Hydronephrosis is also called hydrocele of the kidney, since with this disease the outflow of urine in the area of the calyx and pelvis of the organs is disrupted. As a result, these parts of the kidneys expand, which can ultimately lead to irreversible changes (atrophy) in the tissues of these paired organs. Hydronephrosis often develops against the background of urolithiasis, kidney tumors, injuries to the urinary system and other diseases. Damage to the calyx and pelvis of the kidneys causes characteristic symptoms of hydronephrosis in humans.
What is pyelectasia?
Pyeloectasia is an expansion of the renal pelvis (pyelos (Greek) - pelvis; ectasia - expansion). In children, as a rule, pyeelectasis is congenital. If the calyxes are dilated along with the pelvis, then they speak of pyelocalicoectasia or hydronephrotic transformation of the kidneys. If the ureter is dilated along with the pelvis, this condition is called ureteropyeloectasia (ureter), megaureter or ureterohydronephrosis. Pyeelectasis is 3-5 times more common in boys than in girls. There is both unilateral and bilateral pathology. Mild forms of pyelectasis often go away on their own, while severe forms often require surgical treatment.
Make an appointment with a urologist
If you have discovered one or more signs of hydronephrosis, contact our State Urology Center.
We invite you to make an appointment with a urologist at a convenient time. In our clinic you can undergo diagnosis and treatment of hydronephrosis free of charge as part of the compulsory medical insurance program. The sooner the disease is confirmed, the more effective the therapy will be. It is equally important to consult a doctor on time, as this reduces the risk of complications and generally improves the prognosis for recovery. October 19, 2020
Hakobyan Gagik Nersesovich - urologist, oncologist, MD, doctor of the highest category, professor
All the symptoms of the disease...
What can be an obstacle to the outflow of urine?
Often, an obstacle to the outflow of urine from the kidney is a narrowing of the ureter at the junction of the pelvis and the ureter, or when the ureter flows into the bladder. Narrowing of the ureter may be a consequence of its underdevelopment or compression from the outside by an additional formation (vessel, adhesions, tumor). Less commonly, the cause of impaired urine outflow from the pelvis is the formation of a valve in the area of the ureteropelvic junction (high ureteric outlet). Increased pressure in the bladder, resulting from a disruption of the nerve supply to the bladder (neurogenic bladder) or from the formation of a urethral valve, can also impede the flow of urine from the renal pelvis.
Diagnosis of hydronephrosis
In a conversation with the patient, after collecting anamnesis, the doctor determines the diagnostic search algorithm. Upon examination, almost nothing specific can be detected, except that in advanced cases an enlarged kidney can be felt.
It is mandatory to study urine and blood in the laboratory. Diagnosis includes mandatory instrumental examination - kidney ultrasound and radiography. Ultrasound reliably reveals signs of hydronephrosis; if necessary, ultrasound examination of renal vessels is prescribed.
X-rays are performed with intravenous contrast. During the study, kidney function is assessed, it is seen how the contrast agent passes through the calyces and pelvis, where it accumulates, how long it takes to completely filter the blood (excretory urography). In some cases, contrast is injected from below through the ureter, which allows visualization of the level of narrowing (retrograde ureteropyelography). MRI and radioisotope studies are also used as diagnostics. Endoscopic ureteroscopy (examination using an endoscope, which is inserted through the urethra and bladder into the ureter) allows you to clarify all the details and see the narrowing with your own eyes before surgery.
What diagnostic methods are used for pyeelectasis in a newborn?
For mild pyelectasis, it may be sufficient to conduct regular ultrasound examinations (ultrasounds) every three months. If a urinary infection occurs or the degree of pyelectasia increases, a complete urological examination is indicated, including radiological research methods: cystography, excretory (intravenous) urography, radioisotope study of the kidneys. These methods allow you to establish a diagnosis - determine the level, degree and cause of the disturbance in the outflow of urine, as well as prescribe reasonable treatment. The research results themselves do not constitute a verdict that unambiguously determines the fate of the child. The decision to manage the patient is made by an experienced urologist, usually based on observation of the child, analysis of the causes and severity of the disease.
Treatment of hydronephrosis
If the course is asymptomatic and the degree of hydronephrosis is insignificant, a wait-and-see approach is chosen, and the patient is monitored over time. Conservative treatment of hydronephrosis is used in cases of inflammation in preparation for surgery.
The main treatment method for this pathology is surgery. Tumors, metastases, stones are removed, congenital malformations are eliminated.
Practice shows that the maximum number of narrowings occurs in the ureter. It is enough to eliminate the narrowing in this place, and the normal outflow of urine is restored, and the person recovers.
CELT urologists have been performing ureteroplasty using laparoscopic access for more than 15 years. This is the most gentle reconstructive surgery that leads to a complete recovery. We have accumulated vast practical experience that allows us to help a huge number of patients.
The operation is performed through punctures, without large incisions. The image is projected onto a large monitor, where all the details are visible. The narrowed, scarred ureter is dissected. A flap is cut out from the tissue of the pelvis, which is sewn into the place of narrowing, and plastic surgery is performed.
Endoscopic ureteroplasty causes minimal damage to the patient. During the operation, a small amount of tissue is dissected, therefore, there are much fewer possible postoperative complications than with open access. The risk of infection is reduced to almost zero. The rehabilitation period lasts no more than a month, most of which the patient spends at home. You only need to spend 2-4 days in the hospital.
CELT urologists try to help all patients who have a similar problem.
What diagnoses are made based on the examination?
Some examples of common diseases accompanied by pyelectasis:
- Hydronephrosis caused by an obstruction (obstruction) in the area of the ureteropelvic junction. It manifests itself as a sharp dilation of the pelvis without dilatation of the ureter.
- Vesicoureteral reflux is the backflow of urine from the bladder into the kidney. It manifests itself as significant changes in the size of the pelvis during ultrasound examinations and even during one examination.
- Megaureter - a sharp dilation of the ureter can accompany pyelectasis. Causes: severe vesicoureteral reflux, narrowing of the ureter in the lower section, high pressure in the bladder, etc.
- Posterior urethral valves in boys . Ultrasound reveals bilateral pyelectasis and dilatation of the ureters.
- Ectopic ureter - The flow of the ureter not into the bladder, but into the urethra in boys or the vagina in girls. Often occurs with double kidneys and is accompanied by pyeelectasis of the upper segment of the double kidney
- Ureterocele - the ureter, when it enters the bladder, is inflated in the form of a bubble, and its outlet is narrowed. Ultrasound reveals an additional cavity in the lumen of the bladder and often pyelectasis on the same side.
Main symptoms
Most patients complain of the following manifestations of hydronephrosis:
- severe pain in the lower back and abdomen, which can radiate to other parts of the body
- increase in body temperature
- weakness
- chills
- the appearance of blood clots in the urine
- headaches and increased blood pressure
- there may be a completely asymptomatic course when the pathology is present from birth and the body has adapted to it
The more advanced the disease, the more pronounced its symptoms become.
The more advanced the disease, the more pronounced its symptoms become.
Important! Body temperature rises when the disease is accompanied by an infection. In this case, it is very important to carry out immediate treatment.
Symptoms of hydronephrosis may also include bloating, constant nausea and severe vomiting, increased fatigue with decreased performance.
In children, signs of the disease include:
- cloudy urine
- reducing the amount of daily urine
- pain
Like adults, children complain of weakness, headaches, and nausea. Parents should pay close attention to the child’s health if he refuses his favorite food, games, walks, becomes lethargic and sleeps a lot.
Competent treatment of kidney hydronephrosis in an adult or child is impossible without a high-quality comprehensive examination.
Types of disease
Hydronephrosis is classified according to three criteria. By origin it is:
- congenital (most typical for children);
- acquired (usually develops against the background of inflammation in the urinary system, etc.).
According to localization, the disease is:
- one-sided;
- double-sided
Depending on the severity, there are three stages of the pathological process:
- first (slight enlargement of the kidney and stretching of the pelvis);
- second (expansion of the pyelocaliceal components, development of the process of parenchymal atrophy, impaired renal function);
- third (severe atrophy of the parenchyma, a greatly enlarged kidney that does not perform its function).
Megaureter
It happens that a child has impaired ureteral emptying from birth, and because of this, over the years he cannot get along with the potty. We are talking about megaureter, i.e. congenital dilatation of the ureter. This problem will eventually lead to kidney complications due to stagnation of urine. This fact is easy to explain - urine is not cleared from the renal pelvis and ureter in a timely manner, microbial flora penetrates the urinary tract and everything turns into pyelonephritis, i.e. chronic inflammation in the kidneys, renal tissues. Also, due to the increased pressure in the pelvis, it reaches a pathological effect on the renal blood flow, the result is that the kidney shrinks a second time, as its tissues are scarred, functionality suffers, i.e. nephrosclerosis occurs. An alarming signal for parents should be a child's complaints of pain in the abdomen or lower back. In principle, this pathology rarely manifests itself until it reaches pyelonephritis. This is indicated by a high temperature, an increased number of leukocytes and protein in the urine, and an increase in ESR in the blood. In this case, acute pyelonephritis will first need to be treated in a hospital setting and only then will it come to urological examinations.
Chronic renal failure
Pathology develops if the acute form is not treated. Chronic renal failure is a condition in which anemia is observed, phosphorus-calcium metabolism is disrupted, and blood pressure increases. The cause of chronic renal failure in children can be poisoning with drugs and heavy metals, untreated infections and diseases of the urinary system:
- pyelonephritis;
- scleroderma;
- arterial stenosis;
- amyloidosis;
- hereditary nephritis;
- tumors, kidney stones.
In children under 3 years of age, the development of the disease is often caused by abnormalities in the development of the urinary tract, heredity, and renal tissue dysplasia.
The causes of chronic renal failure in children over 10 years of age are acquired diseases: organ damage due to tuberculosis, diabetes mellitus. The risk group includes children with intrauterine development disorders and obstructive diseases. Source: T.I. Razdolkina Features of chronic renal failure in children // Difficult Patient, 2013, No. 2-3, v. 11, pp. 16-20
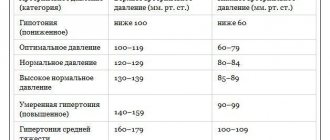
Stages of development of chronic renal failure
- Compensated – no complaints.
- Subcompensated – accompanied by increased thirst, decreased appetite, and disruption of the gastrointestinal tract. CRF manifests itself in growth retardation, severe intestinal infections, dry skin and peeling.
- Decompensated – a noticeable decrease in urine volume. Signs include poor appetite and nausea. In children, curvature of the legs is noticeable.
- Terminal – damage to organs and systems, requiring transplantation or dialysis. Swelling of the face and lower extremities, headaches, lack of appetite, decreased vision, shortness of breath, itchy skin. There is a sharp lag in growth.
Ureterocele
This is an intravesical cyst of the distal ureter. This disease is usually caused by abnormal congenital development of the ureter. Disturbances during the period of fetal formation lead to a thinning of the passage of the ureter in the bladder itself. With ureterocele, the child may at times complain of difficulty urinating, pain in the lumbar region and abdomen, or may behave absolutely calmly until pyelonephritis appears. If there is still a suspicion of a ureterocele, the pediatric urologist will conduct a series of standard studies of the bladder and kidneys, which will explain the cause of what is happening. The patient will undergo intravenous urography (X-ray), and if doubt remains, ultrasound, cystoscopy (internal examination of the bladder through a special optical tube) and cystography (will reveal the presence of VUR). The diagnosed disease is treated primarily surgically, and the type of operation is determined by the condition of the kidney. An alternative method is to create a new orifice in the ureter using an endoscopic instrument.
General information about the disease
On average, one child in one and a half thousand suffers from hydronephrosis; in one fifth of all cases, the disease affects both kidneys. Boys are more susceptible to this disease (it occurs twice as often).
Hydronephrosis is often diagnosed at the stage of intrauterine development, at 20 weeks of pregnancy. In our country, of all pregnancies, in approximately 1% of cases, the fetus is diagnosed with such a congenital disease. The prognosis for it varies, depending on the severity of the anomaly. If the deviations are minor, then it is possible that the fetus will “outgrow” the disease. In case of serious pathologies, either treatment is carried out or it is recommended to terminate the pregnancy.
As for newborns, hydronephrosis is suspected if there is blood in the urine, an enlarged abdomen, or restlessness. Next comes the diagnosis, based on the results of which the diagnosis is confirmed or refuted. The anomaly is usually provoked by dysfunction or obstruction of the muscles in the areas of the walls of the urinary tract and the anterior abdominal wall. Source: S.N. Styazhkina, E.M. Vinokhodova, M.L. Chernenkova, K.A. Karimova, A.N. Khametshina The influence of maternal kidney diseases on the fetus // Bulletin of Science and Education, 2015
Description of pathogenesis
With increased pressure inside the kidneys and dilation of the calyces, the blood vessels are compressed, which increases damage to the parenchyma and reduces glomerular filtration. Urinary infiltrates (accumulations of urine) are formed in the connective renal tissue, and protein accumulates in the affected area. The tissue is reborn into a denser and harder one. Often an infection is added to the process, which accelerates the development of the disease and the death of the parenchyma, blood circulation and lymph flow in the kidney are disrupted. The result of these harmful processes is atrophy of the kidney tissue, that is, the organ ceases to perform its function.
Pyelonephritis in children: classification, course, diagnosis and treatment
Pyelonephritis is a nonspecific infectious and inflammatory disease of the kidneys with predominant damage to the pyelocaliceal system (PSS), tubules and interstitium. According to the World Health Organization (WHO) classification, pyelonephritis belongs to the group of tubulointerstitial nephritis and is actually tubulointerstitial nephritis of infectious origin [1, 2, 6].
Today, the question of the primary and secondary nature of pyelonephritis, especially chronic, as well as the role of urinary tract obstruction in the development of its various variants remains relevant [3, 7]. These signs form the basis for the classification of pyelonephritis.
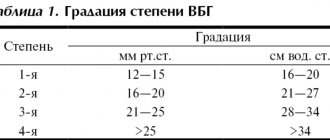
There is no generally accepted classification of pyelonephritis today. The most frequently used classification is proposed by M. Ya. Studenikin and co-authors in 1980 (Table 1), which determines the form (primary, secondary), nature of the course (acute, chronic), disease activity and kidney function. V. G. Maydannik and co-authors (2002) also suggested indicating the stage of the pyelonephritic process (infiltrative, sclerotic) and the degree of disease activity [2, 3, 6, 7, 9].
Primary is called pyelonephritis, in which the examination fails to identify any factors that contribute to the fixation of microorganisms in the kidney tissue, that is, when a microbial inflammatory process develops in an initially healthy organ. Secondary pyelonephritis is caused by specific factors.
In turn, secondary pyelonephritis is divided into obstructive and non-obstructive. Secondary obstructive develops against the background of organic (congenital, hereditary and acquired) or functional disorders of urodynamics; secondary non-obstructive - against the background of dysmetabolic disorders (secondary dysmetabolic pyelonephritis), hemodynamic disorders, immunodeficiency states, endocrine disorders, etc. [2, 3, 6].
The concept of primary or secondary disease undergoes significant changes over time. Clinical and experimental data convincingly indicate that without a preliminary disturbance of urodynamics, the pyelonephritic process practically does not develop. Obstruction of the urinary tract implies not only the presence of a mechanical obstruction to the flow of urine, but also functional disturbances of activity, such as hyper- or hypokinesia, dystonia. From this point of view, primary pyelonephritis no longer implies any absence of disturbance in the passage of urine, since dynamic changes in urination are not excluded [1, 2, 6].
Primary pyelonephritis is quite rare - no more than 10% of all cases, and its share in the structure of the disease decreases as methods for examining the patient improve.
It is also very conditional to classify secondary dismetabolic pyelonephritis as a non-obstructive group, since with this option, obstruction of the renal tubules and collecting ducts by salt crystals is always observed [2, 6].
Acute and chronic pyelonephritis are distinguished depending on the duration of the pathological process and the characteristics of clinical manifestations.
Acute or cyclic course of pyelonephritis is characterized by the transition of the active stage of the disease (fever, leukocyturia, bacteriuria) into a period of reverse development of symptoms with the development of complete clinical and laboratory remission with a duration of the inflammatory process in the kidneys of less than 6 months. The chronic course of pyelonephritis is characterized by the persistence of symptoms of the disease for more than 6 months from its onset or the presence of at least two relapses during this period and, as a rule, is observed with secondary pyelonephritis. According to the nature of the course, latent or recurrent chronic pyelonephritis is distinguished. The recurrent course is characterized by periods of exacerbation, occurring with the clinical picture of acute pyelonephritis (urinary and pain syndromes, symptoms of general intoxication), and remissions. The latent course of the chronic form is characterized only by urinary syndrome of varying severity [2, 3, 7].
As the experience accumulated in the Nephrology Department of the Russian Children's Clinical Hospital shows, chronic pyelonephritis is always secondary and develops most often as an obstructive-dysmetabolic type against the background of dismetabolic nephropathy, neurogenic bladder dysfunction, obstructive uropathy, etc. Among 128 patients with chronic pyelonephritis that we observed during 2004 g., in 60 (46.9%) the disease developed against the background of dysmetabolic nephropathy, in 40 (31.2%) - against the background of neurogenic bladder dysfunction, in 28 (21.9%) - against the background of obstructive uropathies (vesi- ureteral reflux, hydronephrosis, hypoplasia and aplasia of the kidney, horseshoe kidney, lumbar dystopia of the kidney, etc.).
Depending on the severity of the signs of the disease, one can distinguish the active stage of chronic pyelonephritis, partial clinical and laboratory remission and complete clinical and laboratory remission.
The activity of chronic pyelonephritis is determined by a combination of clinical symptoms and changes in urine and blood tests.
Clinical symptoms include:
- fever, chills;
- pain syndrome;
- dysuric phenomena (when combined with cystitis).
Urinalysis indicators are as follows:
- bacteriuria >100,000 microbial bodies in 1 ml;
- leukocyturia > 4000 in urine analysis according to Nechiporenko.
Blood test indicators:
- leukocytosis with rod-nuclear shift;
- anemia;
- increased erythrocyte sedimentation rate (ESR).
Partial clinical and laboratory remission is characterized by the absence of clinical manifestations with persistent urinary syndrome. At the stage of complete clinical and laboratory remission, neither clinical nor laboratory signs of the disease are detected.
With exacerbation of recurrent pyelonephritis, an acute clinical form is observed, although general clinical symptoms are usually less pronounced. During periods of remission, the disease often does not manifest itself at all or only urinary syndrome occurs.
Often, in the chronic form, children experience infectious asthenia: irritability, fatigue, poor performance at school, etc.
Leukocyturia in pyelonephritis is neutrophilic in nature (more than 50% neutrophils). Proteinuria, if present, is insignificant, less than 1 g/l, and correlates with the severity of leukocyturia. Often, children with pyelonephritis have erythrocyturia, usually single unchanged red blood cells.
In the chronic dismetabolic variant, crystalluria is detected in a general urine analysis; in a biochemical urine analysis, increased levels of oxalates, phosphates, urates, cystine, etc.; in a urine analysis for the anti-crystal-forming ability of urine, a decrease in the ability to dissolve the corresponding salts, positive tests for calcification and the presence of peroxides.
Diagnosis of chronic pyelonephritis is based on the protracted course of the disease (more than 6 months), repeated exacerbations, identification of signs of damage to the tubulointerstitium and CLS due to bacterial infection [1, 2, 6, 8].
In any course of the disease, the patient must undergo a full range of studies aimed at establishing the activity of the microbial inflammatory process, the functional state of the kidneys, the presence of signs of obstruction and metabolic disorders, and the state of the renal parenchyma [1, 2, 6]. We offer the following set of studies for chronic pyelonephritis, which allows us to obtain answers to the questions posed.
1. Research to identify the activity of the microbial inflammatory process.
Mandatory laboratory tests:
- Clinical blood test.
- Biochemical blood test (total protein, protein fractions, urea, fibrinogen, C-reactive protein (CRP)).
- General urine analysis.
- Quantitative urine tests (according to Nechiporenko, Amburge, Addis-Kakovsky).
- Morphology of urine sediment.
- Urine culture for flora with quantitative assessment of the degree of bacteriuria.
- Urine antibioticogram.
- Biochemical examination of urine (daily excretion of protein, oxalates, urates, cystine, calcium salts, indicators of membrane instability - peroxides, lipids, anti-crystal-forming ability of urine).
Additional laboratory tests:
- Urine examination for chlamydia, mycoplasma, ureaplasma (polymerase chain reaction, cultural, cytological, serological methods), fungi, viruses, mycobacterium tuberculosis (urine culture, express diagnostics).
- Study of immunological status (secretory immunoglobulin A (sIgA), state of phagocytosis).
2. Studies to assess the functional state of the kidneys and tubular apparatus.
Mandatory laboratory tests:
- Level of creatinine, urea in the blood.
- Zimnitsky's test.
- Clearance of endogenous creatinine.
- Study of pH, titratable acidity, ammonia excretion.
- Diuresis control.
- Rhythm and volume of spontaneous urination.
Additional laboratory tests:
- Urinary excretion of β2-microglobulin (mg).
- Urine osmolarity.
- Urine enzymes.
- Ammonium chloride test.
- Zimnitsky test with dry food.
3. Instrumental research.
Required:
- Blood pressure measurement.
- Ultrasound examination (ultrasound) of the urinary system.
- X-ray contrast studies (void cystography, excretory urography).
- Functional methods for studying the bladder (uroflowmetry, cystometry, profilometry).
Additional:
- Doppler ultrasound of renal blood flow.
- Excretory urography with furosemide test.
- Cystourethroscopy.
- Radionuclide studies (scintigraphy).
- Electroencephalography.
- Echoencephalography.
- CT scan
- Nuclear magnetic resonance.
Thus, the diagnosis of pyelonephritis in children is established based on a combination of the following criteria [6].
- Symptoms of intoxication.
- Pain syndrome.
- Changes in urinary sediment: leukocyturia of the neutrophilic type (more than 50% neutrophils), bacteriuria (more than 100 thousand microbial bodies in 1 ml of urine), proteinuria (less than 1 g/l of protein).
- Violation of the functional state of the kidneys of the tubulointerstitial type: decrease in urine osmolarity less than 800 mOsmol/l with blood osmolarity less than 275 mOsmol/l, decrease in the relative density of urine and indicators of acido- and amoniogenesis, increase in the level of β2-microglobulin in the blood plasma more than 2.5 mg/l and in urine - above 0.2 mg/l.
- Asymmetry of contrasting of the maxillary joint, coarsening and deformation of the arches of the cups, pyelectasis.
- Lengthening of the secretory and excretory segments of renograms, their asymmetry.
Additional criteria may include:
- Increased ESR (more than 15 mm/h).
- Leukocytosis (more than 9Ё109/l) with a shift to the left.
- Increased titers of antibacterial antibodies (1:160 or more), disimmunoglobulinemia, increased number of circulating immune complexes.
- Increased CRP levels (above 20 mcg/ml), hyper-γ- and hyper-α2-globulinemia.
Complications of pyelonephritis are associated with the development of purulent processes and progressive dysfunction of the tubules, leading to the development of chronic renal failure in chronic pyelonephritis.
Complications of pyelonephritis:
- nephrogenic arterial hypertension;
- hydronephrotic transformation;
- pyelonephritic wrinkled kidney, uremia;
- purulent complications (apostematous nephritis, abscesses, paranephritis, urosepsis);
- bacteremic shock.
Pyelonephritis must be differentiated from chronic cystitis, interstitial nephritis, acute glomerulonephritis with isolated urinary syndrome, chronic glomerulonephritis, kidney tuberculosis, etc. Often in pediatric practice, pyelonephritis is diagnosed as an “acute abdomen,” intestinal and respiratory infections, pneumonia, and sepsis.
Treatment of pyelonephritis
Treatment of pyelonephritis involves not only antibacterial, pathogenetic and symptomatic therapy, but also the organization of the correct regimen and nutrition of the sick child.
The issue of hospitalization is decided depending on the severity of the child’s condition, the risk of complications and the social conditions of the family. In the active stage of the disease, in the presence of fever and pain, bed rest is prescribed for 5–7 days.
Dietary restrictions are aimed at reducing the load on the tubular transport systems and correcting metabolic disorders. In the active stage, table No. 5 according to Pevzner is used without salt restriction, but with an increased drinking regime, 50% more than the age norm. The amount of salt and liquid is limited only if kidney function is impaired. It is recommended to alternate protein and plant foods. Products containing extractives and essential oils, fried, spicy, fatty foods are excluded. Detected metabolic disorders require special corrective diets.
The basis of drug treatment of pyelonephritis is antibacterial therapy, which is based on the following principles [6]:
- Before starting treatment, a urine culture is necessary (later treatment is changed based on the culture results);
- exclude and, if possible, eliminate factors contributing to infection;
- improvement of the condition does not mean the disappearance of bacteriuria;
- treatment results are regarded as failure if there is no improvement and/or persistence of bacteriuria;
- primary lower urinary tract infections usually respond to short courses of antimicrobial therapy; upper urinary tract - require long-term therapy;
- early relapses (up to 2 weeks) represent a recurrent infection and are caused either by the survival of the pathogen in the upper urinary tract or by ongoing seeding from the intestine. Late relapses are almost always re-infection;
- pathogens of community-acquired urinary tract infections are usually sensitive to antibiotics;
- frequent relapses, instrumental interventions on the urinary tract, recent hospitalization make one suspect an infection caused by resistant pathogens.
Therapy for pyelonephritis includes several stages: 1) suppression of the active microbial inflammatory process using an etiological approach; 2) pathogenetic treatment against the background of subsiding of the process using antioxidant protection and immunocorrection; 3) anti-relapse treatment. Therapy for acute pyelonephritis, as a rule, is limited to the first two stages; for chronic pyelonephritis, all three stages of treatment are necessary [6].
The stage of suppressing the activity of the microbial inflammatory process. Conventionally, this stage can be divided into two periods.
The first is aimed at eliminating the pathogen before obtaining urine culture results and includes the appointment of initial (empirical) antibacterial therapy, diuretic therapy (for non-obstructive variants), infusion-corrective therapy for severe endogenous intoxication syndrome and hemodynamic disorders.
The second (etiotropic) period consists of correcting antibacterial therapy taking into account the results of urine culture and determining the sensitivity of the microorganism to antibiotics.
When choosing antibacterial drugs, it is necessary to consider that:
- the drug must be active against the most common pathogens of urinary tract infections;
- must not be nephrotoxic;
- should create high concentrations at the site of inflammation (urine, interstitium);
- should have a predominantly bactericidal effect;
- must be active at the pH values of the patient’s urine (Table 2);
- when combining several drugs, synergism should be observed [5, 6].
The duration of antibacterial therapy should be optimal, ensuring complete suppression of pathogen activity. Thus, its duration is usually about 4 weeks in the hospital with a change of antibiotic every 7-10 days (or replacement with a uroseptic).
Initial antibiotic therapy is prescribed empirically, based on the most likely causative agents of infection. If there is no clinical and laboratory effect, the antibiotic must be changed after 2–3 days.
In case of manifest severe and moderate pyelonephritis, drugs are administered mainly parenterally (intravenously or intramuscularly) in a hospital setting.
We list some antibiotics used in the initial treatment of pyelonephritis:
- semisynthetic penicillins in combination with β-lactomase inhibitors - amoxicillin and clavulanic acid: augmentin - 25-50 mg/kg/day, orally - 10-14 days; amoxiclav - 20-40 mc/kg/day, orally - 10-14 days;
- 2nd generation cephalosporins: cefuroxime (zinacef, ketocef, cefurabol), cefamandol (mandol, cefamabol) - 80-160 mg/kg/day, intravenously, intramuscularly - 4 times a day - 7-10 days;
- 3rd generation cephalosporins: cefotaxime (claforan, clafobrine), ceftazidime (Fortum, Vicef), ceftizoxime (epocelin) - 75-200 mg/kg/day, intravenously, intramuscularly - 3-4 times a day - 7-10 days; cefoperazone (cephobid, cefoperabol), ceftriaxone (rocephin, ceftriabol) - 50-100 mg/kg/day, intravenously, intramuscularly - 2 times a day - 7-10 days;
- aminoglycosides: gentamicin (gentamicin sulfate) - 3.0-7.5 mg/kg/day, intravenously, intramuscularly - 3 times a day - 5-7 days; amikacin (amicin, lykacin) - 15-30 mg/kg/day, intravenously, intramuscularly - 2 times a day - 5-7 days.
During the period of subsidence of activity, antibacterial drugs are administered mainly orally, while “step therapy” is possible, when the same drug that was administered parenterally or a drug of the same group is given orally [5]. The most commonly used during this period are:
- semisynthetic penicillins in combination with β-lactomase inhibitors: amoxicillin and clavulanic acid (Augmentin, amoxiclav);
- 2nd generation cephalosporins: cefaclor (Ceclor, Vercef) - 20–40 mg/kg/day;
- 3rd generation cephalosporins: ceftibuten (cedex) - 9 mg/kg/day, once;
- nitrofuran derivatives: nitrofurantoin (furadonin) - 5–7 mg/kg/day;
- quinolone derivatives (non-fluorinated): nalidixic acid (negram, nevigramon) - 60 mg/kg/day; pipemidic acid (palin, pimidel) - 0.4–0.8 g/day; nitroxoline (5-NOK, 5-nitrox) - 10 mg/kg/day;
- sulfamethoxazole and trimethoprim (cotrimoxazole, biseptol) - 4-6 mg/kg/day for trimethoprim.
In severe septic conditions, microbial associations, multiresistance of microflora to antibiotics, when affecting intracellular microorganisms, as well as to expand the spectrum of antimicrobial action in the absence of culture results, combination antibacterial therapy is used. In this case, bactericidal antibiotics are combined with bactericidal, bacteriostatic with bacteriostatic antibiotics. Some antibiotics are bactericidal against some microorganisms and bacteriostatic against others.
Bactericidal drugs include: penicillins, cephalosporins, aminoglycosides, polymyxins, etc.
Bacteriostatic drugs include: macrolides, tetracyclines, chloramphenicol, lincomycin, etc.
Potentiate the action of each other (synergists): penicillins and aminoglycosides; cephalosporins and penicillins; cephalosporins and aminoglycosides.
Antagonists are: penicillins and chloramphenicol; penicillins and tetracyclines; macrolides and chloramphenicol.
From the point of view of nephrotoxicity, erythromycin, drugs of the penicillin group and cephalosporins are non-toxic or low-toxic; moderately toxic - gentamicin, tetracycline, etc.; Kanamycin, monomycin, polymyxin, etc. have pronounced nephrotoxicity.
Risk factors for nephrotoxicity of aminoglycosides are: duration of use for more than 11 days, maximum concentration above 10 μg/ml, combination with cephalosporins, liver disease, high creatinine levels [6].
After a course of antibiotic therapy, treatment should be continued with uroantiseptics.
Nalidixic acid preparations (nevigramon, negram) are prescribed to children over 2 years of age. These agents are bacteriostatics or bactericides, depending on the dose, against gram-negative flora. They should not be prescribed simultaneously with nitrofurans, which have an antagonistic effect. The course of treatment is 7–10 days.
Gramurin, a derivative of oxolinic acid, has a wide spectrum of action on gram-negative and gram-positive microorganisms. It is used in children aged 2 years and over for a course of 7–10 days.
Pipemidic acid (palin, pimidel) has an effect on most gram-negative bacteria and staphylococci. Prescribed in a short course (3–7 days).
Nitroxoline (5-NOK) and nitrofurans are drugs with broad bactericidal action.
The reserve drug is ofloxacin (Tarivid, Zanocin). It has a wide spectrum of action, including on intracellular flora. It is prescribed to children only if other uroseptics are ineffective.
The use of biseptol is possible only as an anti-relapse agent in the latent course of pyelonephritis and in the absence of obstruction in the urinary tract.
In the first days of the disease, against the background of increased water load, fast-acting diuretics (furosemide, veroshpiron) are used, which increase renal blood flow, ensure the elimination of microorganisms and inflammatory products and reduce swelling of the interstitial tissue of the kidneys. The composition and volume of infusion therapy depend on the severity of the intoxication syndrome, the patient's condition, hemostasis, diuresis and other kidney functions.
The stage of pathogenetic therapy begins when the microbial inflammatory process subsides against the background of antibacterial drugs. On average, this occurs on the 5–7th day from the onset of the disease. Pathogenetic therapy includes anti-inflammatory, antioxidant, immunocorrective and anti-sclerotic therapy [6].
A combination with anti-inflammatory drugs is used to suppress inflammatory activity and enhance the effect of antibacterial therapy. It is recommended to take non-steroidal anti-inflammatory drugs - ortofen, voltaren, surgam. The course of treatment is 10–14 days. The use of indomethacin in pediatric practice is not recommended due to a possible deterioration in the blood supply to the kidneys, decreased glomerular filtration, water and electrolyte retention, and necrosis of the renal papillae.
Desensitizing agents (tavegil, suprastin, claritin, etc.) are prescribed for acute or chronic pyelonephritis in order to relieve the allergic component of the infectious process, as well as when the patient develops sensitization to bacterial antigens.
The complex therapy for pyelonephritis includes drugs with antioxidant and antiradical activity: tocopherol acetate (1–2 mg/kg/day for 4 weeks), unithiol (0.1 mg/kg/day intramuscularly once, for 7–10 days), b-carotene (1 drop per year of life, 1 time per day for 4 weeks), etc. Among the drugs that improve kidney microcirculation, trental, cinnarizine, and aminophylline are prescribed.
Immunocorrective therapy for pyelonephritis is prescribed strictly according to indications [4]:
- infancy;
- severe variants of kidney damage (purulent lesions; aggravated by multiple organ failure syndrome; obstructive pyelonephritis against the background of reflux, hydronephrosis, megaureter, etc.);
- long-term (more than 1 month) or recurrent course;
- intolerance to antibiotics;
- features of the microflora (mixed flora; flora multiresistant to antibiotics; unusual nature of the flora - Proteus, Pseudomonas, Enterobacter, etc.).
The prescription of immunocorrective therapy is made only after agreement with an immunologist and should include immunological monitoring, relative “selectivity” of the prescription, a short or intermittent course and strict adherence to the dosage and regimen of drug administration.
Immunal, sodium nucleate, t-activin, levamisole hydrochloride, lycopid, immunofan, reaferon, leukinferon, viferon, cycloferon, myelopid, lysozyme are used as immunotropic agents for pyelonephritis and urinary tract infections in children.
If patients have signs of sclerosis of the renal parenchyma, it is necessary to include in the treatment complex drugs that have an anti-sclerotic effect (delagil) for a course of 4-6 weeks.
During the period of remission, a necessary continuation of treatment is herbal medicine (collections of St. John's wort, lingonberry leaves, nettles, corn silk, bearberry, rose hips, birch buds, yarrow, sage, chamomile in combinations).
Anti-relapse therapy for pyelonephritis involves long-term treatment with antibacterial drugs in small doses and is carried out, as a rule, in an outpatient setting.
For this purpose, use: biseptol at the rate of 2 mg/kg for trimethoprim and 10 mg/kg for sulfamethoxazole 1 time per day for 4 weeks (use with caution in case of obstructive pyelonephritis); furagin at the rate of 6–8 mg/kg for 2 weeks, then if urine tests are normal, switch to 1/2–1/3 doses for 4–8 weeks; prescribing one of the drugs pipemidic acid, nalidixic acid or 8-hydroxyquinoline every month for 10 days in usual dosages for 3–4 months.
For the treatment of frequently recurrent pyelonephritis, a “duplicate” regimen can be used: nitroxoline at a dose of 2 mg/kg in the morning and biseptol at a dose of 2–10 mg/kg in the evening.
At any stage of treatment of secondary pyelonephritis, it is necessary to take into account its nature and the functional state of the kidneys. Treatment of obstructive pyelonephritis should be carried out jointly with a urologist and pediatric surgeon. In this case, the decision to prescribe diuretics and increase the water load should be made taking into account the nature of the obstruction. The issue of surgical treatment must be resolved in a timely manner, since in the presence of obstruction of urine flow at any level of the urinary system, the prerequisites for the development of relapse of the disease remain.
The treatment of dysmetabolic pyelonephritis should include an appropriate dietary regimen and pharmacological treatment.
With the development of renal failure, it is necessary to adjust the doses of medications in accordance with the degree of decrease in glomerular filtration.
Dynamic observation of children suffering from pyelonephritis suggests the following [6, 9].
- Frequency of examination by a nephrologist: during exacerbation - once every 10 days; during remission during treatment - once a month; remission after completion of treatment for the first 3 years - once every 3 months; remission in subsequent years until the age of 15 years - 1-2 times a year, then observation is transferred to therapists.
- Clinical and laboratory tests: general urine analysis - at least once every 1 month and against the background of acute respiratory viral infections; biochemical urine analysis - once every 3-6 months; Ultrasound of the kidneys - once every 6 months. According to indications - cystoscopy, cystography and intravenous urography.
Removal from the dispensary register of a child who has suffered acute pyelonephritis is possible if clinical and laboratory remission is maintained without therapeutic measures (antibiotics and uroseptics) for more than 5 years after a full clinical and laboratory examination. Patients with chronic pyelonephritis are observed before transfer to the adult network.
Literature
- Borisov I. A. Pyelonephritis//In the book. "Nephrology" / ed. I. E. Tareeva. M.: Medicine, 2000. pp. 383–399.
- Vozianov A.F., Maydannik V.G., Bidny V.G., Bagdasarova I.V. Fundamentals of childhood nephrology. Kyiv: Book Plus, 2002. pp. 22–100.
- Ignatova M. S., Veltishchev Yu. E. Pediatric nephrology. L.: Medicine, 1989. 432 p.
- Kirillov V.I. Immunocorrective therapy of urinary system infections in children//In the book. "Nephrology" / ed. M. S. Ignatova: a guide to pharmacotherapy in pediatrics and pediatric surgery (edited by A. D. Tsaregorodtsev, V. A. Tabolin). M.: Medpraktika-M, 2003. T. 3. P. 171–179.
- Korovina N. A., Zakharova I. N., Mumladze E. B., Zaplatnikov A. L. Rational choice of antimicrobial therapy for urinary system infections in children // In the book. "Nephrology" / ed. M. S. Ignatova: a guide to pharmacotherapy in pediatrics and pediatric surgery (edited by A. D. Tsaregorodtsev, V. A. Tabolin). M.: Medpraktika-M, 2003. T. 3. P. 119–170.
- Malkoch A.V., Kovalenko A.A. Pyelonephritis//In the book. “Childhood Nephrology” / ed. V. A. Tabolina et al.: a practical guide to childhood diseases (edited by V. F. Kokolina, A. G. Rumyantsev). M.: Medpraktika, 2005. T. 6. P. 250–282.
- Papayan A.V., Savenkova N.D. Clinical nephrology of childhood: a guide for doctors. St. Petersburg, 1997, pp. 450–501.
- Tebloeva L. T., Kirillov V. I., Diagnosis of urinary tract infections in children: materials of the 1st Congress “Modern methods of diagnosis and treatment of nephro-urological diseases in children.” M., 1998. pp. 57–60.
- Erman M.V. Nephrology of childhood in diagrams and tables. St. Petersburg: Special literature, 1997. pp. 216–253.
A. V. Malkoch , Candidate of Medical Sciences V. A. Gavrilova , Doctor of Medical Sciences Yu. B. Yurasova , Candidate of Medical Sciences Russian State Medical University, Russian Children's Clinical Hospital, Moscow
Consequences and complications
If diagnosis is not made in a timely manner and treatment is incorrect, serious complications can occur. The development of the disease leads to a reduction in renal function, disruption of systems and organs, poisoning by metabolic products, and irreversible consequences.
Among the dangerous complications:
- risk of cardiac arrest;
- dysfunction of several body systems;
- blood poisoning;
- uremia.
If there is a pathology, the child is developmentally delayed, does not fit into the team well, and has difficulties in developing speech.