microbes present in the human body. Cocci are a family of single-celled organisms, named from the word coccus, which means “spherical” in Latin and “grain” in ancient Greek. Like other bacteria, cocci have the unique ability to reproduce intensively (about every half hour). Under favorable conditions, unicellular organisms divide in two, i.e. are crushed, which is why they are also called “fragmented”, and then either exist separately or are combined into groups. Cocci are nonmotile, do not form spores, and are anaerobic (can live in an airless environment).
What are gonococci?
The causative agent of gonorrhea is non-stainable, immobile bacteria that are arranged in pairs. Outwardly, they resemble coffee beans. Bacteria are not afraid of phagocytosis. Despite all the body's attempts, they continue to be active and reproduce.
Antibacterial drugs are often used to combat gonococci. If you take them incorrectly, then it is impossible to achieve the effect. Under the influence of agents, the walls of bacteria are destroyed, but the ability to develop remains. Due to their high survivability, they are able to change characteristics. In the presence of carbon dioxide and normal temperature conditions (37 0C), gonococci actively multiply in an artificial nutrient medium.
Normal microflora
The healthy microflora of the female genital organs consists of lactobacilli - Dederlein bacilli, bifidobacteria and a small (about 5%) amount of cocci. This ensures the normal course of processes such as:
- metabolism;
- regulation of acidity levels;
- destruction of pathogenic microbes.
The presence of cocci in a smear in women is not dangerous and natural. When the balance of microorganisms is maintained at the proper level, beneficial lactobacilli multiply in an acidic environment and create protection against fungi (thrush), E. coli and other harmful microbes. Accordingly, the genitourinary system functions stably and fully.
Receiving material
Cervical cancer most often develops in the transformation zone, it is preceded by background processes and intraepithelial lesions (epithelial dysplasia), which can be located in small areas, so it is important that material is obtained from the entire surface of the cervix, especially from the junction of squamous and columnar epithelium . The number of altered cells in a smear varies, and if there are few of them, then the likelihood increases that pathological changes may be missed when viewing the specimen. For effective cytological examination it is necessary to consider:
- During preventive examinations, cytological smears should be taken from women, regardless of complaints, the presence or absence of changes in the mucous membrane. Cytological examination should be repeated at least once every three years;
- it is advisable to obtain smears no earlier than on the 5th day of the menstrual cycle and no later than 5 days before the expected start of menstruation;
- you cannot take material within 48 hours after sexual intercourse, use of lubricants, vinegar or Lugol’s solution, tampons or spermicides, douching, insertion of medications, suppositories, creams into the vagina, including creams for performing ultrasound examinations;
- pregnancy is not the best time for screening, as incorrect results are possible, but if you are not sure that the woman will come for examination after childbirth, it is better to take smears;
- for symptoms of acute infection, it is advisable to obtain smears for the purpose of examining and identifying pathological changes in the epithelium, the etiological agent; Cytological control is also necessary after treatment, but not earlier than 2 months. after completing the course.
Material from the cervix should be taken by a gynecologist or (during screening, preventive examination) by a well-trained nurse (midwife).
It is important that the smear contains material from the transformation zone, since about 90% of tumors come from the junction of the squamous and columnar epithelium and the transformation zone, and only 10% from the columnar epithelium of the cervical canal.
For diagnostic purposes, material is obtained separately from the ectocervix (vaginal portion of the cervix) and endocervix (cervical canal) using a spatula and a special brush (such as Cytobrush). When conducting a preventive examination, Cervex-Brush, various modifications of the Eyre spatula and other devices are used to obtain material simultaneously from the vaginal part of the cervix, the junction (transformation) zone and the cervical canal.
Before obtaining the material, the cervix is exposed in “mirrors”; no additional manipulations are performed (the cervix is not lubricated, mucus is not removed; if there is a lot of mucus, it is carefully removed with a cotton swab without pressing on the cervix). A brush (Eyre spatula) is inserted into the external os of the cervix, carefully guiding the central part of the device along the axis of the cervical canal. Next, its tip is rotated 360° (clockwise), thereby obtaining a sufficient number of cells from the ectocervix and from the transformation zone. The instrument is inserted very carefully, trying not to damage the cervix. Then the brush (spatula) is removed from the canal.
What do cocci say in a smear?
When the microclimate is disturbed, the picture changes: the content of cocci increases, and beneficial bacteria die, so if the number of cocci in a smear exceeds the norm, this indicates health problems.
Normal: pH (acidity level) – up to 5. Weakly acidic environment (beginning of the inflammatory process): pH – up to 7. Increased alkaline environment (infection or inflammation is actively developing): pH – more than 7.5.
To determine a specific disease, it is necessary to establish which type of spherical bacteria is present in excess, and also to determine the presence of gram-negative and gram-positive cocci in the smear. These terms originated with the Danish scientist Gram and his method for identifying drug-resistant cocci. The fact is that many bacteria have a very strong shell, impenetrable to most common antibiotics (Gram-negative). But those microorganisms whose cell wall is destroyed under the influence of antibacterial drugs (Gram-positive) are also capable of causing serious pathologies, since as a result of their breakdown products, intoxication of the body occurs. Only thanks to a strong immune system and compliance with all treatment rules, the bacterial norm is restored.
To the question: “What do cocci mean in a woman’s smear?” You can answer this: vaginal dysbiosis, decreased protective functions of lactobacilli and an increased likelihood of inflammatory processes. Cocci in a smear in men also indicate a malfunction of the genitourinary system.
Attention! This condition requires qualified medical care. Traditional methods, self-administration of antibiotics and other medications are extremely undesirable and can only aggravate the situation.
Why do you need a flora smear?
A gynecological smear is what the doctor should first recommend at the initial appointment, regardless of the symptoms. This study, along with colposcopy, is included in the gold standard for annual preventive examinations in women. Smear microscopy allows you to assess the condition of the vagina and the presence/absence of an inflammatory process in the organs of the reproductive system. The laboratory technician will see the number of leukocytes, epithelial cells and the ratio of bacteria on the slide. If cocci predominate over beneficial bacilli in the results or fungi are visualized, this means dysbiosis, inflammation or candidiasis. If the number of leukocytes in the smear is increased, the gynecologist may prescribe additional tests for STIs.
Types of cocci
There are several types of bacteria, many of which are opportunistic:
- Diplococci (more than 80 species are known). They exist in pairs and are gram-negative and gram-positive. The most pathogenic type is gonococcus, the causative agent of gonorrhea. The disease ranks first in terms of prevalence among STIs (sexually transmitted infections).
- Streptococci are microbes connected in a chain. Externally, cocci in a smear look like rods formed from several spherical cells. To date, more than 100 types of streptococci (all gram-positive) have been discovered. By multiplying in the genitals, they cause vaginitis (inflammation of the vagina), cystitis (inflammation of the bladder), cervicitis (inflammation of the cervix), endometritis (inflammation of the uterine lining) and other pathologies.
- Staphylococci (gram-positive). They are clusters similar to bunches of grapes. There are 27 types of pathogens, the most dangerous is Staphylococcus aureus. The presence of a large number of staphylococci in the vagina contributes to the active proliferation of other pathogens, such as candida fungi (thrush). Against this background, the mucous membrane and appendages of the uterus often become inflamed.
- Enterococci (oval-shaped cocci, arranged in chains or pairs) are opportunistic representatives of the intestinal microflora, which, in the absence of hygiene, can rapidly develop in the genitourinary system.
- Coccobacilli (an intermediate form between bacilli and cocci). Haemophilus influenzae, gardnerella, chlamydia are detected in the presence of sexually transmitted diseases and bacterial vaginosis.
- Gonococci. They have a gram-negative structure and an oval shape. When the genitourinary tract is damaged, they cause an inflammatory reaction with the subsequent development of cervicitis and salpingitis.
Coccobacilli - what is it?
The content of the article
Coccobacillary flora is the presence of a certain kind of bacteria, which are combined into 2 subspecies - bacilli and cocci. These include chlamydia and the causative agents of the disease - gardnerellosis. An imbalance in the flora of the genital organs occurs due to an increase in the number of coccobacilli. When this is associated with bacteria that are spread sexually, bacterial vaginosis develops, affecting hundreds of millions of women on earth. Cocci are beneficial microorganisms up to a certain point, but if the polymorphic flora is disturbed, the alkaline environment of the vagina increases, then the protection disappears and pathogenic bacteria begin to be active spread throughout the genitals, worsening the patient’s well-being. The appearance of cocci in a woman’s vagina can be caused by various factors, including:
- sexually transmitted infections;
- ignoring the rules of personal hygiene;
- weakening of the immune system;
- allergic reactions;
- long-term use of antibiotics;
- hormonal disorders;
- masturbation with dirty hands and so on.
The optimal ratio of coccobacillary flora in the female body. A control smear is taken at each scheduled visit to the gynecologist, or in the presence of painful symptoms of the reproductive system. Thanks to this analysis, the number of cocci bacilli in the discharge is determined. The resulting analyzes can be divided into 3 types:
- In a slightly acidic environment, pH values do not exceed 5.0.
- Moderate value for a neutral environment – pH 7.0.
- An alkaline environment is characterized by pH values greater than 7.5.
If the results obtained do not correspond to statistical data, then we are talking about the emergence of gram-positive cocci, which destroy the vaginal microflora and lead to deterioration of the patient’s reproductive system. When the mixed flora in the smear approaches alkaline in terms of indicators, then we can talk about the development of dysbacteriosis, due to advanced inflammation of the genital organs. Attention: multiplication of cocci is often a common cause of infertility, and therefore you should not delay a trip to the gynecologist (if specific discharge and pain in the ovarian area appear).
Causes
There are a huge number of factors that provoke pathology. The main causes of cocci in a smear:
- Incompetent treatment. If a person takes antibacterial drugs without prescription or does not comply with the dosage, the likelihood of being affected by pathogenic microbes increases many times over.
- Neglect of personal hygiene. Ignoring basic rules and incorrectly performing procedures increase the risk of disruption of the vaginal microflora. It must be remembered that soap is an alkali, and washing too deeply has a negative effect on the acid-base balance. For women, girls and girls it is advisable to use special intimate hygiene products. It is also important to perform manipulations from the vagina to the anus, and not vice versa.
- Wearing underwear made of dense materials or synthetics has a bad effect on the microclimate of the genital organs.
- Disorderly sex life. Unprotected contact with a carrier of pathogenic microbes leads to infection in 99 cases out of 100. In addition, if you do not have a regular partner and regularly have sex, the microflora will inevitably be exposed to “foreign” bacteria.
- Douching. Due to frequent douching, beneficial flora is washed away.
- Hormonal imbalances. Hormonal imbalances cause bacterial imbalance.
- Weakened immunity. When the body's protective functions are reduced, it cannot resist dangerous pathogens.
Integration of various laboratory methods
In the diagnosis of cervical diseases, clinical data and microflora test results (classical microbiological (culture), ANC methods (PCR, RT-PCR, Hybrid Capture, NASBA, etc.) are important).
If it is necessary to clarify the pathological process (ASC-US, ASC-H), cytological examination is, if possible, supplemented with molecular biological ones (p16, oncogenes, methylated DNA, etc.).
HPV detection tests have low prognostic significance, especially in young women (under 30 years of age), due to the fact that in most patients in this age group, HPV infection is transient. However, despite the low specificity of the test for intraepithelial tumors and cancer, it can be used as a screening test in women under 30 years of age, followed by cytological examination. Sensitivity and specificity increase significantly with the combined use of the cytological method and research to detect HPV, especially in patients with questionable cytological data. This test is important in the management of patients with ASC-US, during follow-up to determine the risk of relapse or progression of the disease (CIN II, CIN III, carcinoma in situ, invasive cancer).
Associated symptoms
Alarming signs associated with a violation of the microflora of the urogenital area are difficult to miss in 90% of cases. In women, vaginal discharge acquires a specific smell (fermented milk or fishy) and becomes abundant.
Common symptoms of cocci in a smear for men and women:
- discomfort during urination and intimacy;
- itching and burning of varying degrees of severity;
- swelling of the genitals;
- yellowish, white, purulent, bloody discharge from the genitals.
Women often complain of pain in the lower abdomen, weakness, and lack of appetite. This is due to the fact that during their life, pathogenic cells produce toxic substances. Foci of inflammation also form, causing noticeable discomfort.
If you have the above symptoms, you should immediately see a gynecologist, get tested and undergo a full course of therapy. Self-medication is prohibited!
Classification
There are several types of classification of vaginal candidiasis. Depending on the characteristics of the course, acute and chronic (recurrent) forms of the disease are distinguished. In the first case, the pathology is characterized by vivid symptoms and occurs no more than four times a year. With chronicity, the symptoms are usually less pronounced, and the disease itself recurs 4 times a year or more often.
Depending on the presence of complications, uncomplicated and complicated vaginal candidiasis is distinguished. In the first case, the process is relatively easy and can be stopped quite quickly with the selection of adequate therapy. As a rule, it occurs in women who do not have additional risk factors (diabetes mellitus, immunodeficiency states of various origins).
The complicated form of vaginal candidiasis is characterized by pronounced symptoms that negatively affect the patient’s daily life. As a rule, inflammation spreads to the external genitalia, causing the appearance of ulcers and cracks. This form often recurs.
Localization of the pathological process allows us to distinguish three forms of the disease:
- vaginitis: inflammation affects only the vaginal mucosa;
- vulvovaginitis: the external genitalia and vagina are affected;
- cervicitis: the cervix is involved in the process.
Complications
If you are not examined in time and treatment is not started, coccal infections will spread to neighboring organs, mucous membranes and skin. Complications largely depend on the type of cell. For example, streptococcus provokes meningitis, pneumonia, osteomyelitis (bone tissue damage). Staphylococcus causes endocardium (inflammation of the inner lining of the heart), pyoderma (purulent inflammatory processes under the skin), pneumonia, bronchitis, diseases of the upper respiratory tract (rhinitis, sinusitis) and the digestive tract. In addition, the proliferation of pathogenic bacteria in the vagina reduces the production of estrogen, which ultimately causes miscarriages and infertility.
Cocci in a smear during pregnancy complicate the process of bearing a child. The growth and development of the fetus are directly related to the health of the expectant mother, and the inflammatory process can affect not only the rectum and urinary canal, but also the uterus. To prevent danger, pregnancy should be planned in advance and, if necessary, therapy.
The most common consequences of coccal infections:
- cervical erosion;
- endometritis;
- pyelonephritis (kidney damage).
In men, in the absence of adequate treatment, cocci lead to prostatitis (inflammation of the prostate), damage to the testicles and seminiferous tubules. All this threatens impotence and infertility.
Tests for infections
Analysis for infections (STDs and opportunistic flora). Not all bacteria and viruses found in the vagina need to be treated. For example, you were diagnosed with ureaplasma. It belongs to the opportunistic flora, which has the right to be in the vagina. Under favorable conditions, its presence does not cause inflammation and there is no need to treat it (the same applies to other u/n bacteria). It is necessary to treat only chlamydia and mycoplasma genitalium . These are true pathogens, and even in small quantities they should not exist. And everything else needs treatment only if there is inflammation and discomfort.
So: if a conditionally pathogenic flora is discovered, it needs treatment only with concomitant inflammation. If there is no inflammation, live calmly and don’t eat handfuls of extra medicine!
Yana Aleksandrovna Nikitenko, obstetrician-gynecologist, ultrasound diagnostics specialist.
Diagnostics
Diagnosis is a laboratory examination. In women, a smear is taken from the back wall of the vagina, urethra and cervical canal. For men, a special probe is inserted into the urethra (if inflammation has already begun, manipulation can be painful). Next, a sample of the biomaterial is sent to the laboratory, where it is stained (Gram method) and examined under a microscope. In some cases, additional diagnostics may be required: a swab from the throat and nasal cavity (if staphylococcus is suspected), general blood and urine tests.
Before carrying out the procedure, it is important to adhere to the following rules:
- do not urinate for 2 hours;
- do not consume spicy food and alcohol for 3-5 days;
- do not take medications for 3-5 days;
- abstain from intimacy for 2 days;
- do not use vaginal suppositories, do not douche for 2 days.
Attention! The analysis is taken before menstruation or 4-5 days after its end.
Microflora of the urogenital tract in men examined for chronic prostatitis
Treatment of chronic inflammatory pathology of the urogenital tract in men has always been a difficult task in urology. Treatment for these diseases, especially those complicated by impaired fertility, sexual dysfunction, pelvic pain syndrome, can be successful if done individually and based on knowledge of the etiology of the inflammatory process, immunoreactivity to this inflammatory process and morpho-functional changes in the pelvic organs.
In widespread medical practice, at present, when diagnosing the etiological factor of inflammatory pathology of the urogenital tract, the emphasis is on identifying sexually transmitted infections. The purpose of this study is to demonstrate the significance of other, no less important, etiological factors, as well as the place of STIs in the pathogenesis of this group of inflammatory diseases. An infectious inflammatory process in the urogenital tract occurs by two mechanisms.
In the first case, a virulent STI causes clinically and laboratory identifiable urethritis, which subsequently leads to the occurrence of an ascending inflammatory process. The pathogenetic role of sexually transmitted infection in this case is obvious: when examining discharge from the urethra, prostate secretion, seminal fluid, a significant increase in the number of leukocytes and STIs is revealed; The primary inflammatory process begins with the clinical picture of urethritis. Patients with an inflammatory process of this nature are most often treated in dermatovenerological dispensaries, when in addition to acute venereal disease there is a prostatitis clinic.
The second mechanism is more complex. The occurrence of an infectious inflammatory process in the urogenital tract in this case is preceded by certain predisposing factors.
Let's highlight several main groups:
- The first group of factors includes vascular, trophic and morpho-functional changes in the pelvic organs, which arise as a result of congestion in the pelvic organs, habitual intoxication and other reasons. These changes are well known and widely discussed in the specialized domestic literature.
- Infravesical obstruction is also a predisposing cause of infectious inflammation. In this case, a retrograde flow of urine occurs into the acini of the prostate gland at the time of urination due to an increase in intraurethral pressure. This can lead to infection of the prostate gland by microflora from the overlying urinary tract.
- The most important predisposing cause of the inflammatory process of the urogenital tract is secondary immunodeficiency, which develops against the background of a sluggish bacterial intracellular infection (chlamydia, mycoplasma) and persistent viral infection (urogenital herpes, cytomegalovirus). Infection of the urogenital tract with this microflora leads to a characteristic disturbance of phagocytic activity (HCT test), a decrease in class A immunoglobulins with an increase in class G immunoglobulins; disruption of T helper and T suppressor interaction. Secondary immunodeficiency, as well as certain morpho-functional changes in the pelvic organs open the way to infection of the urogenital tract with banal pathogenic and conditionally pathogenic bacterial microflora.
With the development of an infectious process in the urogenital tract according to this mechanism, there is no clinical manifestation of urethritis, in studies of discharge from the urethra there will be no significant increase in the number of leukocytes, in scrapings from the urethra STIs will be detected much less frequently, however, patients will have a clinically and laboratory identifiable inflammatory process in the prostate-vesicular complex or in the scrotal organs.
In the presence of the above predisposing factors, infection of the urogenital tract with banal bacterial microflora is fundamentally possible in two ways: transurethral and hematogenous.
Hematogenous infection most often occurs from foci of chronic infection with concomitant ENT pathology, diseases that are widespread among the population; for diseases of the rectum with chronic constipation, hemorrhoids (especially with frequent exacerbations). Infection through this route most often occurs when there are already pronounced structural changes in the prostate gland (congestion, calcifications, BPH).
The transurethral route of infection with secondary bacterial microflora is more significant. Four main sources of bacterial infection should be identified.
- Widespread bacterial vaginosis in women. According to the Preobrazhenskaya Clinic, women examined for inflammatory diseases of the genital organs were diagnosed with bacterial vaginosis in 20% of cases. The cause of bacterial vaginosis is small opportunistic rod flora, which often leads to infection of the urogenital tract of men. The cause of bacterial vaginosis is sluggish bacterial and persistent viral infections, hormonal disorders and other causes that cause secondary immunodeficiency. In married couples, women suffering from bacterial vaginosis and husbands are much more likely to have chronic prostatitis than women with inflammatory gynecological diseases, but not having bacterial vaginosis.
Table of microorganisms most often found in the genital organs of women with inflammatory diseases caused by gardnarella vaginalis and non-spore-forming bacteria. (collection of works of UrNIIDVII, 1985)
| Types of microorganisms. | Morphological features. |
| Garnarella vaginalis | Coccobacilli single, paired, polymorphic |
| Undifferentiated species | Coccobacilli polymorphic |
| Coryneforms | Club-shaped sticks |
| Bifidobacteria | The rods are variable, often with forked ends. |
| Bacterioids | Rods, coccobacilli, often bipolarly colored |
| Lactobacilli | Polymorphic shelves, often arranged in long filaments. |
| Anaerobic cocci | Cocci, solitary, in groups or in chains. |
| Aerobic cocci | Cocci, chains, tetrads, clusters. |
| Propionibacteria | Polymorphic rods, club-shaped, coccoid. |
| Cellos | Cocci, diplococci, clusters or chains. |
| Fusobacteria | The rods are large, polymorphic, often long with pointed ends, and may have thickenings in the center. |
- The prevalence of oral-genital and anal sexual intercourse is also a source of infection of the urogenital tract of men. In the first case, infection occurs predominantly with streptococcal or staphylococcal microflora, in the second case - with Gr-bacillus flora (Proteus, Klebsiella, Escherichia coli, etc.).
Clinical case.
Patient N13603 Igor Nikolaevich, 30 years old, applied on May 16. 98 years old with complaints of pelvic pain. Examined at UrNIIDVII for the presence of STIs - gonorrhea, trichomoniasis, candidiasis, gardnarellosis, chlamydia, ureaplasmosis, mycoplasmosis, HSV were not found, in the secretion of the prostate gland there were 20-40-80 leukocytes per p/z, there was no evidence of extragenital inflammatory pathology. A bacteriological study of prostate secretions was performed. Staphylococcus with hemolysis and Gr+ bacillus with hemolysis were detected, TMC 10x9 in 1 ml of discharge. Upon further questioning, it was found that the family regularly practices oral-genital sex, and the wife suffers from chronic tonsillitis and sinusitis with frequent exacerbations. The wife (N13784 Anna Sergeevna, 29 years old) was referred to an otolaryngologist. A bacteriological study of tonsil washings revealed staphylococcus with hemolysis, Gr+ rod with hemolysis, TMC 10x6 in 1 ml of discharge, the presence of chronic tonsillitis and sinusitis in the subacute phase was confirmed.
- Iatrogenic infection by hospital microflora during urethral therapeutic or diagnostic procedures, which are widespread at present.
- Infection from the upper urinary tract and bladder, especially in the presence of bladder outlet obstruction.
The mechanism for the development of bacterial inflammation in the urogenital tract, when its cause is not sexually transmitted infections, is clearly presented below.
The purpose of this work was to analyze the microflora in patients examined for chronic prostatitis. In addition to examinations for STIs, over 1996-98, the Preobrazhenskaya Clinic performed more than 200 bacteriological cultures on men for various indications.
Bacteriological research of prostate secretions is carried out on the basis of the bacteriological laboratory of the UrNIIDVII. Before collecting the material, the patient is asked to empty the bladder and toilet the glans penis and preputial sac. Next, a massage of the prostate gland is performed, its secretion is placed in a test tube with a storage medium - sugar broth. Test tubes in a thermostat are delivered to the bacteriological laboratory within 40-60 minutes, where the material is immediately dispersed into 4 nutrient media: meat peptone agar, blood agar, Endo medium and Sabour medium. After 24 hours, for further identification of the pathogen, subculture is carried out on appropriate nutrient media (for example, to identify staphylococcus in yolk-salt agar to assess lyceto-vitellase activity, in blood plasma to assess plasma-coagulating activity). After 5 days, the results are “read”, pure cultures are transferred to media with disks soaked in antibacterial drugs, and after 24 hours the antibiogram is “read”.
The study group included only those patients who, despite the presence of clinical and laboratory data for the inflammatory process in the prostate-vesicular complex, did not have any data for inflammation in the urethra, those who met the following conditions below.
- Minimum scope of examination: smear analysis, examination of prostate secretions, examination for chlamydia, ureaplasmosis, mycoplasmosis, chronic gonorrhea, blood for HIV, RW, bacteriological examination of prostate secretions, ultrasound of the prostate gland with a transrectal sensor.
- The entire examination complex was completed within no more than 14 days.
- There is no clinical evidence of urethritis, and in the study of leukocytes discharged from the urethra there are less than 10 leukocytes in the field of view.
- Negative Wesserman reaction and absence of HIV.
Thus, in the study group there were 63 patients in whom 113 microorganisms were isolated in a bacteriological study of prostate secretions. The age of the patients ranged from 20 to 65 years. Let us note a certain pattern in the total degree of leukocytosis in prostate secretions in patients of different age groups.
| Age | Number of persons | % | Leukocyte count min | White blood cell count average | White blood cell count max |
| 20-29 years old | 18 | 28 | 21 | 35 | 65 |
| 30-39 years old | 25 | 40 | 34 | 58 | 101 |
| 40-49 years old | 13 | 21 | 27 | 44 | 93 |
| 50-65 years | 7 | 11 | 24 | 44 | 83 |
In the first age group, due to the fact that the inflammatory process began relatively recently, leukocytosis is still quite moderate. In the second group, where the history of the inflammatory process is already long, and the immune response to the inflammatory process is quite active, leukocytosis is the highest of the groups presented. In the third and fourth groups, despite pronounced structural changes in the prostate gland, leukocytosis decreased again. This may be due to a significant decrease in the immune response during a long-term chronic inflammatory process.
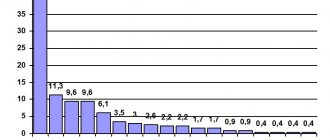
The structure of the identified microflora in the bacteriological study of prostate secretion is presented in Table N1.
The data from the research performed must be assessed with a high degree of criticality for the following reasons:
- This laboratory does not have an anaerostat to perform inoculation under anaerobic conditions, therefore the number of anaerobic microorganisms should be significantly greater.
- A significant increase in opportunistic microflora sometimes obscures the true causative agent of inflammation. During repeated bacteriological examination after treatment, pathogenic microflora are sown much more often. However, this topic is beyond the scope of this work.
Both pathogenic and opportunistic microorganisms were identified. The ratio of pathogenic and opportunistic microorganisms is presented in the diagram.
Microorganisms were sown both as a monoinfection and in associations, which is presented in Table N2.
Thus, it is clear that in 68.2% of cases, in a bacteriological study of prostate secretions, associations of microorganisms are sown. Note that in 46% of those examined (those 29 patients out of 63), microorganisms causing hemolysis of blood agar were identified in the secretion of the prostate gland, and the higher the degree of association, the more often a hemolytic microorganism is detected in its structure. More than half of the patients are diagnosed with STIs, and their detection rate remains almost the same regardless of the degree of association.
These data are presented in table N2.
Table N3 shows the identified hemolytic microflora:
The presented diagram shows that the detection of staphylococcal microflora predominates, which corresponds to the general layout of the detected microflora. Second place is occupied by Gram+ rod flora (unidentified Gr+ rod flora and corynobacteria), and streptococcus is in third place. Separately, we note that a certain part of the Gram-rod flora also exhibits hemolytic activity (12.5% of the total number of identified Gram-bacteria).
We classified all other microorganisms as opportunistic microflora. We decided not to isolate microorganisms from this group, which can be considered more likely to be saprophytes. In our opinion, it is necessary to classify a particular microorganism as a saprophytic microflora individually, taking into account all clinical and laboratory diagnostic data.
Opportunistic microflora is presented in Table N4.
Based on the structure of pathogenic and conditionally pathogenic microflora, it is easy to notice that the detected coccal microflora, especially streptococcal microflora, is also characteristic of chronic diseases of the oral cavity. Gr+ and Gr- rod microflora are a common causative agent of bacterial vaginosis in women; in addition, Gr- rod microflora is often a hospital microflora and an infection detected in chronic inflammatory diseases of the urinary system.
In 33 patients i.e. In 52.4% of those examined, in the absence of clinical and laboratory signs of an inflammatory process in the urethra, STIs were detected.
The identified STIs are presented in Table N5.
Gonorrhea was identified by examining scrapings from the urethra using the PCR method.
Yeast cells were detected during bacterioscopic examination of urethral discharge or in bacteriological examination of prostate secretions with identification to species. Chlamydia was identified by examining scrapings from the urethra using PCR or PIF or by the presence of class M immunoglobulins for infection. Ureaplasmosis and mycoplasmosis were identified by examining scrapings from the urethra using the PCR method. HSV and CMV were identified by examining scrapings from the urethra using PCR or by the presence of class M immunogobulins for infection.
A comparative analysis of the detection rate of STIs in patients in two groups was carried out:
Group 1 - bacteriological culture of prostate secretion contains a pathogen, Group 2 - bacteriological culture reveals only opportunistic microflora.
The obtained data are presented in table N6.
Thus, it is clear that candidiasis, ureaplasmosis, mycoplasmosis, and viruses are detected equally in both groups. But in the group with pathogenic microflora, gonorrhea and chlamydia are detected much more often. In practice, in patients with clinical and laboratory data of an inflammatory process in the prostate-vesicular complex and in the presence of chlamydia, hemolytic bacterial microflora is always cultured!!!
Another reason why this work was done is demonstrated by the following diagram.
Conclusions:
- In all patients examined for chronic prostatitis in the absence of clinical and laboratory data of acute or chronic urethritis, bacteriological examination of prostate secretions revealed nonspecific bacterial microflora. In 46% of patients (29 out of 63 people), pathogenic (hemolytic) microflora was detected.
- In 54% of patients, opportunistic microflora was identified; the pathogenicity of this microflora is assessed based on the specific clinical situation, taking into account all examination data.
- In 68% of cases, microorganisms were sown by associations. Moreover, the higher the degree of association, the more often a microorganism with hemolytic activity was identified in it.
- The structure of the bacterial microflora of the urogenital tract in men (both with and without hemolytic activity) suggests its possible source is bacterial vaginosis and diseases of the oral cavity in sexual partners, as well as, possibly, a hematogenous route of infection.
- In 52.4% of patients, in the absence of clinical and laboratory data of acute or chronic urethritis, sexually transmitted infections were detected. Moreover, in cases where gonococci or chlamydia were determined in scrapings from the urethral mucosa by the PCR method, hemolytic microflora was determined during bacteriological examination of prostate secretions.
- Considering the fairly pronounced resistance of the identified microflora to antibacterial drugs, it is recommended to include bacteriological culture of prostate secretions in the examination program for patients with inflammatory diseases of the urogenital tract.
Zhuravlev V.N., Vlasenko L.Yu., Pankov V.I.
Treatment
If an abnormal number of cocci is detected in the smear, treatment should be carried out in accordance with all medical prescriptions. It is strongly recommended not to use general antibiotics. As already mentioned, many cocci are resistant to such medications, so therapy may be not only ineffective, but also dangerous. Under the influence of antibacterial agents, the growth of pathogenic cells will begin to increase, and the number of beneficial bacteria will begin to decrease.
In order for the fight against cocci to be as effective as possible, a sensitivity test is first carried out. Antibioticogram - bacterial culture of the vagina on a nutrient medium allows you to determine the level of susceptibility of pathogenic cells to certain drugs.
Metronidazole is considered one of the most effective drugs against coccal infections. Its main advantage is the absence of contraindications for use during pregnancy and breastfeeding. Together with antibiotics, medications containing lacto- and bifidobacteria are used. To restore normal microflora, vaginal suppositories, ointments and creams with antiseptic properties are used. At the same time, immunomodulatory agents can be prescribed. Douching with herbal decoctions should be performed strictly with the permission of the gynecologist.
Attention! At the same time, your regular sexual partner should also undergo treatment. At this time, it is better to refrain from sex, masturbation, and the use of tampons.
After completing the course of therapy, a smear on the flora is done again. If there is no positive result, another group of antibiotics is selected. In 70-80% of cases, hospitalization is not required; treatment is carried out at home or on an outpatient basis.
Treatment of vaginal candidiasis
Specific treatment aimed at eliminating vaginal candidiasis is carried out only after identifying the pathogen and if the patient has signs of the disease. The basis of therapy is specific antifungal agents: nystatin, clotrimazole, ketoconazole, fluconazole, nitrofungin and others. The specific drug, its dose, frequency of administration and course duration are selected individually depending on the characteristics of the course of the disease, the presence of concomitant pathologies and other factors.
If we are talking about an acute uncomplicated process, the drugs are prescribed in local form in the form of suppositories, vaginal tablets or creams. They are introduced directly into the genital tract, where they stop the active reproduction of the pathogen.
In the presence of complications, as well as in the chronic course of the disease, systemic drugs are used in the form of tablets for oral administration. The application regimen is selected on an individual basis.
Until the manifestations of vaginal candidiasis are completely eliminated, it is necessary to maintain sexual rest in order to minimize injury to the inflamed walls of the genital tract. In chronic cases, condoms must be used. The effectiveness of therapy is assessed 14 days after the start of treatment.
Make an appointment