A lipidogram is a medical analysis that talks about lipid, that is, fat metabolism in the body. To perform this study, venous blood is required.
You all know very well that it is important to maintain a balance of proteins, fats and carbohydrates in your diet. So in our body it is also very important that fat, carbohydrate and protein metabolism are normal. The level of fat metabolism is determined by a simple blood test for a lipid profile .
The analysis is completed in just 1 day - And you have the whole truth about fat metabolism!
Requirements for passing the analysis:
1) Strictly on an empty stomach, in the morning, last meal at 19.00. In the morning you can drink plain water 2) The day before, exclude physical activity and intake of fatty foods and alcohol 3) Do not smoke before taking the test and exclude emotional stress.
Indications for taking a lipid profile test:
1) Age 2) Preventive examination, recommended for everyone once a year after 25 years 3) Excess weight 4) Diagnosis of dyslipidemia 5) Liver and kidney diseases 6) Endocrine diseases (diabetes mellitus, hypothyroidism) 7) High blood pressure, hypertensive surges Aggravated heredity for cardiovascular diseases among close relatives (hypertension, coronary heart disease, heart attacks, strokes, obesity) 9) Sedentary lifestyle 10) Bad habits - smoking, drinking alcoholic beverages 11) Diseases that require control of cholesterol levels 12) Taking medications that affect fat metabolism.
Aggravated heredity for cardiovascular diseases among close relatives (hypertension, coronary heart disease, heart attacks, strokes, obesity) 9) Sedentary lifestyle 10) Bad habits - smoking, drinking alcoholic beverages 11) Diseases that require control of cholesterol levels 12) Taking medications that affect fat metabolism.
1.What are cholesterol and triglycerides?
Triglycerides and cholesterol are fatty substances in the blood. Cholesterol in the blood is attached to proteins. The combination of protein and cholesterol is called lipoprotein. A lipoprotein test shows the levels of total cholesterol, low-density lipoprotein (LDL or beta-lipoprotein), high-density lipoprotein (HDL) and triglycerides.
- Cholesterol.
Our body uses cholesterol to build new cells and produce hormones. If cholesterol levels are elevated, it accumulates in the arteries, forming plaques. A large number of plaques increases the chances of heart attack and stroke. - High density lipoprotein (HDL).
High-density lipoprotein helps remove excess fat from the body by taking it from the blood and delivering it to the liver. It is sometimes called “good” cholesterol. High HDL levels reduce the risk of heart disease and stroke. - Low-density lipoprotein (LDL).
Low-density lipoprotein carries fat from the liver to other parts of the body. A low LDL level is normal, because... The body needs it so that certain parts of the body receive the necessary fat. But if LDL is elevated, it increases the risk of developing heart disease. This is why it is sometimes called “bad” cholesterol. - Very low density lipoproteins (VLDL).
VLDL contains very little protein and its main job is to distribute triglycerides that are produced in your liver. High VLDL levels can also lead to cholesterol buildup in the arteries. - Triglycerides.
Triglycerides are a special type of fat that is used to store energy and transfer it to muscles. If you have elevated triglycerides and LDL, this can lead to heart disease faster than just elevated cholesterol.
The state of lipid metabolism in women with early menopause and hypothyroidism
The prevalence of metabolic syndrome (MS) is reaching epidemic proportions, which requires the integration of various medical specialties for the purpose of timely diagnosis, effective treatment and prevention. Impaired lipid metabolism (dyslipidemia) is one of the main factors in the development of MS. In patients with MS, there is often a combination of “traditional” risk markers for coronary heart disease (CHD) (increased levels of cholesterol (CH), low-density lipoproteins (LDL), decreased levels of high-density lipoproteins (HDL)) with non-traditional ones - increased concentrations of triglycerides ( TG), small modified LDL particles (very low density lipoproteins (VLDL)), low HDL levels. It has now been proven that an increase in the level of TG, VLDL and a decrease in the level of HDL are independent factors of coronary artery disease, and also reflect the effect of lipid-lowering therapy.
Dyslipidemias are classified depending on which specific lipids and lipoproteins levels are outside the normal range. According to Fredrickson's classification (1967), 5 phenotypes of dyslipidemia are distinguished. Type I is characterized by an increase in chylomicrons, TG, cholesterol, for type IIa - an increase in LDL, cholesterol (may be normal), for type IIb - an increase in LDL, VLDL, TG, cholesterol, for type III - VLDL, TG, cholesterol, chylomicrons, for type IV - increased VLDL, TG, cholesterol (may be normal), for type V - increased VLDL, chylomicrons, cholesterol, TG. The risk of developing atherosclerosis increases sharply for coronary and peripheral vessels, starting with type IIa.
But this classification does not separate primary and secondary dyslipidemias and does not take into account the level of HDL and genetic defects that underlie many lipid metabolism disorders. Dyslipidemia can only be characterized by an increase in cholesterol (isolated hypercholesterolemia), triglycerides (isolated hypertriglyceridemia), triglycerides and cholesterol (mixed hyperlipidemia).
Primary dyslipidemias are determined by single or multiple mutations of the corresponding genes, as a result of which there is overproduction or impaired utilization of triglycerides and LDL cholesterol or overproduction and impaired clearance of HDL. Primary dyslipidemias can be diagnosed in patients with clinical symptoms of these disorders, with early onset of atherosclerosis (before 60 years of age), in those with a family history of atherosclerosis, or with elevated serum cholesterol levels > 240 mg/dL (> 6.2 mmol/L).
Secondary dyslipidemias usually occur in the population of developed countries as a result of a sedentary lifestyle and consumption of food containing large amounts of cholesterol and saturated fatty acids. Another cause of secondary dyslipidemia may be the development of diseases such as hypothyroidism, estrogen deficiency, diabetes mellitus, etc.
Up to 45–50 years of age, women have a significantly lower risk of developing atherosclerosis compared to men, which is largely due to the protective properties of estrogens, which maintain lipid concentrations within optimal values. However, with the sharp onset of estrogen deficiency, the factors for the development of metabolic disorders increase [1, 2]. The protective effect of estrogens on lipid metabolism is as follows: the production of large, TG-rich VLDL particles increases, which is accompanied by an increase in the level of total TG in the blood; the LDL content decreases by increasing the number of liver receptors for LDL, which subsequently leads to increased catabolism; Estrogens can inhibit the activity of hepatic triglyceride lipase, which leads to an increase in HDL levels due to a delay in their clearance.
The second feature of a deficiency in ovarian estrogen production is a change in the level of gonadotropin production by the pituitary gland and, in particular, an increase in the level of follicle-stimulating hormone (FSH), luteinizing hormone (LH), and thyroid-stimulating hormone (TSH). The prevalence of overt hypothyroidism in the general population is about 2%, and it is 10 times more common among women [4]. Subclinical hypothyroidism (SH) or minimal thyroid deficiency is a condition in which hormonal testing reveals normal free thyroxine (T4) levels and elevated TSH levels. Subclinical hypothyroidism is more common than manifest hypothyroidism - its prevalence varies from 8% to 10% among women [5]. It is interesting to note that among menopausal women, the prevalence of FH increases in direct proportion to cholesterol levels: from 4% in women with low cholesterol levels to 10% in women with the highest cholesterol levels. In addition, it has been shown that in postmenopausal women, an increase in TSH levels by 1 mU/L is accompanied by an increase in cholesterol levels by 0.09 mmol/L (3.5 mg/dL) [5].
Dyslipidemia, which is observed in hypothyroidism, is characterized by an increase in serum levels of VLDL and LDL, which is caused by a deficiency of thyroid hormones, which leads to a decrease in the content of LDL receptors in the liver and, consequently, to a decrease in hepatic excretion of cholesterol and, subsequently, to an increase in the level of LDL and VLDL, rich in apo-B-lipoproteins [6]. LDL receptor expression is negatively regulated by intracellular cholesterol levels mediated by sterol binding regulatory protein-2 (SSRP-2). With long-term hypothyroidism, the structure of HDL is disrupted and the reverse transport of cholesterol is impaired, which is the main anti-atherogenic process in the human body [7]. Studies evaluating the effects of thyroid hormone replacement therapy on lipoprotein levels in patients with thyroidectomy have not found changes in the apolipoprotein (apo-C3) (HDL)/apo-C3 (LDL) ratio, which provides an indirect measure of lipoprotein lipase activity ( LPL), which indicates that in hypothyroidism the activity of this enzyme is not impaired [7].
HDL has the most pronounced antiatherogenic properties; their level is regulated by another key enzyme—hepatic lipase (LLP) [8]. Lipid exchange between lipoproteins is carried out by cholesterol ester transport protein (CETP), which transfers cholesterol esters from HDL to VLDL, and triglycerides back to HDL. Thyroid hormones stimulate fat utilization, mobilization of triglycerides from adipose tissue and activate PL and CETP [6, 8]. CETP is a plasma protein that, as previously stated, mediates the exchange of cholesteryl esters between lipoproteins and is a key factor in HDL metabolism and reverse cholesterol transport pathways. Consequently, a decrease in CETP activity may lead to disruption of these processes. Hepatic lipase (HL) is a glycoprotein produced by the liver that promotes the remodeling of various lipoproteins. With long-term hypothyroidism, a significant decrease in the activity of CETP and PL, which provide approximately 30% of reverse cholesterol transport, can occur [8]. In addition, a decrease in the activity of CETP and PL in hypothyroidism can lead to impaired conversion of LDL to HDL [9]. As a result, there is an increase in serum levels of VLDL, apo-B, LDL and HDL.
Diagnostics
To assess the state of the hypothalamic-pituitary ovarian function in women with early shutdown of ovarian function, it is necessary to conduct a study of the level of FSH, LH, steroid hormones - estradiol, progesterone, androgens in the blood serum.
Diagnosis of hypothyroidism is very specific and accessible. It involves determining the level of TSH and T4, while the detection of an isolated increase in TSH (4.0–10.0 mIU/l with a norm of 0.4–4.0 mIU/l) indicates subclinical hypothyroidism, and a simultaneous increase in TSH level and a decrease T4 level - about obvious or manifest hypothyroidism. The 2000 American Thyroid Association guidelines recommend screening TSH levels at 5-year intervals in all adults over the age of 35 years. The feasibility of population screening is due to the significant prevalence of various thyroid dysfunctions. In addition, subclinical hypothyroidism may be associated with hypercholesterolemia that is reversible with replacement therapy, especially in cases where the TSH level exceeds 10 mIU/L. Determination of TSH levels is an accurate, widely available, reliable and relatively inexpensive test for diagnosing any type of thyroid dysfunction [3].
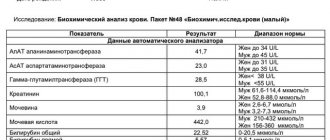
Diagnosis of dyslipidemia is made on the basis of determining the indicators of cholesterol, TG, HDL, LDL and LDL (Table 1).
During the day, even healthy people have fluctuations in cholesterol levels by 10%; TG parameters - by 25%. LDL content is calculated using the Friedewald formula: LDL = cholesterol - (HDL + triglycerides/5), based on the fact that LDL is the amount of cholesterol minus the cholesterol contained in VLDL and HDL. The amount of cholesterol in VLDL is equal to triglycerides/5, since the concentration of cholesterol in VLDL is approximately 1/5 of the total amount of lipids (Table 2).
Fasting lipid profiles are measured in individuals over 20 years of age every 5 years. In this case, it is necessary to identify other risk factors for the development of cardiovascular diseases (diabetes mellitus, smoking, arterial hypertension, family history of the development of coronary artery disease in first-degree relatives).
To assess the ratio of atherogenic and antiatherogenic fractions of cholesterol, we used the cholesterol atherogenicity coefficient proposed by A. M. Klimov (1977), calculated by the formula: CAT = (total cholesterol (TC) - HDL cholesterol)/HDL cholesterol.
Treatment
Considering the frequent development of dyslipidemia against the background of a combination of estrogen and thyroid hormone deficiency in women, timely recommended hormone replacement therapy can reduce the risk of mortality from cardiovascular pathology by 9–13%.
The drug Eutirox belongs to the pharmacological group of thyroid hormone drugs, the active substance of which is levothyroxine sodium (L-thyroxine, L-T4). L-T4 therapy for hypothyroidism is rightly considered the “gold standard”. The action of the drug Eutirox is identical to the action of natural thyroxine. The drug is characterized by high bioavailability (more than 80% when taken orally) and good tolerability, with a long half-life in plasma (about 7 days). When taking Eutirox, side effects are practically absent and can only occur in case of overdose. The daily rhythm of thyroid hormone secretion is practically absent (variation from day to day is less than 15%). In this regard, daily administration of the drug Eutirox in the same dose easily models their endogenous production. The drug should be taken in the morning on an empty stomach 30–40 minutes before meals, once a day, at the same time of day and at least 4 hours apart before or after taking other medications or vitamins. Dosages: 25, 50, 75, 100, 125 and 150 mcg. The quality of life of patients with hypothyroidism who are constantly receiving replacement therapy with Eutirox is almost insignificantly different from that for persons without hypothyroidism.
In case of manifest hypothyroidism, replacement therapy with levothyroxine is indicated at an average dose of 1.6–1.8 mcg/kg of the patient’s body weight. The criterion for the adequacy of this therapy is the persistent maintenance of normal TSH levels in the blood.
For subclinical hypothyroidism, it is recommended: repeated hormonal testing after 3–6 months to confirm the persistent nature of the thyroid dysfunction; Levothyroxine replacement therapy is indicated for persistent subclinical hypothyroidism (increased TSH levels in the blood by more than 10 mU/l, as well as in the case of at least two detections of TSH levels between 5–10 mU/l).
The criterion for the adequacy of replacement therapy for subclinical hypothyroidism is the persistent maintenance of normal TSH levels in the blood.
To treat ovarian hypofunction, in the absence of contraindications, hormone replacement therapy (HRT) (Femoston) is prescribed. Femoston is a combined two-phase drug for hormone replacement therapy, containing micronized 17-beta-estradiol (1 mg) as an estrogenic component and dydrogesterone (10 mg) as a gestagenic component. Both components are chemically and biologically identical to the endogenous female sex hormones produced in the ovaries (estradiol and progesterone).
Estradiol replenishes the deficiency of estrogen in the female body after menopause and provides effective relief of psycho-emotional and vegetative menopausal symptoms, such as hot flashes, increased sweating, sleep disturbances, increased nervous excitability, dizziness, headache, involution of the skin and mucous membranes, especially the genitourinary system (dryness) and irritation of the vaginal mucosa, pain during sexual intercourse).
Taking Femoston leads to a change in the lipid profile towards a decrease in the level of total cholesterol and LDL and an increase in HDL. Dydrogesterone is a gestagen, effective when taken orally, which completely ensures the onset of the secretion phase in the endometrium, thereby reducing the risk of developing endometrial hyperplasia and (or) carcinogenesis (increased with the use of estrogens). Dydrogesterone does not have estrogenic, androgenic, anabolic or glucocorticoid activity.
After taking the drug orally, micronized estradiol is easily absorbed and subsequently metabolized in the liver to form estrone and estrone sulfate. Estrone sulfate undergoes intrahepatic metabolism. Glucuronides of estrone and estradiol are excreted primarily in the urine.
In the body, dydrogesterone is quickly absorbed from the gastrointestinal tract and completely metabolized. The main metabolite of dydrogesterone is 20-dihydrodydrogesterone, present in urine mainly as a glucuronic acid conjugate. Complete elimination of dydrogesterone occurs after 72 hours.
Indications for prescribing Femoston are: hormone replacement therapy for disorders caused by natural menopause or menopause resulting from surgical intervention; prevention of osteoporosis in postmenopause.
To date, the question of the effect of sex steroid hormone therapy on thyroid status remains insufficiently studied; the data available in the literature on this issue are somewhat contradictory. The only thing that has been reliably established is the impossibility of a direct influence of estrogens on the hormone-producing function of the thyroid gland due to the absence of receptors for estrogens and progesterone in its tissue. Fluctuations in thyroid hormone levels are adaptive in nature during the period of adaptation to HRT. This period in patients with hypothyroidism takes about 6 months, while in women without thyroid pathology, according to the literature, it lasts for 3 months, which may be due to a decrease in metabolism in the liver due to a lack of thyroid hormones. An increase in T4 levels during HRT in women with primary hypothyroidism in menopause can be explained by an increase in the sensitivity of thyrotrophs to TSH estrogens. In this situation, eliminating estrogen deficiency can increase the functional activity of the thyroid gland in the absence of profound irreversible changes in its tissue (Table 3).
At the District Clinical Perinatal Center in Surgut, we examined 45 women with early menopause. The average age of the patients was 32.7 ± 2.3 years. The average duration of the disease was 6.8 ± 1.6 years. The reason for contact was the absence of menstruation, rapid weight gain (on average 10 ± 2.1 kg/year) in 77.8% of patients since the cessation of menstruation. When analyzing the body mass index of women in the clinical group, it was revealed that only 22.2% of patients had normal body weight, 44.4% had a body mass index within the range of overweight, 17.8% had mild obesity, 11 .1% have moderate obesity and 4.4% have extreme obesity.
With an increase in the level of FSH (average value 32.4 ± 8.5 U/ml) and LH (15.8 ± 3.1 U/ml), a decrease in the level of estradiol and progesterone in the blood plasma of patients was observed. The higher the level of FSH in the blood plasma, the more pronounced were the echographic signs of ovarian hypofunction, such as a decrease in ovarian volume (average value 1.25 ± 0.23 cm3), number of follicles (average number - 3.4 ± 1.4 ) and an increase in the resistance index in the ovarian artery (average RI = 0.78). When assessing thyroid function, the average TSH value was 12.3 ± 0.45 IU/l, a decrease in T4 levels in 64.4% of patients. According to ultrasound data, both during combination therapy (simultaneous administration of the drugs Eutirox and Femoston) and during monotherapy with levothyroxine, the volume of the thyroid gland decreased by 8% and amounted to 20.9 ± 1.3 cm3.
We studied and compared the results of lipid metabolism in women. During the initial assessment of the parameters of the blood lipid spectrum, various variants of its disturbance were identified in 93.3% of women with hypothyroidism and early menopause. In hypothyroidism, type IIa dyslipidemia was more common (55.5%), and type IIb, accompanied by an increase in all atherogenic fractions of the lipid spectrum, was detected in 26.6% of cases, while in the euthyroid state only 13.3% had this type. female patients. A detailed study of the concentration of various classes of lipoproteins depending on the functional state of the thyroid gland found that women with uncompensated hypothyroidism have a significantly higher level of cholesterol by 30.3% (p < 0.05), LDL by 18.7% (p < 0 .05), TG by 15.6% (p < 0.05) and atherogenicity coefficient by 58.2% (p < 0.05).
Despite lower concentrations of atherogenic lipid fractions in women without thyroid pathology, these patients had an increase in atherogenic potential, indicating an inversely proportional relationship between the atherogenicity coefficient and the concentration of the antiatherogenic HDL fraction. Thus, we have identified a high incidence of thyroid pathology, in particular hypothyroidism, in women with estrogen deficiency. Both pathological conditions lead to the development of dyslipidemia as one of the manifestations of MS. Complex HRT (Femoston and Eutirox) has a positive effect on blood lipid metabolism, reducing the atherogenicity coefficient by 17.5% (p < 0.05).
Literature:
- Azizova D. Sh. State of lipid metabolism in women with postovariectomy syndrome in conditions of chronic iodine deficiency // Pediatrics. Specialist. release. 2003. pp. 183–189.
- Serebrennikova K. G., Chumakova N. V., Konev M. V. The effect of hormone replacement therapy on some metabolic processes in women with surgical menopause. Materials of the First Russian Congress on Menopause, Moscow, September 10–12, 2001. Menopause. 2001; 3:67.
- Fadeev V.V. Modern concepts of diagnosis and treatment of hypothyroidism in adults // Probl. Endocrinol. 2004. No. 2. P. 47–53.
- Vanderpump MP, Tunbridge WM Epidemiology and prevention of clinical and subclinical hypothyroidism // Thyroid. 2002. Vol. 12. P. 839–847.
- Bindels AJ, Westendorp RG, Frolich M. et al. The prevalence of subclinical hypothyroidism at different total plasma cholesterol levels in middle aged men and women: a need for case finding // Clin Endocrinol. 1999. Vol. 50. P. 217–220.
- Shin DJ, Osborne TF Thyroid hormone regulation and cholesterol metabolism are connected through Sterol Regulatory Element-Binding Protein (SREBP-2) // J Biol Chem. 2003. Vol. 278. P. 34114–34118.
- Dredecjus M., Masson D., Gautier T. et al. Low cholesteryl ester transfer protein (CETP) concentration, normal CETP activity in serum from patients with shortterm hypothyroidism. Lack of relationship to lipoprotein abnormalities // Clin Endocrinol. 2003. Vol. 58. P. 581–588.
- Franco M., Castro G., Romero L. et al. Decreased activity of lecithin: acyltransferase and hepatic lipase in chronic hypothyroid rats: implications for reverse cholesterol transport // Mol Cell Biochem. 2003. Vol. 246. P. 51–56.
- Zambon A., Bertocco S., Vitturi N. et al. Relevance of hepatic lipase to the metabolism of triacylglycerol rich lipoproteins // Biochem Soc Trans. 2003. Vol. 31. P. 1070–1074.
L. D. Belotserkovtseva , Doctor of Medical Sciences, Professor L. V. Kovalenko , Doctor of Medical Sciences, Professor E. V. Korneeva, Candidate of Medical Sciences, Associate Professor
State Educational Institution of Higher Professional Education, Surgut State University of Khanty-Mansi Autonomous Okrug-Yugra, Surgut
Contact information for authors for correspondence
2.Why measure cholesterol and triglycerides?
A test for cholesterol and triglycerides in the blood is done in the following cases:
- You have lipidosis (lipid metabolism disorder). In this case, analysis of triglycerides and cholesterol in the blood is done regularly;
- To check the progress of treatment for lipid metabolism disorders;
- To help determine your risk of heart disease, especially if there are other factors that negatively affect your heart health;
- If you have unusual symptoms - yellow fatty deposits on the skin (xanthomas), which can form due to rare genetic diseases that raise cholesterol levels.
Low triglycerides in the blood: what does this mean?
Hypotriglyceridemia is a condition in which a general analysis or lipid profile shows a persistent decrease in the level of triglycerides in the blood serum. This means that the body does not have enough fats, it does not absorb them well or cannot produce them in the required volume.
The main reason why you should be wary of triglyceride deficiency is a person’s lack of vital energy necessary for his full functioning. Also, all lipid-dependent processes (stimulation of metabolism, formation of cell membranes, thermoregulation, etc.) suffer from hypotriglyceridemia: they are inhibited or stop completely.
The normal concentration of triglycerides is individual - it is determined by the age and gender of the patient:
- in children from birth to 14 years – 0.32–1.46 mmol/l;
- in women from 14 to 45–60 years old – 0.41–2.72 mmol/l;
- in men from 14 to 55–65 years old – 0.60–3.58 mmol/l;
- in old people aged 50–65 years and older – 0.61–2.86 mmol/l.
If the value of neutral fats falls beyond the lower limit, this indicates a high risk of disruption of the physiological mechanism of neuromuscular transmission, which is accompanied by severe fatigue and can lead to the development of serious diseases
Reference . A decrease in triglyceride levels is usually accompanied by changes in other lipid parameters, as well as a slower erythrocyte sedimentation rate (ESR) and a decrease in platelet counts.
3.How to prepare and how is the analysis carried out?
How to prepare for a blood cholesterol and triglyceride test?
Preparation will depend on the type of analysis. Ask your doctor what tests will be done and he will tell you how to prepare. General recommendations before analysis are:
- Do not drink alcohol before the test;
- Don't eat fatty foods the day before the test;
- Avoid vigorous exercise before the test.
Tell your doctor about the radiation test you recently had.
How are triglycerides and cholesterol tested?
The level of cholesterol and triglycerides in the blood is measured after it is taken from a vein. Blood sampling is carried out according to a standard procedure.
Which doctor should I contact for treatment?
Initially, the diagnosis of hyportriglyceridemia is made by a general practitioner - a family doctor, pediatrician or local physician. They also give the patient basic nutritional recommendations and prescribe medications. In the future, based on the cause of the disease, concomitant pathologies and the dynamics of treatment, the intervention of specialized doctors may be required: a cardiologist, endocrinologist, pulmonologist, nutritionist and psychotherapist.
Since low triglyceride levels are not an independent disease, but a consequence of other ailments, in order to increase it, it is necessary to eliminate the root cause and carefully monitor your diet. Only with such an integrated approach can hypotriglyceridemia be cured and the development of serious complications prevented.
4.What are the risks and what could interfere with the analysis?
What are the risks of testing for triglycerides and cholesterol?
Possible risks of blood testing for cholesterol and triglycerides may only be associated with the blood collection itself. In particular, the appearance of bruises at the puncture site and inflammation of the vein (phlebitis). Warm compresses several times a day will relieve phlebitis. If you are taking blood thinning medications, you may bleed at the puncture site.
What can interfere with the analysis of cholesterol and triglycerides?
Testing for cholesterol and triglycerides may be interfered with by:
- Taking medications such as diuretics, corticosteroids, androgens, tranquilizers, estrogens, contraceptives, antibiotics, vitamin B3;
- Physical overload – infection, previous surgery, heart attack;
- Eating 9-12 hours before the test;
- Diseases such as hypothyroidism, diabetes, liver and kidney diseases;
- Abuse of alcohol or drugs, or sudden cessation of their use;
- Pregnancy.
What do we have to do?
- First of all, go to the doctors immediately! In order to identify the reasons for the decrease in triglyceride levels in order to prescribe adequate treatment for “hidden” (possibly for years) diseases. Or reduce the risk of developing other dangerous diseases, which will be discussed below. Or take social measures (in the case of malnutrition - due to poverty or bullying from other people).
- Secondly, they definitely need to be normalized! At the discretion of the doctor: either by changing the diet, or by adjusting the treatment of other diseases (if a decrease in the amount of TG is a side effect after taking certain medications.