How does lipemia interfere with testing?
Lipemia can interfere with blood tests in several ways:
- Increases light absorption. Because of this, the results of spectrophotometric analysis, which are used during biochemical blood tests, are distorted. The accuracy of studies that use light with a short wavelength suffers especially severely. The device determines the concentrations of some substances, for example, ALT, AST, bilirubin, incorrectly.
- Lipoproteins prevent antibodies from binding to antigens. As a result, the results of immunological tests are distorted. Depending on the nature of the reaction, they can turn out to be false positive and false negative.
- Distorts the results of studies in which the method of capillary electrophoresis of whey proteins is used. For example, it was noted that when analyzing blood with lipemia, the alpha-2-globulin fraction changes.
- Leads to heterogeneity of plasma and serum after centrifugation. In a centrifuge, VLDL, due to its low density, accumulates in the upper layer. Accordingly, there will be very few substances that are soluble in water. During analysis, their concentration will be incorrectly determined as low. At the same time, steroid hormones and some drugs accumulate in the upper lipid layer, and their concentration will be low in the lower part of the tube.
- Leads to the effect of volume displacement. Normal blood plasma consists of 92% water and 8% lipids. With lipemia, these figures can be 75% and 25%, respectively. But electrolytes are dissolved only in plasma, they are not in lipids. If the laboratory uses methods that determine the level of electrolytes in the total volume (indirect potentiometry, flame photometry), then their concentration will be lower than it actually is.
- With lipemia, hemolysis occurs more strongly - the destruction of red blood cells and the release of hemoglobin from them. This also interferes with the analysis and affects its accuracy. It is not entirely clear why lipids lead to this effect; it is believed that they act on the wall of red blood cells during the processing and centrifugation of blood as detergents (surfactants).
References
- ESC/EOA Clinical Guidelines for the Diagnosis and Treatment of Dyslipidaemias, 2021.
- Russian recommendations VI revision. Diagnosis and correction of lipid metabolism disorders for the prevention and treatment of atherosclerosis, 2021.
- NCEP Expert Panel on detection, evaluation and treatment of high blood cholesterol in adults. Executive summary of the third report of the National Cholesterol Education Program (NCEP) Expert Panel on detection, evaluation and treatment of high blood cholesterol in adults (Adult Treatment Panel III). JAMA 2001;285:2486–2497.
Blood viscosity and hematocrit indicators
To study the problem of blood viscosity, you should focus on normal values.
- 1048-1066 are normal values that determine blood density. This indicator should not go beyond this framework. It determines the level of salts, protein components and blood elements.
- 1092-1095 are indicators of the normal specific gravity of red blood cells.
- 1024-1050 are indicators of normal plasma density.
- 40-54% is a normal hematocrit level for men.
- 37-47% is a normal hematocrit level for women.
- 4.0-5.5 is a normal level of blood viscosity.
The more red blood cells there are in the blood, the higher the blood viscosity will be. The fewer red blood cells there are, the lower the blood viscosity will be.
If a person drinks too much, or fluid is retained in his body due to kidney disease, then the viscosity of the blood will be below the permissible normal limits. A similar situation develops against the background of bearing a child, with anemia, and when undergoing therapy with certain medications (Aspirin, Heparin). The lower the density of the blood, the faster its flow through the vessels. The higher the blood density index, the slower the blood flow rate. This can lead to the development of many pathologies of the heart and blood vessels.
Diagnosis of various blood readings is carried out in different ways:
- A viscometer is used to determine blood viscosity.
- The method of immunoelectrophoresis determines which proteins are present in the blood.
- Immunochemical methods make it possible to calculate the amount of these proteins.
How do laboratories detect lipemia?
Lipemia can be seen with the naked eye. The blood of such patients appears cloudy. This method is not reliable. Lipemia can be noticed only if the concentration of triglycerides is very high: in the supernatant - more than 3.4 mmol/L, in whole blood - more than 11.3 mmol/L. This is very subjective; not every laboratory technician can examine the changes that are recorded using special tests.
Many laboratories test for triglyceride concentrations. This method makes it possible to indirectly judge the presence of lipemia and, in combination with determining the L-index (more about it below), judge its cause. But this study has two shortcomings:
- The content of triglycerides in different types of lipoproteins varies: for example, in VLDL it is about 50%, in chylomicrons – up to 85–90%.
- In most of these assays, triglyceride concentration is inferred from the oxidation of glycerol to dihydroxyacetone phosphate. The more triglycerides, the faster glycerol oxidizes. If there is a lot of glycerol in the sample, a false positive result will be obtained. Such cases are known in patients with certain genetic disorders, among lovers of beer that contains glycerin.
Currently, automatic determination of the L-index is most often used. The essence of the method is that a blood sample is diluted in saline or a special buffer solution and the absorption spectrum of light of a certain wavelength (300–700 nm) is measured. The more lipids in a sample, the more it absorbs light.
Automatic determination of the L-index is a fast, inexpensive and fairly accurate method for detecting lipemia. But it also has some disadvantages. You can get a false positive result when the blood plasma is cloudy due to the content of other substances, for example, paraprotein (an “incorrect” immunoglobulin protein that appears in the blood in some diseases), contrast dyes that are used during some medical procedures.
Test systems for automatically determining the L-index are produced by different manufacturers; there is no single standard, and this makes it difficult to interpret the analysis results. Thus, errors are also possible when using this method, although they are rare.
Detailed description of the study
The study is important to study the distribution, volume and type of fats. Very low and low density lipoproteins (LP) belong to the atherogenic fraction, and high density lipoproteins help prevent atherosclerotic changes in blood vessels.
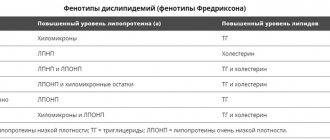
Atherogenicity index – the ratio of low- and high-density drugs. This indicator determines the risk of developing atherosclerosis and coronary heart disease. Triglycerides are lipids that are significant for the diagnosis of lipid metabolism disorders - hyperlipidemias, which are divided into five types and differ in origin, pathogenesis and therapy used.
Determining the level of various cholesterol fractions plays an important role in diagnosing cardiovascular pathologies, determining patient management tactics, predicting the development of complications, and monitoring treatment.
Complications
High blood viscosity syndrome is not a disease, but in the presence of serious pathologies it can cause severe and dangerous complications. More often, blood thickens in older people, but in recent years this syndrome has been increasingly detected in middle-aged and young people. According to statistics, thick blood is more often observed in men.
The most dangerous consequences of hyperviscosity syndrome are a tendency to form blood clots and thrombosis. Usually small vessels are thrombosed, but there remains an increased risk that the clot will block a coronary artery or cerebral vessel. Such thromboses cause acute tissue necrosis of the affected organ, and the patient develops myocardial infarction or ischemic stroke.
- What is dangerous about thick blood, causes and treatment for men, women and children
Other consequences of thick blood may include the following diseases and pathological conditions:
- hypertonic disease;
- atherosclerosis;
- bleeding;
- intracerebral and subdural bleeding.
The degree of risk of complications of hyperviscosity syndrome largely depends on the underlying cause of its development. That is why the main goal of treating this condition and preventing its complications is to eliminate the underlying disease.