Table of contents
- Etiology and pathogenesis
- Clinical manifestations
- Treatment methods
- Medicinal methods
- Surgical methods
- Hardware methods
Hemangioma (capillary hemangioma, capillary hemangioma) is a benign tumor that develops from hyperplastic vascular endothelium. It is often absent at birth, but appears in childhood and is characterized by progressive growth.
In our company you can purchase the following equipment for removing hemangiomas:
- M22 (Lumenis)
- AcuPulse (Lumenis)
- Fraxel (Solta Medical)
- UltraPulse (Lumenis)
A feature of hemangiomas is the possibility of spontaneous involution, therefore the treatment tactics for these neoplasms are selected individually for each patient, based on the current state of the tumor and its dynamics. Spontaneous regression distinguishes hemangiomas from other vascular malformations, such as port-wine stains.
According to statistics, capillary hemangiomas occur in 1–2% of newborns, with about 50% of neoplasms forming on the head (often in the eye area) and neck. 30% of patients say that their parents or doctors recorded signs of hemangioma immediately after birth, but the majority note the onset of manifestation of this neoplasm at the age of 6 months. The ratio of men to women in the incidence of hemangioma is 1:3.
Zolotov Sergey Alexandrovich
- Candidate of Medical Sciences, surgeon, specialist in laser surgery.
- From 2003 to 2009 completed training at the State Budgetary Educational Institution of Higher Professional Education "Russian National Research Medical University" named after. N.I.Pirogov Ministry of Health of Russia.
- From 2009 to 2011, he completed his residency at the Moscow State Budgetary Healthcare Institution, Research Institute of Emergency Pediatric Surgery and Traumatology, specializing in Pediatric Surgery.
- In 2011, he completed training under the program of additional professional education of doctors in laser medicine at the State Scientific Center for Laser Medicine of the Federal Medical and Biological Agency of Russia. From 2011 to 2014, he studied full-time graduate school at the Moscow State Budgetary Healthcare Institution Research Institute of Emergency Pediatric Surgery and Traumatology.
He has extensive experience in removing various benign formations of the skin and subcutaneous tissue using laser surgical methods.
More than 5 years of experience in surgery.
Etiology and pathogenesis of capillary hemangiomas
Today, it is believed that capillary hemangioma is a hamartomatous proliferation (i.e., a nodular benign tumor-like formation representing a tissue developmental abnormality) of vascular endothelial cells. To date, no specific gene mutations or obvious hereditary characteristics have been found that would be 100% responsible for the appearance of hemangiomas.
In its development, hemangioma goes through 2 phases - proliferative and involutive. The proliferative phase usually begins 8–18 months after tumor manifestation and is characterized by progressive growth of the tumor. Histologically, it is characterized by an increase in the number of endothelial and mast cells, the latter stimulating further vascular growth.
The proliferative phase gives way to the involutive phase , which is characterized by gradual regression of the hemangioma. It exhibits a reduction in angiogenesis, apoptosis of endothelial cells, a decrease in the activity of mast cells and dilation of vascular channels. About 50% of all neoplasms undergo involution before the age of 5 years, and about 75% - before the age of 7 years.
Causes
To date, scientists cannot name the exact cause of hemangioma, but there are many assumptions about this. One of the theories for the occurrence of this tumor in humans is considered to be a viral-infectious factor that occurs in the first 12 weeks of pregnancy. It is during this period of intrauterine development that the formation and establishment of a system of blood vessels occurs, and the influence of infection can change their properties, which subsequently leads to the formation of intraorganic or superficial hemangiomas.
Clinical manifestations
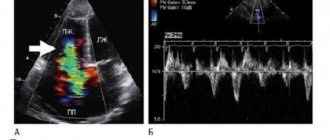
A simple hemangioma is a red, bumpy neoplasm that rises above the surface of the surrounding healthy skin ( Fig. 1 ). Cavernous hemangioma is located in the subcutaneous fatty tissue and looks like a bluish tumor ( Fig. 2 ). Combined hemangioma is located both on the surface and inside the skin. There are also mixed hemangiomas , which are combined with lipomas, fibromas, keratomas and other neoplasms.
An important differential feature of hemangiomas is blanching when pressed - this distinguishes them from port-wine stains.
Rice. 1. Simple capillary hemangioma
https://www.danderm-pdv.is.kkh.dk/atlas/7-65.html
Rice. 2. Cavernous hemangioma
https://www.danderm-pdv.is.kkh.dk/atlas/7-69-2.html
Depending on the location, hemangioma can cause various complications. Thus, a periobrital tumor in 43–60% of cases provokes amblyopia - “switching off” the affected eye from the visual process. Located in the larynx, the tumor can cause stridor and airway obstruction. In general, despite the benign nature of hemangiomas, about 10% of them are destructive in nature, causing serious aesthetic defects.
Price list for medical services of the laser surgery department
Consultation
| Name | Cost in rub. |
| Initial consultation | 2 000 |
Research
| Name | Cost in rub. |
| Cytological examination | 500 |
| Histological examination | 2 800 |
Anesthesia
| Name | Cost in rub. |
| Application anesthesia | 500 |
| Infiltration anesthesia | 500 |
| Conduction anesthesia | 1 500 |
Bandages
| Name | Cost in rub. |
| Adhesive bandage | 300 |
| Aseptic dressing | 500 |
| Bandage with medicines | 1 000 |
Removal of formations using laser radiation
| Anatomical zone | Cost in rub. for 1mm in maximum diameter |
| Scalp | 500 |
| Hands, forearms, feet, legs | 500 |
| Neck, chest, abdomen, back, armpits, shoulders, hips, crotch | 600 |
| Forehead, temporal region, ears, postauricular region | 600 |
| Eyebrows, nose, nasolabial triangle, chin, cheeks, cheekbones, red border of lips | 700 |
| Lower upper eyelids | 850 |
| Ciliary edge of the eyelids | 1 000 |
| External genitalia - single elements* *per 1 mm. 600 rub. | 1 000 |
Removal of papillomas with a diameter of up to 2.0 mm
| Name | Cost in rub. for a unit |
| Neck, chest, abdomen, back, armpits, shoulders, hips, crotch | 300 |
| Lower upper eyelids | 500 |
| Ciliary edge of the eyelids | 1 000 |
Scar treatment
| Name | Cost in rub. |
| Drug injection into the scar | 1 200 |
| Laser dermabrasion (resurfacing) per cm² | 1 200 |
Removal of vascular formations using laser radiation*
| Name | Cost in rub. |
| Photodestruction of the vessels of the wings of the nose | from 5 000 |
| Photodestruction of cheek vessels | from 10 000 |
*exact cost depends on capillary density, repeated stage of vessel destruction minus 30%
Treatment of ingrown toenails using laser radiation
| Name | Cost in rub. |
| Marginal resection of the nail plate | 6 000 |
| Removal of hypergranulations | 1 900 |
| Nail plate removal | 3 500 |
| Complex plastic surgery for ingrown toenails | 8 500 |
Removal of lipoma, atheroma
| Name | Cost in rub. |
| Lipoma removal | 18 000 |
| Removal of atheroma up to 5 mm | 6 000 |
| Removal of atheroma from 5 to 10 mm | 12 000 |
| Removal of atheroma more than 10 mm | 18 000 |
Treatment methods for hemangiomas
Primary therapy for capillary hemangiomas is simple dynamic observation . Since most tumors (up to 75%) regress with age, there is usually no need for their treatment. However, hemangiomas can cause complications that require therapy:
- Systemic complications - congestive heart failure, thrombocytopenia, hemolytic anemia, nasopharyngeal obstruction.
- Ophthalmological complications - disturbance of the visual axis, compression of the optic nerve, severe proptosis (protrusion) of the eyeball, anisometropia (difference in eye refraction).
- Dermatological complications - maceration and erosion of the epidermis, infection of the neoplasm, severe cosmetic defect.
Medicinal methods
Depending on whether the patient has a particular complication, treatment tactics will be different - for example, topical corticosteroids may be prescribed. At the same time, the clinical response to even the most powerful drugs develops quite slowly—over several weeks. Therefore, this method is not suitable for vision-threatening conditions.
Injectable corticosteroids provide a faster effect: blanching of hemangiomas is observed already on days 2–3, and involution becomes noticeable after 2–4 weeks. The success rate of this therapy is about 75%.
Systemic corticosteroids are used for amblyogenic life-threatening lesions. A marked response is usually observed in 30% of patients, a moderate response in 40%, and no response in 30%.
Alpha-2a interferon is prescribed when hemangioma is resistant to corticosteroid therapy. Despite its good effectiveness, its use is associated with undesirable side effects: fever, arthralgia, retinal angiopathy.
Propranolol can be used to treat hemangiomas , although the evidence base is relatively weak and mainly consists of anecdotal cases. However, some studies indicate that propranolol may prevent loss of visual acuity in the case of periocular hemangioma.
For some superficial (and in some cases deeply located) neoplasms of a limited area, timolol .
Hardware methods for treating hemangiomas
CO2 laser was previously used to remove hemangiomas , which has a good hemostatic effect. The disadvantage of the CO2 laser is long-term rehabilitation due to damage to the integrity of the skin, as well as the formation of a scar at the site of the removed hemangioma. Pulsed dye laser ( PDL) is effective only for superficial tumors. Its effect develops quite slowly, which does not allow the use of the PDL laser for complications. Currently, intensive pulsed light - IPL and long-pulse Nd:YAG laser 1064 nm, as well as their combination, are used to treat hemangiomas for aesthetic purposes. These techniques are non-ablative and are based on selective heating of pathological vessels due to the absorption of light energy by hemoglobin.
Indications for removal
In the absence of direct medical indications, a wait-and-see approach can be applied to congenital pathologies, which often pays off. It is of little use to infant tumors, since during the period of intensive growth of the child they can significantly increase in size. In this case, removal of the vascular hemangioma is indicated.
Indications
- Ulceration
- Life-threatening location, e.g. respiratory tract, liver
- Tumor infection
- Growth in depth, which is accompanied by compression of healthy vessels and tissues
- Mechanical damage, etc.
Contraindications to the procedure
- Individual intolerance to laser radiation
- Oncology
- Exacerbation of chronic, infectious, seasonal diseases
- Immunodeficiency conditions
- Systemic blood diseases
- Diabetes mellitus, etc.
You can get acquainted with the full list of contraindications during a consultation with a doctor at our medical center in Moscow. Having studied the complexity of your problem, the specialist will answer all your questions, including whether it is possible to remove hemangioma with a laser in children of a certain age. Reception is by appointment only.