What hurts when you cough?
The pain syndrome caused by coughing attacks can be defined by different levels of intensity and the nature of the pain: sharp or dull, localized or widespread, severe or moderate.
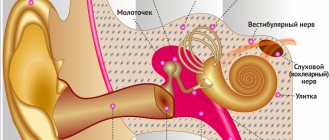
The location where the pain is detected may indicate the affected organ: in the throat, sternum, inside the chest, under the ribs or in the back, stomach, head. Very often, patients describe their sensations as pain in the lungs, but it is worth clarifying that there are no pain nerve endings in the lungs themselves. Cough, accompanied by pain, is a consequence of diseases of a very different nature.
Character of chest pain
The nature of chest pain differs into several types:
- pressing;
- piercing;
- aching.
The pain may be localized to a specific area or may be felt throughout the entire chest and radiate to the shoulder or arm. Aching, pressing or stabbing pain in the heart area occurs under various circumstances - when changing posture, during inhalation, with increased stress, or even at rest. In terms of duration, it can be short-term or long-term.
Causes of pain when coughing
Muscles
Overstrain of the muscle fibers responsible for the cough reflex can manifest as soreness and aching pain.
Throat
With pharyngitis, laryngitis, tracheitis, sore throat, the inflammatory process affects the mucous membranes of the upper respiratory tract. In these cases, while swallowing, talking and coughing, a person is bothered by unpleasant sensations in the throat: pain, stinging, soreness, dryness.
Bronchi and lungs
With colds, patients complain of a mild, painless cough, but if the infection spreads to the bronchi and lungs, the cough becomes more intense, accompanied by a burning sensation in the chest and pain in both the chest and back.
With tuberculosis and obstructive bronchitis, chest pain is provoked by the destruction of lung tissue and manifests itself when coughing.
Pleurisy is accompanied by pain and heaviness in the chest, usually on one side, the intensity of the pain varies depending on the position of the patient, and intensifies with deep breathing and coughing.
Heart and blood vessels
With pericarditis, the pain is localized in the left side of the chest. Pain can also be caused by arterial blockage, thromboembolism, unstable angina and acute heart failure.
Injuries
Blows and bruises received in the chest area can damage the ribs and muscle frame, causing painful spasms when inhaling.
Nervous system
If you feel discomfort in the chest without additional symptoms, you need to undergo a full examination to exclude diseases of the neuralgic type. They are usually accompanied by a dry cough due to irritation of the receptors.
Gastrointestinal tract
If the patient also complains of a burning sensation behind the breastbone, problems with swallowing food and saliva, as well as a bitter or sour taste in the mouth, then the problem may be reflux esophagitis (GERD), in which the lining of the esophagus becomes inflamed.
Kidneys
In case of kidney disease, cough may be accompanied by the discharge of blood. Cutting pain caused by the movement of stones during urolithiasis can radiate to the sternum and intensify when coughing.
Tumors
A severe, annoying cough, accompanied by sharp pain and shortness of breath, can be caused by pulmonary oncology. It is necessary to urgently visit a pulmonologist if there is pain accompanied by purulent sputum.
Pain in the heart area
Pain in the heart area is one of the most common symptoms and in frequency of occurrence can be compared only with headache. However, not all pain that we describe to the doctor as heart pain actually is. For example, the chest has a mass of nerve fibers and several large plexuses, when irritated, pain appears that is very similar to heart pain. However, pain in the heart area sometimes becomes the only complaint in various diseases. The causes of pain in the heart area can be both emergency conditions that require urgent treatment, and chronic diseases that last for years. Moreover, the cause of pain in the heart is not necessarily diseases of this particular organ. In this regard, pain in the heart area (which is often called simply chest pain) can be conditionally divided into true pain in the heart and cardialgia, which is a symptom of other diseases.
The first group includes angina pectoris, myocardial infarction, cardiac aneurysm, mitral valve prolapse, and other heart diseases in which the pain, although not acute, accompanies patients for a long time.
The second group includes diseases and conditions that may not be related to the heart, but cause cardialgia. Among these conditions it is worth mentioning osteochondrosis, hormonal disorders (thyrotoxicosis, hypothyroidism, menopause, etc.), features of the vegetative-vascular nervous system, which is sometimes called vegetative-vascular dystonia, neurological diseases, including neuroses, some lesions of the musculoskeletal system etc.
Coronary heart disease (CHD)
The most common cause of heart pain is coronary artery disease (CHD). This collective concept includes more than thirty diseases, the most common of which are angina pectoris and myocardial infarction. The main mechanism in the development of coronary heart disease is insufficiency of blood supply to the myocardium. At the same time, serious changes develop in heart cells (cardiomyocytes), experiencing an acute lack of oxygen and nutrients. If ischemia (a sharp decrease in blood supply) lasts more than 30 minutes, then these changes become irreversible, the cells die, which marks the onset of a heart attack.
Angina pectoris
Angina pain usually occurs as a result of physical or emotional stress. Typically, the pain associated with angina pectoris is squeezing, pressing or burning in nature. Often radiates (gives) to the left arm, shoulder blade, shoulder. These pains are very painful for the patient: it is not without reason that one of the characteristics of angina pain is the fear of death.
The pain of angina is quite easily relieved with nitroglycerin, which is its important distinguishing feature.
An attack of angina rarely lasts more than 10 minutes and goes away either on its own or after taking drugs that have the ability to dilate the blood vessels supplying the heart (the most famous among them is nitroglycerin).
For mild, short-lived attacks of angina, as well as to reduce heart pain caused by neurosis, validol is also used.
Myocardial infarction
Myocardial infarction is, in fact, the result of a prolonged attack of angina. But if changes in the heart during angina pectoris are still reversible, then during a heart attack necrosis of myocardial cells occurs. The pain characteristics of a heart attack are often no different from those of angina. Only their intensity can differ. Sometimes, with a heart attack, there is pain in the abdomen (abdominal form of heart attack). In some cases, myocardial infarction is accompanied by loss of consciousness, vomiting, and headache. As with angina, there is a fear of death.
Unfortunately, a clear relationship between the intensity of pain and a real threat to life is not always observed. Quite often, a heart attack is suffered on the legs, leading to complications. In some cases, a myocardial infarction may be an accidental discovery in a clinic, from where a seemingly healthy person is taken away by ambulance. This may be due to both individual characteristics of the body and irrational use of painkillers.
In their daily practice, doctors in specialized departments have the opportunity to use laboratory blood values to diagnose myocardial infarction. They appear when heart muscle cells are destroyed. At the same time, laboratory parameters increase depending on the increase in the area of damage to the heart muscle.
These tests are of particular importance in cases where the electrocardiogram data is inaccurate, it is not possible to repeat it several times, and other symptoms are not clearly expressed.
These markers are:
- Myoglobin is a muscle protein that appears in the blood during acute myocardial infarction. This indicator is one of the very first markers. Its level increases 2-4 hours after the development of myocardial infarction, and reaches maximum values 12 hours after the heart attack.
- Cardiac troponin is the “gold standard” for diagnosing acute myocardial infarction - a protein directly from the heart muscle. Its level rises 4-6 hours after the onset of acute myocardial infarction and lasts up to 10 days
- MB fraction of creatine phosphokinase. Its level increases within 3 hours after acute myocardial infarction, increases rapidly until the end of the first day and normalizes by the third day
That is, the “trio” of these three enzymes makes it possible to determine with very high accuracy the presence of damage to the heart muscle during myocardial infarction, begin treatment on time and reduce the risk of complications.
An important point in this state of affairs remains the low medical culture of the population and insufficient attention to their health. After all, any pain requires the attention of a doctor!
Mitral valve prolapse
For cardiology, mitral valve prolapse is a relatively new diagnosis. This is due to the introduction into practice of ultrasound examination of the heart - echocardiography. Prolapse is the excessive bending of the valve leaflets due to blood pressure in the heart. Normally, the closed leaflets of the mitral valve remain practically motionless when the phases of the cardiac cycle change. Valve structures are made of connective tissue. And it is the strength of this tissue that determines a person’s propensity for this condition.
For this reason, mitral valve prolapse is more often observed in people with increased flexibility in the joints, thin people, and with relatively thin bones. In other words, in people with more elastic connective tissue.
Mitral valve prolapse is often not accompanied by problems with the heart. Therefore, if the heart function is not impaired, then it does not require any special treatment. If mitral valve prolapse was detected in adolescents during a period of intensive growth, then it is necessary to repeat the study in order to make sure that the degree of mitral valve prolapse has not changed and the functioning of the heart is not impaired.
In some cases, the severity of mitral valve prolapse can be significant: through the “unclosed leaflets” of the valve, part of the blood is “thrown back”, which affects hemodynamics. And this is a more serious condition that requires the attention of a cardiologist, and sometimes, adjustments to the degree of physical activity.
With mitral valve prolapse, patients report vague pain in the heart. The pain is usually moderate, dull, bursting. Patients note interruptions in the work of the heart, freezing, although these complaints are not confirmed by the ECG. Quite typical complaints are headaches, fluctuations in blood pressure, fatigue, and decreased performance. As can be seen from this incomplete list, complaints to the doctor alone will not be enough. Only echocardiography will help in making a diagnosis, when in real time the doctor will see excessive protrusion of the valve into the atrium cavity, which gives the doctor the right to make a final diagnosis.
Extracardiac causes of heart pain
Very often doctors answer the question, “Why does the heart bother you?” ─ they answer: “Osteochondrosis of the spine is to blame” or “You have vegetative-vascular dystonia, this explains everything...”
These diagnoses are so common in the cards that a suspicion arises: is it really true that 80-90% of people who go to the doctor suffer from these mysterious diseases?! And can pain in the heart have the same causes as pain in the lower back, or dizziness with a headache?
Osteochondrosis
Osteochondrosis is a very common disease. And, indeed, it can cause all the conditions described above. The mechanism of occurrence of disorders in osteochondrosis is irritation of the nervous structures of the spinal cord. Thus, when these formations are affected at a certain level of the spine, completely definite pain sensations arise. Pain in the heart most often occurs when osteochondrosis affects the cervicothoracic region.
Pain in the heart with osteochondrosis does not have clear distinctive signs. More often it is an aching, dull pain that can radiate to the arm, neck, or chest. Accompanied by a change in skin sensitivity, the appearance of a feeling of “crawling goosebumps”, etc.
The appearance of pain in the heart mainly in the evening hours may also indicate osteochondrosis, since the spine in the evening “shortens” somewhat under the weight of the body, and this contributes to compression (compression) of the nerves and vessels of the spine.
It is worth emphasizing that in order to fully exclude (or confirm) osteochondrosis as the cause of pain in the heart, it is worth performing an examination of the spine (x-ray, CT, MRI). As a rule, this allows the doctor to accurately imagine the role of osteochondrosis in the occurrence of cardialgia.
Vegetative-vascular dystonia (VSD)
Another cause of heart pain may be vegetative-vascular dystonia. True, this diagnosis even among doctors causes a lot of disagreement, despite its prevalence. In fact, it should be understood that the vessel is the same organ as all the others, therefore its work, like the work of muscles, is regulated by the nervous system. The only difference is that the regulation mechanism is different ─ it cannot be influenced by willpower.
It is also extremely difficult to notice changes in the regulation of the vessels that supply blood to the heart muscle: they can only be judged by indirect signs, the same ones that bring people to the doctor: pain, anxiety, etc.
Pain in the heart due to disorders that some doctors call vegetative dystonia most often does not have a clear localization. Patients complain of bursting, pressing pain in the heart area. The pain is usually dull and aching, often spreading to the left arm, causing discomfort in it. Often concerned about inadequate sleep, increased fatigue, motion sickness in transport.
It is characteristic that such patients are often helped by drugs that do not have a direct effect on the cardiovascular system. This could be a hot drink, a bath, menthol or mint. For some, pain is relieved by eating or resting.
Sometimes the help of a psychotherapist and taking sedatives that “put in order” the nervous system help cope with the pain.
Hormonal disorders
The hormonal (or endocrine) system is an important link in regulating the functioning of the entire body. Its importance is no less than the role of the nervous system. That is why any disruption in the endocrine system can provoke pain in the heart. However, most often cardialgia causes changes in the thyroid gland and adrenal glands.
First of all, it is worth mentioning thyroid hormones. Both excess and deficiency of the hormones T3 and T4 can provoke heart pain. An excess of these hormones causes a significant increase in heart rate and intensification, which requires increased blood supply to the heart. This is why the heart becomes more sensitive to oxygen deficiency, which can manifest itself in the form of typical angina attacks.
With a decrease in the synthesis of thyroid hormones, there is a decrease in the rate of all metabolic processes. The body falls into a kind of “sleep mode”, reducing resource consumption. In such conditions, the heart is also at risk of a deficiency of nutrients and oxygen, since it, also being “in hibernation,” is obliged to supply blood to all organs and tissues of the body.
Adrenal hormones also have a pronounced effect on the heart. For example, excess adrenaline observed with an adrenal tumor (pheochromacytoma) causes a sharp increase in heart function, increases blood pressure and, if left untreated, leads to uncontrolled hypertension and its complications - angina pectoris, heart attack, stroke.
Heart and female hormones
Estrogens play a major role in a woman’s body. These hormones protect the heart from negative influences, i.e. have proven cardioprotective properties. This fact explains the significant difference in the incidence of heart disease in women under 50 years of age than in men.
It is significant that with the onset of menopause this difference practically disappears. This is why many menopausal women often complain of heart pain. A woman’s complaints during this period should be especially carefully considered by a doctor: in the case of severe symptoms of menopausal disorders, hormonal correction is successfully used, which eliminates not only discomfort in the heart, but also many complaints, and provides milder changes in the woman’s hormonal levels.
Heart pain: what else you need to keep in mind
Many of us have quite a lot of experience communicating with people who are unsuccessfully trying to get rid of heart pain. Very often, even a full examination does not give the expected results. After all, the concept of normal for the laboratory and for the patient may sometimes differ. After all, it happens that the test results are quite good, but there is pain in the chest... This is how the mysterious diagnosis “unexplained pain in the heart” appears. Few specialists undertake to treat them, since it is impossible to guarantee any success of therapy!
For this reason, such patients are at the highest risk of being “treated” in the hands of alternative medicine practitioners and simply charlatans. And the wave-like nature of the complaints gives confidence in the effectiveness of the imaginary treatment. You can always blame the patient himself for deterioration.
In such cases, it is much more effective to consult a psychoneurologist. Since pain in the heart caused by a violation of the nervous regulation of blood vessels, in many cases disappears after adjusting the functioning of the nervous system (neurocirculatory dystonia, the more accurate scientific name of vegetative-vascular dystonia).
On the other hand, patients themselves can rarely boast of a healthy lifestyle. That is why, in cases of heart pain that cannot be explained with the help of a cardiologist, it is more rational to begin treatment with lifestyle correction - healthy nutrition, water, rest, air, sun, adequate physical activity.
These simple, naive truths “from childhood” only bring an ironic smile to many. It is much easier for us to shift responsibility for our health to our “bad” medicine.
Treatment of painful cough
We remind you that in order to prepare competent treatment, you need to contact a general practitioner, who will refer you to a specialist (otolaryngologist, phthisiatrician, cardiologist, neurologist, etc.) for a full examination. Selecting your own medications and abusing painkillers can be dangerous to your health and lead to complications.
- If the pain is of an infectious-inflammatory nature, antibacterial, antiviral therapy, or treatment with other drugs may be prescribed, depending on the causative agent of the infection and the location.
- For the symptomatic treatment of cough, drugs are first prescribed that promote sputum separation and convert a dry cough into a productive one.
- In rare cases, medications may be prescribed to suppress coughing attacks, but this may slow down the healing process.
- If the cause of pain is identified as pleurisy or pericarditis, then a puncture of the pulmonary or cardiac membrane is prescribed to relieve the corresponding organs.
- For GERD, antacids and medications that help reduce the acidity of gastric juice may be prescribed.
- Pinched nerve endings localized in the sternum area can be relieved with painkillers and sedatives.
Chest pain due to sprains, intercostal neuralgia and injuries
With intercostal neuralgia, which manifests itself as a result of muscle spasm, the nerve roots are compressed, and a sharp pain occurs in the chest, radiating to the back.
Chest pain can also be caused by damage to the pectoral or back muscles - sprains, tumors (rhabdomyoma), inflammation (myositis).
Pain from bruises, fractures or cracked ribs can also be mistaken for heart pain. However, by the location of the source of pain, it can be determined that it is not the heart that is hurting.
If you have chest pain or heart pain, contact our clinic. Experienced doctors will make the correct diagnosis and prescribe a course of treatment.
Bromhexine for pain
Bromhexine is prescribed for the rapid removal of mucus from the respiratory tract in various diseases of the respiratory system: bronchitis, pneumonia, ARVI and influenza, asthma, pneumoconiosis. Bromhexine does not have an analgesic effect, it alleviates respiratory symptoms and helps get rid of an unproductive painful cough that can cause pain.
For other causes of cough (cardiac, gastric, neurological), the use of bromhexine and other mucolytics is ineffective.