Adrenergic blockers (adrenolytics) are medications that block adrenergic receptors of various types in organs and tissues, preventing the implementation of the effects of natural biologically active substances - the mediator norepinephrine and the adrenal hormone adrenaline.
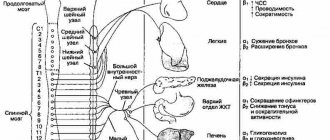
Norepinephrine is a transmitter of impulses in the peripheral nervous system, regulating the functioning of many internal organs and systems (in particular, the heart, blood vessels, bronchi, uterus, pancreas, urinary system, etc.). Adrenaline is similar in structure and function to norepinephrine and is a hormone of the inner (brain) layer of the adrenal cortex.
Norepinephrine and adrenaline realize their effects through interaction with special structural components of cells - receptors, namely adrenergic receptors. Depending on their location and functions, adrenergic receptors are classified into alpha (α)- and beta (β)-adrenergic receptors.
α-Adrenergic receptors are located mainly in blood vessels, the iris of the eye, and the urinary tract. The effects of α-adrenergic receptor stimulation include constriction of blood vessels (and consequently increased blood pressure), pupil dilation, and urinary retention.
β-Adrenergic receptors are localized primarily in the heart (β1-adrenergic receptors), as well as in the bronchi and uterus (β2-adrenergic receptors). When they are stimulated, an increase in the strength and frequency of heart contractions, dilation of the bronchi and relaxation of the uterus are observed.
There is a separate class of drugs that can stimulate adrenergic receptors (adrenergic agonists, adrenergic stimulants), and a group of drugs that can block adrenergic receptors (adrenergic blockers, adrenergic steroids).
Depending on the degree of selectivity, adrenergic blockers are divided into α-adrenergic blockers, β-adrenergic blockers, as well as α- and β-adrenergic blockers. Let us consider in detail drugs that block α-adrenergic receptors.
What are alpha blockers
These are substances that inhibit the effect on alpha receptors.
They dilate blood vessels, thereby reducing resistance in the periphery, facilitating blood circulation and naturally reducing blood pressure. In addition, these drugs effectively lower cholesterol and fat levels, that is, they regulate lipid metabolism.
Therefore, in some cases they are used for obesity.
Beta adrenergic receptors
These elements include beta 1, 2 and 3 adrenergic receptors:
- Beta increases heart contraction and also increases blood pressure.
- Beta 2 increases the amount of glucose that enters the blood.
- Beta 3 is located in adipose tissue. When activated, energy production is ensured along with increased heat production.
Alpha 1 and beta 1 bind norepinephrine. And alpha 2 and beta 2, in turn, bind norepinephrine and adrenaline. It is worth saying that adrenaline is better captured by beta 2 adrenergic receptors.
How do alpha and beta blockers work?
In what cases do alpha blockers give results and why take them?
Alpha blockers for hypertension in combination with beta blockers allow you to correct and regulate the disease at various stages of its development:
- Moderate hypertension - blood pressure rises from 140/90 to 178/113. At this stage, the nervous system works correctly and fully.
- Severe - at this stage, the pressure can increase from 180/115 to 300/129. These jumps are dangerous to health and life. Many years of research and experience have shown that with such pressure, irreversible changes occur in the body, especially in the cardiovascular system and brain. The fundus of the eye changes its structure. There are malfunctions in the liver and kidneys.
Many patients who are forced to use alpha-blockers for the first time to treat hypertension for a long time study the instructions for a long time and consult with a doctor. Many people are concerned about the presence of serious side effects in the instructions. But these medications, like any other, cause a number of complications. This does not mean at all that any of them will make themselves felt.
To ensure that patients understand the essence of therapy, the attending doctor explains the tasks of alpha blockers during the treatment of high blood pressure:
- For most people, hypertension is stressful. And because of this, the patient feels uncomfortable. Therefore, the first goal of taking antihypertensive drugs is to improve the patient's physical condition and relieve symptoms.
- If hypertension is not treated, the disease can lead to the development of severe consequences, from which it may be impossible to fully recover.
- If treatment is started on time, it significantly prolongs the patient’s life and prevents strokes and crises.
pharmachologic effect
α-Adrenergic blockers block α-adrenergic receptors in blood vessels, which leads to their dilation and, as a result, a decrease in blood pressure, as well as normalization of peripheral circulation; in addition, by blocking α-adrenergic receptors in the urinary tract, α-blockers facilitate urination in patients with benign prostatic hyperplasia.
Nicergoline dilates blood vessels in the brain, improves cerebral blood flow, increasing blood flow to ischemic (suffering from a lack of oxygen) areas of the brain.
Dihydroergotamine tones the blood vessels of the brain, eliminates acute migraine attacks.
Indications for use
Alpha receptor inhibitors are used for hypertension in the following cases:
- arterial hypertension;
- malfunctions in the functioning of the vestibular apparatus;
- migraine;
- dementia;
- chronic heart failure;
- disturbances of blood flow in the brain and in the periphery;
- restlessness and anxiety syndrome;
- ischemic optic neuropathy;
- urinary disorder;
- complicated diabetes mellitus;
- diseases of the cornea;
- prostate enlargement and adenoma.
α-adrenergic receptor blockers as antihypertensive drugs
Thus, despite the widespread use of thiazide diuretics,
β AT1 α1 blockers are still the antihypertensive drugs of choice in some clinical situations.
For certain indications, non-selective a-blockers also continue to be used. Blockers of a-adrenergic receptors are divided into two main groups: 1) non-selective, which weaken the effects of catecholamines on both a1- and a2-adrenergic receptors; 2) selective, which selectively block the effects of catecholamines on α1-adrenergic receptors of blood vessels and other organs and tissues. In addition, some antihypertensive drugs that do not formally belong to the group of α-blockers have α-adrenergic blocking properties (Table 1). For example, an α1-adrenergic blocking effect was found in two non-selective β-adrenergic blockers, carvedilol and labetolol, in the selective C2-serotonin receptor blocker ketanserin, and in the central C1A-serotonin receptor agonist urapidil.
| Table 1Main groups of blockersa-adrenergic receptors 1. Non-selective a-blockers: Dihydrogenated ergot alkaloids (dihydroergotoxin, etc.) Piroxican Tropaphen Phenoxybenzamine Phentolamine 2. Selective a-blockers: Alfuzosin Bunazosin Doxazosin Prazosin Tamsulosin Terazosin Trimazosin 3. Other drugs with Droperidol (antipsychotic) Indoramine (central C1A serotonin receptor agonist) Carvedilol (non-selective b-blocker) Ketanserin (C2-serotonin receptor blocker) Labetolol (non-selective b-blocker) Urapidil (central C1A serotonin receptor agonist) Chlorpromazine (aminazine; antipsychotic) |
Non-selective α-blockers include drugs such as phentolamine, phenoxybenzamine and dihydrogenated ergot alkaloids. Phentolamine
causes a short-term and reversible blockade of both postsynaptic a1-adrenergic receptors of smooth muscle cells of the vascular wall, and presynaptic and extrasynaptic a2-receptors. Phentolamine is an effective antihypertensive drug. It is used primarily in the treatment of hypertensive crises associated with hypercatecholaminemia, such as in patients with pheochromocytoma. During a hypertensive crisis, phentolamine is administered intravenously as a bolus or intravenous infusion (2.5-10 mg). Phentolamine is also used for diagnostic purposes in cases of suspected pheochromocytoma in cases where biochemical confirmation of the diagnosis is not possible. Along with pheochromocytoma, the development of a hypercatecholamine crisis can be a consequence of sudden withdrawal of the central α2-adrenergic receptor agonist clonidine, and is also observed in patients taking monoamine oxidase inhibitors (MAOIs).
Table 2 Comparative characteristics
of a 1 -blockers
| Drugs | Duration of action, h | Maximum action, h | Therapeutic doses, mg/day | Frequency of intake per day. |
| Bunazosin retard | ~ 24 | ? | 6-12 | 1 |
| Doxazosin | 18-36 | 5-6 | 1-20 | 1 |
| Prazosin | 4-6 | 0,5 | 1-20 | 2-3 |
| Terazosin | > 18 | 1-1,7 | 1-20 | 1-2 |
| Trimazosin | 3-6 | 3-7 | 100-900 | 2-3 |
| Indoramine | > 6 | 2 | 50-150 | 2-3 |
| Ketanserin | > 12 | 1-2 | 20-40 | 1-2 |
| Urapidil | 6-8 | 3-5 | 15-120 | 1-2 |
| Based on: N. Kaplan [8] with some changes and additions. | ||||
In patients receiving MAO inhibitors, a hypercatecholamine hypertensive crisis may develop while taking medications or foods containing tyramine, ephedrine and other sympathomimetic amines. Foods rich in tyramine and therefore incompatible with MAO inhibitors include chocolate, bananas, soybeans, kefir, buttermilk, chicken liver, some cheeses (cheddar, Camembert and Stilton) and wines (such as Chianti), as well as yeast extracts ( including pubs). Sympathomimetic amines, among other things, are included in combination drugs used in the treatment of rhinitis, hay fever and bronchial asthma. Phenoxybenzamine
unlike phenthalamin, it causes long-term and irreversible blockade of a-adrenergic receptors.
Its α-adrenergic blocking effect after oral administration lasts up to 2 days or more. Phenoxybenzamine is used to treat patients with pheochromocytoma before surgery, as well as in inoperable cases. The initial dose of the drug is 10 mg 1 time per day. If necessary, the dose of phenoxybenzamine is gradually increased in order to reduce blood pressure (BP) to the desired level. Neither phentolamine nor phenoxybenzamine are used in the treatment of hypertension, as they often cause side effects such as orthostatic hypotension, reflex tachycardia, dizziness, weakness and others. The side effects of phenthalamin and phenoxybenzamine are explained by the nonselectivity of their action on α-adrenergic receptors. After all, these non-selective α-adrenergic blockers exert their antihypertensive effect mainly due to the blockade of α1-adrenergic receptors of the vascular wall. The blockade of a2-adrenergic receptors located on the presynaptic membrane of the endings of sympathetic nerve fibers caused by phentolamine and phenoxybenzamine is generally undesirable in patients with arterial hypertension. When blocking presynaptic a2-adrenergic receptors, the release of norepinephrine (norepinephrine) from the endings of the sympathetic nerves increases and at the same time the release of acetylcholamine from the endings of the vagus nerve decreases [1, 2]. Of the dihydrogenated ergot alkaloids, only dihydroergotoxin
.
The fact is that dihydroergotoxin methanesulfonate ( dihydroergocristine
) is part of such once popular combination antihypertensive drugs as brinerdine, cristepine and sinepres.
Dihydroergotoxin and other dihydrogenated ergot alkaloids are traditionally classified as α-blockers [3, 4]. However, according to some observations, the antihypertensive effect of dihydroergotoxin derivatives is at least partly mediated by dopaminergic mechanisms. In the early 70s, prazosin was synthesized, which was much better tolerated than other α-adrenergic receptor blockers. Further studies showed that prazosin is a selective blocker of postsynaptic α1-adrenergic receptors. In the 80s and 90s, other α1-blockers were created (alfuzosin, bunazosin, doxazosin, terazosin, tamsulosin, etc.). But among the available α1-blockers, the majority of pharmaceutical manufacturers are intended for the treatment of benign prostatic hyperplasia (for example, alfuzosin and tamsulosin). For long-term therapy of hypertension, two selective α1-blockers were used - prazosin and doxazosin. In addition, terazosin and the retard form of bunazosin seem promising [5-7]. Prazosin
is a selective α1-blocker with a relatively short antihypertensive effect, so it must be taken 2-3 times a day (Table 2).
After oral administration, prazosin is rapidly absorbed from the gastrointestinal tract. Plasma concentrations of the drug reach a maximum after 2-3 hours. More than 70% of prazosin is bound to plasma proteins. It is metabolized mainly in the liver, 70% of prazosin and its metabolites are excreted in feces, the rest through the kidneys. The half-life of prazosin in blood plasma is 2-4 hours. Prazosin is characterized by the so-called first dose effect - a sharp decrease in blood pressure after taking the first dose of the drug, which is especially pronounced in the orthostatic position and is manifested by dizziness and, in some cases, fainting. Experience in the clinical use of prazosin shows that in terms of antihypertensive effectiveness it is not inferior to thiazide diuretics, beta-blockers, calcium antagonists and ACE inhibitors. According to the observations of F. Zeenen et al. [9], prazosin causes reversal of left ventricular hypertrophy in men with hypertension. The additional pharmacological effects of prazosin and other α1-blockers are of important clinical significance. Unlike all other antihypertensive drugs, selective a 1 -blockers improve blood lipid composition.
They significantly reduce the level of total cholesterol in the blood due to its atherogenic fraction, low-density lipoprotein cholesterol, and at the same time increase the levels of anti-atherogenic high-density lipoprotein cholesterol.
Under the influence of α1-blockers, the content of triglycerides also decreases [10]. Prazosin and other α1-blockers increase tissue sensitivity to the action of insulin.
They cause a small but statistically significant decrease in basal glucose levels (by 7 mg/dL or 5%) and insulin (by 14 pmol/L or 17%) in patients with hypertension.
The predominance of α1-adrenergic receptors in the smooth muscles of the prostate gland and bladder neck served as the basis for the use of prazosin, and then other α1-adrenergic blockers in patients with benign prostatic hyperplasia (adenoma). A number of controlled studies have shown that α 1 -blockers significantly improve clinical symptoms and signs in patients with benign prostatic hyperplasia.
In particular, they increase the maximum and average flow rate of urination.
Due to these beneficial pharmacological properties, prazosin and other α1-blockers are considered particularly indicated for the treatment of hypertension in patients with benign prostate adenoma, atherogenic dyslipidemia, diabetes mellitus, or impaired glucose tolerance. Another indication for the use of a1-blockers is the treatment of benign prostatic hyperplasia, regardless of blood pressure levels.
Observations show that in individuals with initially normal blood pressure, a1-blockers improve urination without having a significant antihypertensive effect.
For this reason, a1-blockers can be used to treat benign prostatic hyperplasia in patients with both high and normal blood pressure. Despite its potentially beneficial properties, the first selective α1-blocker prazosin was not widely used in the treatment of hypertension due to the frequent development of side effects, as well as insufficiently high antihypertensive effectiveness with long-term use. Thus, in the multicenter controlled study VACS (Veterans Affair Cooperative Study), due to side effects, prazosin had to be discontinued in 12% of patients. Weakness, drowsiness and dizziness occurred significantly more often during treatment with prazosin than when prescribed placebo [11]. Prazosin, with long-term use, was not effective enough as an antihypertensive drug in black patients (30-35%), as well as in young white men (46%). And only in white men aged 60 years and older was the antihypertensive effectiveness of prazosin quite high (66%) [12]. The results of the VACS study regarding the effect of prazosin on left ventricular hypertrophy in patients with essential hypertension were unexpected. After 1 year of prazosin therapy, left ventricular myocardial mass did not decrease. In patients with an initial left ventricular mass of no more than 350 g, treatment with prazosin was accompanied by an insignificant increase in the mass of the left ventricular myocardium [13]. Considering the short-term effect of prazosin, insufficient antihypertensive effectiveness, lack of effect on left ventricular hypertrophy and poor tolerability, it is not difficult to understand why the first selective α1-blocker has been rarely used in recent years for long-term treatment of hypertension. Doxazosin
is another selective α1-blocker that has all the valuable pharmacological properties of prazosin, but without many of its disadvantages.
As an α1-adrenergic blocker, doxazosin is more than 2 times more selective than prazosin for α1-receptors. Doxazosin has a long-term antihypertensive effect, which lasts from 18 to 36 hours. Due to this, doxazosin is prescribed once a day. Doxazosin does not have a “first dose effect”. It is characterized by a gradual onset of antihypertensive action. With a single oral dose in the morning, the maximum antihypertensive effect of doxazosin is observed after 5-6 hours [8, 14]. When taking the drug at night, the maximum effect occurs after 8-12 hours and occurs between 6 and 11 a.m., i.e. to the morning rise in blood pressure [15]. The morning rise in blood pressure, which is associated with hyperactivation of the sympathetic-adrenal system, in patients with hypertension is often combined with the development of cardiovascular complications such as cerebral stroke and myocardial infarction. Therefore, it is assumed that the preventive effect of doxazosin on hypertension may be more pronounced if the drug is prescribed at night, rather than in the morning, as is usually done. In terms of pharmacokinetic parameters, doxazosin also differs significantly not only from prazosin, but also from other selective α1-blockers. After oral administration, doxazosin is almost completely absorbed from the gastrointestinal tract. Food slows down the absorption of doxazosin by approximately 1 hour, but does not have a significant effect on its main pharmacokinetic parameters. Therefore, it is believed that doxazosin can be taken with food and not just on an empty stomach. The bioavailability of the drug ranges from 62 to 69%. In the blood, 98-99% of doxazosin circulates in association with plasma proteins. Plasma concentrations of doxazosin reach a maximum 2-3 hours after oral administration of the drug. Its half-life in blood plasma ranges from 19 to 22 hours, which is significantly longer than that of all other α1-blockers. The antihypertensive efficacy of doxazosin compared with placebo, amlodipine, acebutolol, chlorthalidone and enalapral was well studied in the large randomized trial TOMH,S (Treatment Af Mild Hypertension Study), which involved 902 patients with mild hypertension (initial diastolic blood pressure within from 90 to 99 mmHg). Patients were observed monthly for 4 years. When treated with doxazosin (1-2 mg/day), mean blood pressure values significantly decreased compared to placebo (by 13.4/11.2 mmHg versus 8.6/8.8 mmHg; p< 0.01). The antihypertensive effect of doxazosin did not differ from the effects of other antihypertensive drugs, such as the calcium antagonist amlodipine, the β-blocker acebutolol, the thiazide-like diuretic chlorthalidone, and the ACE inhibitor enalapril. Monotherapy with doxazosin was effective throughout the 4 years of observation in 66% of patients. In 22% of other patients, the drug was effective when combined with chlorothiazide and other antihypertensive drugs. Doxazosin caused a reverse development of left ventricular hypertrophy, and in its ability to reduce the mass of the left ventricular myocardium, it was practically no different from other antihypertensive drugs studied. Like other antihypertensive drugs, doxazosin, with long-term therapy, reduced the increased risk of cardiovascular complications in patients with hypertension. Over 4 years of follow-up, the incidence of cardiovascular complications in the group of patients treated with doxazosin was significantly lower than in the control group (11.9% versus 15.8% in the control group). Doxazosin did not stand out among the antihypertensive drugs studied in the TOMH'S study either in terms of its effect on the quality of life of patients or in the frequency of side effects [16]. In a large placebo-controlled study (675 hypertensive patients), the following side effects were more common in the doxazosin-treated group than in the control group: dizziness (21% versus 10%), weakness (12% versus 6%), drowsiness ( 5% vs. 1%), hypotension (1% vs. 0%), and orthostatic hypotension (0.3% vs. 0%). These data indicate that the incidence of adverse events with doxazosin is significantly lower than with prazosin. The TOMH'S study examined the effects of amlodipine, acebutolol, doxazosin, chlorthalidone, and enalapril on sexual function in men and women. Before prescribing antihypertensive drugs, 14.4% of men and 4.9% of women reported sexual dysfunction. 12.2% of men complained of erectile dysfunction before the study, 9.5% after 24 months, and 14.7% after 48 months. The incidence of erectile dysfunction in men depended on the age of the patients and the antihypertensive drug used. After 24 months of therapy, the incidence of erectile dysfunction was highest in the group of patients treated with chlorthalidone (15.7%) and lowest in the group of patients treated with doxazosin (2.8%). In the groups of patients receiving amlodipine, acebutolol and enalapril, the incidence of erectile dysfunction was 6.7, respectively; 7.9 and 6.5% and did not differ significantly from that in the control group (4.9%). After 48 months of therapy, the differences between the groups of patients in the incidence of erectile dysfunction were smaller than after 24 months. At the end of the study, 7 of 8 patients receiving doxazosin, 5 of 11 receiving amlodipine, 5 of 13 receiving acebutolol, 5 of 11 receiving chlorthalidone, 6 of 8 receiving enalapril, and 6 of 14 receiving placebo reported regaining erections. . The frequency of erection normalization, therefore, was greatest in the group of hypertensive patients treated with doxazosin. In women, no significant differences were found in the effect of antihypertensive drugs on sexual dysfunction [17]. Thus, when doxazosin is used as an antihypertensive drug in men, sexual dysfunction occurs much less frequently than when other antihypertensive drugs are prescribed. In a significant proportion of men with erectile dysfunction, sexual function is normalized under the influence of doxazosin therapy. There are reports in the literature that prazosin can also improve sexual function in men. Therefore, it can be assumed that the ability to normalize impaired sexual function in men is inherent in all selective α1-blockers. So, the presented literature data indicate that selective α1-blockers (especially doxazosin) are effective antihypertensive drugs. In some clinical situations, doxazosin and, to a lesser extent, other α1 - blockers may be more useful in the treatment of hypertension than thiazide diuretics, β -blockers, calcium antagonists, and ACE inhibitors, namely in patients with concomitant benign prostatic hyperplasia (adenoma). glands, erectile dysfunction, diabetes mellitus, atherogenic dyslipidemia, chronic obstructive pulmonary diseases and obliterating atherosclerosis of the vessels of the lower extremities.
Literature:
1. Sidorenko B.A., Preobrazhensky D.V. A short guide to the treatment of hypertension. M., 1997. 2. Sidorenko B.A., Preobrazhensky D.V. B-blockers, M., 1996. 3. Metelitsa V.I. Cardiologist's Handbook of Clinical Pharmacology. 2nd edition. M., 1987. 4. Lawrence D.R., Benitt P.N. Clinical pharmacology, M., 1991, volume 2, 345-48. 5. Oshchepkova E.V., Epifanova O.N., Arabidze G.G. The use of the α-adrenergic blocker doxazosin in the treatment of arterial hypertension - Cardiology, 1998;4:76-82. 6. Reid JZ. The place of alpha blockers in the treatment of hypertension — Clin. Exper. Hypertension 1993;15:1291-97. 7. Veelken R., Schmieder RE., Overview of a1-adrenoceptor antagonism and recent advances in hypertensive therapy - Amer. J Hypertens 1996;9(suppl):1395-495. 8. Kaplan NM. Clinical hypertension 7th edition - Baltimore, 1998. 9. Zeenen FHH., Smith DZ., Farkas RM. et al. Vasodilators and regression of left ventricular hypertrophy: hydralazine versus prezosin in hypertensive humans - amer. J Med 1987;82:969-76. 10. Nash DT. a — adrenergic blockers: Mechanism of action, blood pressure control, and effects on lipoprotein metabolism — Clin. Cardiol 1990;13:764-72. 11. Materson BJ., Reda DJ., Cushman WC. et al. Singledrug therapy for hypertension in men. A comparison of six antihypertensive agents with placebo - New Engl. J Med 1993;328:914-21. 12. Materson BJ., Reda DJ., Cushman WC. et al. Department of Veterans Affairs single-drug therapy of hypertension study. Revised figures and new data - Amer. J. hypertens., 1995;8:189-192. 13. Yottediener JS., Reda DJ., Massie BM. et al. Effect of single-drug therapy on reduction of left ventricular mass in mild to moderate hypertension—Cirhulation, 1997;95:2007-14. 14. Elliott HZ., Meredith PA., Vincent J. et al. Clinical pharmacological studies with doxazosin - Brit J. Clin Pharmacol., 1986;21 (suppl 1): 275-315. 15. Pickering TY., Zevenstein M., Walmsley P. et al. Nighttime dosing of doxazozin has peak effect on morning ambulatory blood pressure. Results of the HAZT Study - Amer. J Hypertens 1994;7:844-47. 16. Elliott HZ., Meredith PA., Reid JZ. Pharmacokinetic overview of doxazozin - Amer. J Cardiol 1987;59:789-819. 17. Fulton B., Wagstaff AJ., Sorkin EM. Doxazozin. An update of its clinical pharmacology and therapeutic applications in hypertension and benign prostatic hyperplasia - Drugs, 1995;49:295-320. 18. Neaton JD, Yrimm RH., Jr., Prineas RJ. et al. Treatment of Mild Hypertension Study. Final results - JAMA., 1993;270:713-724. 19. Yrimm RH, Jr Yrandis YA, Prineas RJ. et al. Long-term effects on sexual function of five antihypertensive drugs and nutritional hygienic treatment in hypertensive men and women - Hypertension, 1997;29:8-14.
Classification of funds
To combat the main symptoms of hypertension, it is necessary to block certain classes of nerve endings:
- alpha-1 receptors of vascular smooth muscle fibers;
- alpha-2 receptors of the vasomotor center and the nerve cell conducting the impulse.
To treat arterial hypertension, inhibition of adrenolytic drugs on the corresponding receptors is used. In this case, a significant decrease in norepinephrine occurs, and this normalizes blood pressure. There are 2 broad groups of drugs based on the type of effect on receptors:
- Adrenolytics of selective action. They selectively block only alpha-1 receptors.
- Non-selective adrenolytics. Prevents dilation of blood vessels and receptors of the motor center.
Non-selective blockers are not intended for long-term use. For the treatment of hypertension, alpha blockers of this group are used only to relieve attacks.
Types of drugs
Below is a table of alpha blockers to help you better find the information you need. The table contains lists of drugs, the name of the active substance and commercial names of drugs based on the active component.
Alpha blocker medications
| Group | Active substance | Commercial names of products |
| Alpha-1-blocker drugs | Alfuzosin |
|
| Doxazosin |
| |
| Prazosin |
| |
| Silodosin |
| |
| Terazosin |
| |
| Urapidil |
| |
| Alpha-2 blockers | Yohimbine |
|
| Alpha-1,2-blockers | Dihydroergotoxin |
|
| Proroksan |
| |
| Phentolamine |
|
The dose and duration of drug use are determined by the severity of the disease, the patient’s age and the presence or absence of chronic pathologies.
Rules for taking medication
Medicines are prescribed only by the attending physician. You should not listen to the advice of neighbors, acquaintances, comrades and other people incompetent in this matter. Everyone’s body is individual, and therefore the medicine is suitable for one and not for another. And the path of development of the disease is different for everyone.
The doctor conducts an examination, takes tests, conducts a survey and asks very important questions: are there any other concomitant diseases that could provoke a rise in blood pressure.
In order for alpha blockers to show a high positive effect and not cause side reactions, the patient should carefully monitor their diet. It is not recommended to overload the gastrointestinal tract with heavy, spicy, fried, smoked foods. The tablets must be taken either during meals or after. The dose and frequency of administration depend on the severity of the disease, the age of the patient, and the presence of concomitant pathologies.
To control pressure changes, it is recommended that all hypertensive patients, if possible, purchase personal blood pressure monitors. Daily blood pressure measurement and heart rate tracking are shown.
Both indicators are very important for the health of a hypertensive patient.
When planning a visit to the dental office or a planned operation, it is very important to notify the attending physician about the medications used.
Possible side effects
Alpha blockers are effective medications for the treatment of hypertension. In some cases, taking them can cause side effects:
- malaise, darkening of the eyes, heaviness in the head, lightheadedness;
- nausea reflex;
- nervousness, irritability;
- decreased sex drive;
- sleep disorders;
- discomfort in the abdominal area;
- increased sweating;
- tremor;
- sudden development of circulatory failure;
- malfunction of the digestive system;
- pathological increase in the lumen of blood vessels, which can cause fluid stagnation, migraine, and increased heart rate.
When starting to take alpha blockers for hypertension, there is a high risk of side effects.
Drugs containing the active ingredients prazosin and terazosin have a diuretic effect and also reduce the amount of iron-containing protein in the blood.
Important! A pronounced effect of taking alpha blockers for hypertension is observed upon first use. After a long period of use, the effectiveness of the drug decreases markedly.
Instructions for use
All adrenergic blockers have a similar mechanism of action, side effects and contraindications. Many of them are very popular, and some are prescribed with caution due to the unpredictable effect during treatment.
Features of the action of alpha-blockers
The action of this pharmacological group is aimed at relieving vasospasm and reducing the secretion of renin in the kidneys. After taking the drug, an antianginal effect appears, which is caused by a decrease in the frequency and strength of heart contractions. The antidiuretic effect is observed due to the relaxation of smooth muscle muscles. In this regard, the resistance to urine outflow decreases. Due to the blocking of alpha receptors, a persistent hypotensive effect occurs that lasts about a day.
When is medication indicated?
Indications for the use of alpha-blockers are the following diseases:
- benign prostatic hyperplasia. In this case, tamsulosin, doxazosin, setegis are prescribed. The same drugs are used for prostatitis, when there is compression of the lumen of the urethra by the prostate gland;
- arterial hypertension. In this case, drugs are prescribed to relieve acute attacks of high blood pressure. Since the drugs have a persistent antispasmodic effect, the effect of the drug lasts for a day. This ensures that the load on the blood vessels and heart is relieved for a long time;
- cardiovascular diseases, such as arrhythmia, heart failure, coronary heart disease, extrasystoles. In this case, there is a careful selection of drugs. The most commonly prescribed of them are: prazosin, alfuzosin, urapidil.
It is important to know! Some symptoms are similar to heart disease, however, they are caused by a disorder of the autonomic nervous system.
Contraindications for use
There are a number of contraindications that cannot be ignored, otherwise unwanted symptoms or damage to certain organs and systems may occur:
- Children under 18 years of age.
- Pregnancy and breastfeeding.
- Predisposition to hypotension.
- Hemophilia.
- Individual intolerance to components.
Other contraindications are indicated in the drug instructions. They may include additional items. Before use, read the instructions.
Use for cardiovascular pathologies
Cardiologists prescribe adrenergic blockers for left ventricular hypertrophy. In this case, they have a reverse effect. The use of drugs from this pharmacological group helps the patient cope with critically high blood pressure and saves him from stroke. The main effect of alpha blockers is aimed at dilating the ducts of the coronary vessels. Improved blood circulation while taking these drugs is a good prevention of ischemic heart damage and myocardial infarction.
Features of reception in urology
Alpha-1 adrenergic receptors are located in the tissues of the prostate gland and bladder, the action of which is inhibited when taking blockers. These medications are taken once a day every day. The initial dose is set by the doctor separately for each patient, depending on the damage to the genitourinary system. The drug is started with a minimum dose. Due to their vasodilating properties, alpha-blockers help fight poor urination and reduce pressure in the urinary canal. However, the effect does not occur immediately, but a couple of weeks after the start of use. Among the drugs used in urology, tamsulosin, doxazosin, and alfuzosin are prescribed.
Is it possible to combine
Can alpha-blockers be taken together with other drugs? You can take diuretics with drugs in this series. They activate the renin-angiotensin-aldosterone system and contribute to the retention of salt and water in the patient’s body.
The latter complement the therapeutic effect, promoting the development of a hypotensive effect. This combination of drugs gives an excellent effect! Reduces the negative impact of diuretics on lipid levels in the patient's blood.
β-blockers are also effective in combination with α-blockers. They complement each other. The latter reduce the level of impact of β-blockers on lipid levels. In turn, β-blockers help prevent reflex tachycardia, which can be caused by α.
List of medications in this group
Today, the following drugs are considered the best alpha-blockers:
- The drug "Alfuzosin". This medication is indicated for myocardial hypertrophy and prostatitis. It should be borne in mind that when taking it, people may experience shortness of breath, swelling of the arms and legs.
- The drug "Urapidil" has the same indications as the previous drug. It is also often prescribed for impotence in men. But it should be taken with caution, as it can lower blood pressure to critical values.
- The medicine Yohimbine is also taken for impotence in men. But while using it, problems with urination may occur.
- The drug "Nicergoline" is used for disorders of peripheral blood flow. This drug may cause sleep problems.
- The medicine "Phentolamine" is used in the presence of pathological processes in the soft tissues of the legs and arms. Side effects include that this medication can cause a fever.
- The drug "Proroksan" is prescribed to patients with advanced atherosclerosis.
Contraindications
There are a number of contraindications to the use of adrenergic blockers. First of all, this is the patient’s individual predisposition to these medications. For sinus block or sinus node syndrome.
If you have lung diseases (bronchial asthma, obstructive pulmonary disease), treatment with adrenergic blockers is also contraindicated. For severe liver diseases, ulcers, type I diabetes.
This group of drugs is also contraindicated for women during pregnancy and breastfeeding.
Adrenergic blockers can cause a number of common side effects:
- nausea;
- fainting;
- problems with stool;
- dizziness;
- hypertension (when changing position).
Mechanisms of action of these drugs
The key effect of alpha adrenergic blockers, as a rule, lies in their ability to interact with adrenergic receptors of blood vessels and the heart. They work in such a way that they seem to turn them off. Alpha adrenergic blockers interact with receptors instead of adrenaline and norepinephrine; as a result of such competitive contact, they can cause completely the opposite effect, which will consist of the following:
- Reducing the diameter of the lumen of blood vessels.
- Increase in blood pressure.
- More glucose enters the blood.
Today, there are various drugs based on alpha-blockers, which have general and highly specific pharmacological properties for this line of medications. It is obvious that different groups of blockers can have different effects on the body. There are also different mechanisms for their functioning.
Alpha blockers against alpha 1 and 2 receptors are primarily used as vasodilators. An increase in the vascular lumen leads to improved blood supply to the organ. As a rule, drugs in this category are intended to help the intestines and kidneys. When taking them, people's blood pressure normalizes, the amount of venous blood in the vena cava decreases (this indicator in medicine is called venous return), which reduces the load on the heart.
Medicines have become quite widely used for the treatment of sedentary patients and obese people. Alpha blockers can prevent the occurrence of reflex heartbeat. Here are a number of key effects on the background of the application:
- Unloading of the heart is achieved.
- Blood circulation is normalized.
- Shortness of breath decreases.
- Accelerates the absorption of insulin.
- The pressure in the pulmonary circulation decreases.
Classification of adrenergic blocking drugs
You may be interested in: Osgood-Schlatter disease: causes, symptoms and treatment
The taxonomy of adrenolytics, as a rule, is based on the type of adrenergic receptors that the blocker inhibits. Thus, we distinguish:
- Alpha blockers, which include alpha 1 and alpha 2 blockers.
- Beta blockers, including beta 1 and beta 2 blockers.
Adrenergic blockers are capable of inhibiting one receptor or several at once. For example, the substance pindodol can block beta 1 and 2 adrenergic receptors. Such adrenergic blockers are called non-selective. The substance esmolod acts only on the beta 1 adrenergic receptor. This adrenolytic is called selective.
A series of beta-blockers in the form of “Acetobutolol”, “Oxpenolol” and others have a stimulating effect on beta-adrenergic receptors. They are often prescribed to people suffering from bradycardia. This ability is called sympathetic internal activity, otherwise “ICA”. This terminology is mainly used by doctors.
Mechanism of pharmaceutical action on adrenergic receptors
There are two categories of fundamentally different medications:
- Stimulants that are adrenomimetics or agonists.
- Blockers acting as adrenolytics and adrenoblockers.
The effect of alpha 1 adrenergic agonists is based on the stimulation of adrenergic elements, as a result of which all kinds of changes occur in the human body. The list of these drugs includes Oxymetazoline, along with Ibopamine, Cocaine and Sydnofen.
The action of alpha-blockers is based on the inhibition of adrenergic receptors. In this case, adrenergic receptors trigger diametrically opposite changes. The list of these drugs includes Yohimbine, along with Pindolol and Esmolol.
Thus, adrenolytics, along with adrenergic agonists, are antagonistic substances. Next, we move on to consider the classification of this category of drugs.