Warfarin
Monitoring
A prerequisite for therapy with Warfarin is the patient's strict adherence to the recommended dose of the drug.
The target INR value for oral anticoagulant therapy to prevent thromboembolic complications in patients with prosthetic heart valves is 2.5-3.0; for other indications - 2.0-3.0.
Patients suffering from alcoholism or dementia may be unable to adhere to the prescribed regimen of Warfarin.
Factors influencing the effect of warfarin
In conditions such as fever, hyperthyroidism, decompensated heart failure, alcoholism with concomitant liver damage, the effect of Warfarin may be enhanced. Increased effects of warfarin, requiring dose reduction, may also occur with weight loss, acute comorbidities, and smoking cessation.
The effect of warfarin may be reduced in hypothyroidism. A decrease in the effect of warfarin, requiring an increase in the dose of the drug, is possible with weight gain, as well as with diarrhea and vomiting.
Patients with a mutation of the gene encoding the CYP2C9 isoenzyme
Patients with a mutation in the gene encoding the CYP2C9 isoenzyme have a longer T1/2 of warfarin. These patients require lower doses of Warfarin, since the risk of bleeding increases when using normal therapeutic doses. If it is necessary to achieve a rapid antithrombotic effect, it is recommended to begin therapy with the administration of heparin; then, for 5-7 days, combination therapy with heparin and warfarin should be carried out until the target INR value is maintained for 2 days (see section "Dosage and Administration").
In the case of rare individual resistance to warfarin (extremely rare), 5-20 loading doses of Warfarin are required to achieve a therapeutic effect.
If the use of Warfarin in such patients is ineffective, other possible reasons should be identified, for example, concomitant use of other drugs (see section “Interaction with other drugs”), inadequate diet, laboratory errors.
Calciphylaxis
Calciphylaxis is a rare syndrome characterized by calcification of blood vessels with skin necrosis and is associated with high mortality. This complication is mainly observed in patients with end-stage renal disease on dialysis, or in patients with known risk factors such as protein C or S deficiency, hyperphosphatemia, hypercalcemia, or hypoalbuminemia. Rare cases of calciphylaxis have been described when taking warfarin in patients who do not have kidney disease. If calciphylaxis develops, appropriate treatment should be initiated and discontinuation of warfarin therapy should be considered.
Thrombophilia
Patients with protein C deficiency are at increased risk of developing skin necrosis when starting warfarin. In patients with protein C deficiency, treatment with warfarin should be initiated without a loading dose, even if heparin is used concomitantly. With protein S deficiency there is also a risk of skin necrosis, so it is advisable for such patients to start warfarin therapy with low doses.
Ischemic stroke
Anticoagulant therapy after ischemic stroke increases the risk of secondary hemorrhage in the necrotic area of the brain. In patients with atrial fibrillation, long-term use of warfarin is beneficial. However, the risk of early recurrence of embolism is low, so temporary cessation of therapy after an ischemic stroke is advisable. Warfarin treatment should be restarted 2 to 14 days after an ischemic stroke, depending on the size of the infarction and blood pressure. In patients with major embolic stroke or uncontrolled hypertension, warfarin should be discontinued for 14 days.
Surgical interventions
Surgeries not associated with the risk of severe bleeding can be performed with an INR < 2.5. If there is a risk of serious bleeding, warfarin should be discontinued 3 days before surgery. If it is necessary to continue anticoagulant therapy (for example, with a high risk of life-threatening thromboembolic complications), the INR should be reduced to <2.5 and heparin therapy should be started (see section "Dosage and Administration").
If surgery is necessary and warfarin cannot be stopped 3 days before surgery, the anticoagulant effect of warfarin should be stopped with low-dose vitamin K supplements.
The timing of resumption of warfarin therapy depends on the risk of postoperative bleeding. In most cases, warfarin can be restarted as soon as the patient can take the tablets by mouth.
Dental procedures
You should not stop taking warfarin before routine dental procedures (for example, before a tooth extraction).
Renal dysfunction
In chronic renal failure or nephrotic syndrome, the concentration of the free fraction of warfarin in the blood plasma increases, which, depending on concomitant diseases, can lead to either an increase or decrease in the effect. In cases of moderate renal failure, the effect of warfarin is enhanced. Caution is recommended when using warfarin in patients with impaired renal function. In all of the above conditions, careful monitoring of INR values should be carried out.
Thyroid diseases
The rate of warfarin metabolism depends on the functional state of the thyroid gland. Therefore, patients with hyper- or hypothyroidism require careful monitoring when initiating warfarin therapy.
Elderly patients
Treatment of elderly patients should be carried out with caution, because the synthesis of blood coagulation factors and hepatic metabolism in such patients is reduced, as a result of which the effect of warfarin may be enhanced.
In what situations is this examination prescribed?
This examination is prescribed during treatment with indirect anticoagulants - vitamin K antagonists (neodicoumarin, warfarin, syncumar), which reduce the level of prothrombin in the blood, thus thinning it.
Regular monitoring of the indicator allows you to control the dosages of the above drugs to avoid bleeding or blood clots.
When is it necessary to take indirect anticoagulants?
In what situations is it necessary to regularly take a blood test for INR and prothrombin?
- Treatment and prevention of thrombosis of the superficial and deep veins of the lower extremities;
- Varicose veins;
- Acute coronary syndrome;
- Cerebrovascular accident in the acute stage (ACVA);
- PE (pulmonary embolism);
- Permanent form of atrial fibrillation;
- Heart disease;
- Thrombophlebitis;
- The presence of artificial valves in the heart;
- The presence of a vena cava filter (a filter in a large vein of the body that prevents thrombotic masses from entering the veins of the lower extremities and pelvic organs to the heart and lungs.
It must be remembered that when using warfarin and other anticoagulants, the INR level is increased and should be kept within the range of 2.0 - 3.0 (the optimal value is 2.5), and with prosthetic heart valves from 2.5 to 3.5. Patients with an INR value above 6.0 require urgent treatment.
If a person is not treated with anticoagulants, then a deviation of the INR from the norm can cause serious pathological changes in the body. Let's consider in what situations the level of this indicator may change.
Blood coagulation system
Blood clotting is a vital device that protects the body from blood loss.
However, in some cases, with disturbances in the hemostatic system, it can become pathological. Normal blood thickness is ensured by the coordinated functioning of two systems: coagulation and anticoagulation. Its fluid state is regulated by anticoagulation mechanisms, and thrombus formation by coagulation mechanisms. When the balance between them is disturbed, a person has an increased tendency to bleed or form blood clots (thrombi).
One of the most significant indicators of a coagulogram, reflecting the state of the coagulation system, is a complex protein - prothrombin. It is also called coagulation factor II. It is formed with the participation of vitamin K in the liver. It is by the indicators of this protein, which is a precursor of thrombin, that the doctor can assess the state of the coagulation system and the patient’s tendency to bleeding or thrombosis.
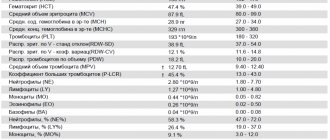
Determination of the level of prothrombin in the blood can be carried out using the following methods:
- PTT (prothrombin time);
- prothrombin level according to Quick;
- PTI (or prothrombin index);
- INR.
In everyday clinical practice, doctors most often prescribe PTI or INR tests, since they most reliably reflect the state of the coagulation system.
Decreased INR level
There is also the opposite condition - hypercoagulation, in which the blood thickens. This condition is dangerous due to blood clots that can block blood vessels leading to vital organs.
- INR blood test - what is it. Norm and interpretation of INR blood test in adults and children
Then such severe conditions as pulmonary embolism (thromboembolism), myocardial, kidney, spleen, intestinal infarction, acute ischemic cerebrovascular accident occur.
Typically, INR levels decrease when:
- dehydration of the body (rapid loss of fluid without its replenishment) - when taking diuretics, burns, impaired permeability of the walls of blood vessels, when fluid leaks out of them into the surrounding tissues, and cellular elements remain in the channel;
- hereditary deficiency of antithrombin III;
- when taking hormonal drugs (especially oral contraceptives);
- infectious diseases accompanied by a significant increase in temperature;
- malignant neoplasms;
Also, indicators may be low due to technical errors during blood sampling or analysis.
Indications for prescribing INR
A blood test for INR is prescribed for certain indications. The normal range of this test varies depending on the underlying disease of the patient.
Indications:
- Preoperative examination of patients. The norm is closer to 1 (from 0.7 to 1.3, usually 0.85-1.25).
- Taking blood thinners (such as Warfarin). The norm is 2.0-3.0.
- Therapy for pulmonary embolism. The norm is 2.0-3.0.
- Condition after aortic valve replacement with a mechanical implant. The norm is 2.0-3.0.
- Condition after mitral valve replacement with a mechanical implant. The norm is 2.5-3.5.
- Preventive treatment of pulmonary embolism for heart defects. The norm is 2.0-3.0.
- Preventive treatment of deep vein thrombosis after surgery. The norm is 2.0-3.0.
INR analysis for patients taking blood thinners is carried out at certain intervals, which are determined individually by the doctor. At the beginning of the disease, when the patient is in the hospital, such tests are performed daily. Next, the patient is recommended to monitor the INR once a week and, if the test results are stable, then the frequency of tests can be reduced to once every 2-3 weeks.
The following changes in the patient’s life or symptoms of hypocoagulation may be the reason for prescribing an extraordinary test:
- long-term cold or other illness;
- changing the concomitant therapy regimen;
- lifestyle or diet changes;
- sudden climate change;
- unmotivated nosebleeds;
- bleeding gums;
- causeless appearance of hematomas;
- blood in urine:
- prolonged and heavy menstruation in women;
- streaks of blood in sputum or vomit;
- blood in stool (or tarry stool);
- prolonged bleeding from cuts;
- unexplained lumps, pain and swelling in the joints while taking a blood thinner.
Complexes with this research
Extended coagulogram Extended study of the functional state of hemostasis 2,460 ₽ Composition
For those at risk of COVID-19 Diagnosis of diseases complicating the course of coronavirus infection 2,430 ₽ Composition
Expanded hospital complex Expanded infectious screening for prevention and hospitalization 4,270 ₽ Composition
IN OTHER COMPLEXES
- Risk of severe COVID-19 630 RUR
- Men's check-up No. 1 RUB 10,930
- Examination during pregnancy. 1st trimester 9,770 RUR
- Women's check-up No. 1 RUB 11,530
- Preventive check-up RUB 6,530