general characteristics
CECs are complexes consisting of antigen, antibodies and associated complement components C3, C4, C1q. Normally, immune complexes formed in the bloodstream are phagocytosed and destroyed by both phagocytes and the liver. However, with an increase in their size (with an excess of antigen and the presence of IgM and the C1q component of complement in their structure), the complexes can be deposited in the perivascular space and the renal cortex, causing activation of complement and inflammatory processes. More often, immune complexes are deposited in the endothelium of blood vessels, renal glomeruli, and joints, which, accordingly, manifests itself in clinical signs of vasculitis, glomerulonephritis, and arthritis. The pathogenesis of autoimmune diseases is closely related to the accumulation of immune complexes in tissues.
Immune system cells
Leukocytes . Their purpose is to recognize foreign substances and microorganisms, fight them, and also remember information about them. There are several types of leukocytes: - lymphocytes: B-lymphocytes get their name from the Latin word “bursa” - bursa (named after the bursa of Fabricius - the organ in which B-lymphocytes mature in birds. In humans, this process occurs in the bone marrow). This type of lymphocyte produces antibodies (immunoglobulins). T lymphocytes control the work of B lymphocytes, that is, the production of antibodies. They got their name from the word “thymus” - the organ in which their maturation occurs. ٭The thymus is the same as the thymus gland. T-helpers are a type of T-lymphocytes that help synthesize antibodies (to help). T-suppressors are a type of T-lymphocytes that suppress the synthesis of antibodies (to suppress, suppress, restrain, prohibit). — natural killer cells (NK) are lymphocyte-like cells that lack the characteristics of T- and B-lymphocytes. They are able to destroy tumor cells and cells infected with viruses; - neutrophilic leukocytes (band-nucleus: the nucleus looks like curved rods; segmented: the nuclei are segmented, have constrictions); - eosinophilic leukocytes; - basophilic leukocytes. Neutrophils, eosinophils and basophils are types of leukocytes, but these cells do not perceive dyes in the same way, which is why they have different names. Eosinophils are involved in the destruction of parasites (they secrete special enzymes that have a damaging effect on them), as well as in allergic reactions (they secrete substances that destroy histamine, preventing the release of enzymes from mast cell granules). Neutrophils are sometimes called "microphagocytes", referring to their ability to phagocytose microorganisms. Macrophages, or phagocytes, “eat” living and dead microbes, antigen-antibody complexes (formed in the process of fighting viruses, bacteria and their toxins), dead cells of the body itself. Without these cells, the activity of lymphocytes is impossible, since they are the ones who “help” the latter recognize antigens and secrete mediators (substances that stimulate or inhibit the activity of other cells of the immune system). The average number of microbes engulfed by one phagocytic cell is called the phagocytic number, and the percentage of phagocytic macrophages is called the phagocytic index. On the surface of cells there are antigens - unique markers (labels) that distinguish some cells from others. These are called clusters of differentiation (CDs). What marks are on the surface of the cell depends on its type (T-lymphocyte, B-lymphocyte, etc.) and its maturity (ability to perform its functions). Labels are numbered in turn, according to when they were opened: the earlier the cluster was opened, the lower its number. In laboratories, clusters of differentiation are detected using monoclonal antibodies. ٭A clone is a collection of cells arising from one common cell. The clone cells are 100% identical. Identical cells synthesize identical antibodies, which are called monoclonal.
The most common types of clusters are: CD2 - cluster of T-lymphocytes, NK-cells; CD3 - T-lymphocyte cluster; CD4 - T-helper cluster; CD8 – T-suppressor cluster; CD16 – cluster of NK cells (natural killer cells); CD20 is a cluster of B cells. Immunoglobulin testing provides information about the state of the humoral immune system. This is used in the diagnosis of primary and secondary immunodeficiencies, autoimmune, infectious, hematological and other diseases. Changes in immunological parameters can be a manifestation of the body’s normal reaction to the influence of physiological or pathological factors (with different patterns of changes at different stages of the disease), reflect excessive activation, depletion of the immune system, or characterize a congenital or acquired defect of individual parts of the immune system.
There are four types of immunoglobulins: IgM - this type of antibody appears first upon contact with an antigen (microbe). An increase in their titer, or content in the blood, indicates an acute inflammatory process. IgG - antibodies of this class appear some time after contact with the antigen. They participate in the fight against microbes: they bind to antigens on the surface of the bacterial cell; then other plasma proteins (the so-called complement) join them, as a result of which the bacterial cell is lysed (its membrane ruptures). In addition, IgG is involved in some allergic reactions. IgA prevents the penetration of microorganisms through mucous membranes. IgE - antibodies of this class interact with receptors located on mast cells (connective tissue cells that secrete physiologically active substances: heparin, histamine, serotonin, etc. They are involved in the processes of inflammation, blood clotting, etc.) and basophils. As a result, histamine and other allergy mediators are released. An allergic reaction itself develops. One of the most important indicators of immune status is complement components C3, C 4. Complement is the set of immune proteins contained in fresh blood serum. They participate in the bactericidal action of blood. C3 is a central component of the complement system, an acute phase protein of inflammation. This is an essential part of the defense system against infections. It is formed in the liver, macrophages, fibroblasts, lymphoid tissue and skin. Therefore, disruption of their normal state significantly affects this component. C4 is a glycoprotein synthesized in the lungs and bone tissue. C4 supports phagocytosis, increases the permeability of the vascular wall, and is involved in the neutralization of viruses. This test is usually prescribed for suspected autoimmune disorders, repeated bacterial infections; during dynamic observation of patients with systemic autoimmune diseases; in the diagnosis of systemic lupus erythematosus, rheumatoid vasculitis and other diseases. Another indicator of immune status is cryoglobulin, an abnormal protein that can be present in the blood in a number of diseases. At low temperatures, cryoglobulins become insoluble, leading to blockage of small blood vessels located in the fingers and toes in cold weather, causing the characteristic rash. The presence of cryoglobulins (cryoglobulinemia) can be a symptom of various diseases, including macroglobulinemia, systemic lupus erythematosus, as well as a number of infectious diseases. Interferons are a special group of proteins that are produced by cells of the human immune system. They are a type of weapon with which the body can resist pathogenic bacteria, parasites and even cancer cells. There are three main classes of interferons: interferon alpha (α), interferon beta (β), interferon gamma (γ), and interferon omega (ω). All of them not only have antiviral and antitumor effects, but also have the property of activating - forcing other protective factors - macrophages and natural killer cells - to act. All types of interferon have a very strong influence on the course of RNA viral infections. In most cases, interferon production is provoked by the penetration of bacteria, viruses or their metabolic products into the body.
Clinical relevance
Pathological reactions to immune complexes can be caused by an increase in the rate of their formation above the rate of elimination, a deficiency of one or more complement components, or functional defects of the phagocytic system. Determining the level of immune complexes in blood serum is important in the diagnosis of acute inflammatory processes in the body and is an indicator of the activity of autoimmune diseases, type III allergic reactions, in which the level of CEC increases, as well as in assessing the effectiveness of treatment.
CIC – circulating immune complexes
It has been established that circulating immune complexes are formed after each meeting of an antigen with an antibody and are destroyed by the efforts of mononuclear phagocytes upon completion of complement activation.
If there is an excess of viral antigens, the antibody loses its ability to neutralize the virus, and instead it forms circulating immune complexes that settle in the kidneys or blood vessels of other organs, causing inflammatory processes there. The consequence of this is tissue damage and the occurrence of systemic diseases such as vasculitis, glomerulonephritis, etc.
In the case of an autoimmune disease or long-term infection, the persistence of the antigen can provoke an immune complex disease. Complement deficiency leads to the formation of large, poorly soluble complexes during complications in their tissues. Positively charged antigens bind to tissues, primarily the glomeruli, which contributes to the local accumulation of CEC in the kidneys. Due to factors that increase vascular permeability, the number of immune complexes in tissues increases.
Circulating immune complexes residing in the blood are in direct contact with erythrocytes, and are also present in free form in plasma. CECs associated with erythrocytes do not often have a damaging effect, which is why the issue of determining the levels of free circulating immune complexes has attracted more attention.
There is also a practice of determining CECs using their affinity for complement components C3d and C1g, using C3d and C1g located in the solid phase.
A decrease in indicators is noted in cases of knockout of the gene responsible for the synthesis of the complement system protein. Increased in cases of autoimmune, systemic or allergic diseases, with vasculitis.
The direct involvement of circulating immune complexes in the development of inflammatory processes has been irrefutably proven, primarily for cases of systemic lupus erythematosus. In addition, this indicator is usually taken into account in rheumatology, since its level is elevated in cases of immunopathological diseases. Based on the level of circulating immune complexes, the activity of immune inflammation and the effectiveness of treatment are determined. The level of CEC increases in systemic vasculitis, diffuse connective tissue diseases, HIV infection, subacute infective endocarditis, autoimmune hepatitis, Crohn's disease, etc.
An increased content of circulating immune complexes in patients with rheumatoid arthritis warns of the development of a systemic rheumatic process. When determining the level of CEC, selective precipitation with polyethylene glycol is most often used. In addition, taking into account the heterogeneity of circulating immune complexes, it is recommended to use several detection methods, the best of which is considered to be the method of binding the Clq component of complement to the CEC. When analyzing the results obtained during the determination of both immunoglobulins and circulating immune complexes, it is necessary to take into account only a multiple - 2-3 or more times increase in their content.
The formation of circulating immune complexes is a physiological defense mechanism that results in the rapid elimination of both endogenous and exogenous antigens (viruses, microorganisms, plant antigens, parasites, fungal, food or pollen antigens) through the reticuloendothelial system.
An increase in the level of circulating immune complexes in various biological fluids, for example, in serum, is observed in all kinds of malignant and inflammatory diseases, which can lead to pathology. The most important indicator in assessing disease activity, especially in autoimmune diseases, is the determination of circulating immune complexes in serum. This definition is based on the ability of CEC to bind to C1q complement components, which are sorbed in the microplate cell.
Ask a question, write a review
Maria 2020-02-17 06:24:23
Hello! I took the Central Election Commission with a result of 0.022, what does this mean?
Korobkova Elena Vladimirovna Obstetrician-gynecologist answers:
Good afternoon. a value of 0-0.025 g/l is the norm. Thank you.
Oksana 2018-03-23 12:31:05
Tell me, what does the indicator CEC = 69 USD mean??
Irina 2017-10-13 20:57:44
After 2 years of treatment for autoimmune hepatitis, the CEC indicators are 1.8 with a reference interval of 0.0-20.0. What can this mean?
Bagaeva Madina Dermatovenerologist, member of the Moscow Society of Dermatovenerologists and Cosmetologists named after. A.I. Pospelova answers:
Hello! You need to see all the analyzes over time...
Galina 2017-08-15 14:07:27
Good afternoon. Central Election Commission-81. What does that mean?
Korobkova Elena Vladimirovna Obstetrician-gynecologist answers:
Good afternoon For what disease were you tested? Thank you.
Maxim 2017-07-08 18:49:10
CEC 200 what does this mean?! Thank you
Korobkova Elena Vladimirovna Obstetrician-gynecologist answers:
Good afternoon This means the presence of inflammatory processes in the body. Thank you.
Anna 2017-06-03 23:18:03
Hello, cycle 30 when the norm is 0-120, what does this mean? Thank you
Korobkova Elena Vladimirovna Obstetrician-gynecologist answers:
Good afternoon Circulating immune complexes (CIC) are evidence of the presence of various inflammatory processes in the human body.
Vera 2017-05-22 12:49:32
A young man I know has been diagnosed with Guillain-Barré syndrome. After the fifth plasmapheresis, the CEC in the blood was 500, although his health improved significantly. The doctors sent the patient home, assuring his mother that the CEC would fall on its own. How can a blood test improve in this case? Thank you!
Korobkova Elena Vladimirovna Obstetrician-gynecologist answers:
Good afternoon Blood tests improve as you recover. Thank you.
Sonya 2017-05-12 17:00:35
CEC 159., diagnosis of rheumatoid arthritis, is this normal?
Korobkova Elena Vladimirovna Obstetrician-gynecologist answers:
Good afternoon CECs are not normally detected in healthy people. For prognostic data regarding rheumatoid arthritis, it is necessary to see the dynamics of the CEC indicator. Thank you.
Valeria 2017-05-05 14:29:04
TsIK-0.10, constant cystitis that does not end, everywhere in urine cultures, throat, smear on flora, cervical canal staphylococcus, antibiotics do not help, no matter how many of them I took, there is also an allergy in the form of rhinitis, sneezing and nasal congestion, aquamaris was prescribed , loratadine, it became a little better, the doctor says that maybe I need to inject anti-staphylococcal immunoglobulin, I don’t know what to do, so much money has already been spent...
Korobkova Elena Vladimirovna Obstetrician-gynecologist answers:
Good afternoon The correct treatment tactics can only be agreed upon with your attending physician. Thank you.
Natalia 2017-04-28 14:58:32
Is CEC 3.69 the norm?
Interpretation:
- An increase in the level of CEC in the blood is characteristic of: • Acute bacterial, fungal, parasitic and viral infections. • Autoimmune diseases, collagenosis, rheumatism, glomerulonephritis, allergic alveolitis, vasculitis, Arthus phenomenon. • Immune complex diseases, serum sickness. • Allergic reactions of the 3rd type.
- A decrease in the level of CEC during the disease or during treatment indicates the extinction of the inflammatory process and the effectiveness of therapy.
Sample result (PDF)
Lymphocytes, immunophenotyping
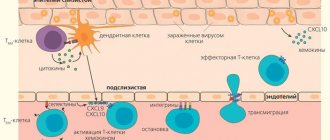
There are different populations of lymphocytes that play a key role in directing the immune response - cellular or humoral. Determination of the immune phenotype of a lymphocyte is possible in a special study using flow cytometry. The phenotype of lymphocytes depends on special receptors on their surface - CD differentiation clusters. The presence of one or another receptor indicates that the cell belongs to a certain population of lymphocytes.
Cellular immunity is determined:
- B lymphocytes (CD19+)
- T-lymphocytes (CD3+) common and their subtypes:
- T helper cells (CD3+CD4+)
- T-cytotoxic (CD3+CD8+)
- T-killer cells (CD3+CD16+CD56+)
- Natural killer cells (CD3-CD16+CD56+)
- Lymphocytes with HLA-DR+ marker
- Immunoregulatory index (T-helpers/T-cytotoxic)
Additionally, other lymphocyte CD markers are examined to determine their activity.
Evaluation of the result is possible only in conjunction with data from the clinical picture and immunomodulatory therapy. Immunophenotyping of lymphocytes is usually carried out over time. Thus, in HIV infection that affects T-helper cells, a decrease in the level of CD3+CD4+ cells and the immunoregulatory index (CD3+CD4+/CD3+CD8+) has a poor prognosis for the course of the disease.
Immunoglobulins A, M, G, E
Total immunoglobulins are indicators of the humoral immune response. IgM levels increase during the acute period of the disease and during exacerbation of chronic infection, IgG - during the recovery process, IgA - during the acute period of the disease, persisting longer than IgM, reflecting a protracted course and damage to the mucous membranes. Elevated IgE levels indicate allergic inflammation.
General immunoglobulins do not explain the cause of infection, so it is advisable to look at specific antibodies to specific pathogens. The main indications for determining total antibodies are suspicion of congenital immunodeficiency associated with humoral immunity.
Total immunoglobulin E, immunoglobulin G, immunoglobulin M, immunoglobulin A are examined.