It has long been known that a person’s internal biological clock regulates sleep and the functioning of all body systems. They synchronize with the light-dark cycle and are regulated by a special protein that accumulates at night and is used up during the day. When the phase of biological rhythms shifts, a person becomes hostage to disruption of circadian rhythms. Experiences a constant need to get a dose of sleep during the day and sleeps poorly at night. This condition leads to difficulties in living at a normal pace of life, decreased concentration, and requires urgent treatment from a somnologist.
What is circadian rhythm
Almost every cell of the human body is involved in biological processes that repeat cyclically throughout the day. Under the influence of special proteins, there is a timely activation of the synthesis of hormones for falling asleep, and an increase in blood pressure for awakening. It has been proven that appetite and brain activity depend on circadian rhythms.
The intensity of biological processes is affected by the duration of daylight and darkness. Information about the change of day and night is processed by a special part of the brain, receiving a signal through the retina. Today it is known that not only external factors are responsible for biorhythms. There is a section of DNA in the body that controls the human biological clock.
The circadian system is individual - everyone has their own time of falling asleep and waking up. When the “genetic clock” fails, the body adapts to new conditions. As a result, disorders arise that cause sleep disturbances, deterioration of well-being and a high risk of developing diseases.
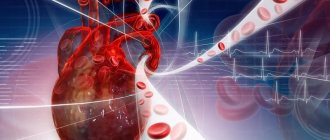
Synchronization of the molecular clock of cardiac muscle cells with lipid metabolism
We have already talked about how important it is to synchronize heart rhythms with the cycles of other physiological systems of the body. It is equally important to note that some internal cycles are capable of imposing their rhythm on the heart clock. One of these master cycles is the daily rhythm of the circulation of fatty acids and lipid levels, which is tightly linked to the circadian one. Fatty acids are the primary “heart fuel”: 70% of them are utilized by the heart. With an excess of fatty acids, the contractile function of the heart is suppressed, and the heart responds to these changes in the internal environment by activating both oxidative (mitochondrial) and non-oxidative metabolism. In this way, the heart reduces cellular toxicity caused by fatty acid loading. And this process is also associated with the daily rhythms of gene expression.
American researcher Molly Bray studied circadian clock genes using DNA microarray technology. She was able to identify 548 genes that regulate the clock in atrial cardiomyocytes and 176 genes associated with the circadian rhythm of ventricular muscle cells. These included genes involved in lipogenesis and lipid binding proteins; all of them showed diurnal expression [8].
How does jet lag manifest itself?
The main symptom of circadian disorders is a person's inability to fall asleep or wake up at a certain time. Lack of sleep leads to:
- to inattention;
- increased daytime sleepiness;
- lack of clarity of thinking;
- difficulty performing usual activities during the day;
- irritability, aggression;
- chronic fatigue, depression.
Sleep disturbances are accompanied by attacks of nausea and general malaise. Failure of biological rhythms threatens deterioration of heart function and the appearance of metabolic disorders.
Very often, in order to stay awake or, conversely, fall asleep, patients uncontrollably use sleeping pills and alcohol. But this behavior only makes the situation worse. If such signs appear, there is no need to try to cope with the problem on your own; it is correct to contact a specialist at a sleep medicine clinic.
Treatment
Treatment of the underlying pathological process is carried out. The circadian index should not be specifically normalized. Yes, and there is no such possibility. Contractility needs to be increased.
Treatment is mainly conservative, with the use of medications to relieve symptoms and combat the etiological factor. Both problems are solved at once.
What drugs are prescribed:
- Antiarrhythmic. Amiodarone or Quinidine. To restore normal heart rate and intervals between contractions. Used in short courses, it is not used on an ongoing basis due to the significant danger and mass of side effects.
- Antihypertensive. As needed. ACE inhibitors, calcium antagonists, centrally acting agents, diuretics with a mild, potassium-sparing effect. The names are selected by the doctor. With illiterate therapy, rapid development of heart failure and death of the patient in the short term is possible.
- Beta blockers. They help lower blood pressure and stop tachycardia. Increased frequency also occurs, but less frequently. If the normal functioning of the heart is disrupted, such as bradycardia, they are never prescribed.
- Cardiac glycosides. If there are no symptoms of coronary insufficiency, ischemia of cardiac structures.
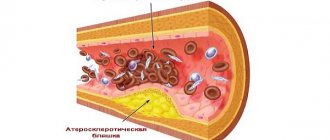
If necessary, statins are also indicated to dissolve cholesterol plaques and eliminate excess low-density lipids. Antiplatelet agents, special agents for normalizing the rheological properties of blood and preventing the formation of blood clots.
The operation is prescribed in extreme cases, strictly according to indications. These are considered to be heart defects. Congenital and acquired. Aortic, mitral, tricuspid valves, the vessels themselves, during the formation of aneurysms and other conditions.
Up to the destruction of chambers, for prosthetics or mechanical expansion of arteries (stenting, ballooning), creating bypass paths of blood flow (bypass surgery).
Radiofrequency ablation is possible for blockades of the conduction system (cauterization of an excessively active area).
The choice of the optimal direction of therapy is decided at the discretion of the doctor. The patient is instructed to limit himself for the rest of his life. But these are reasonable limits that will not cause much discomfort.
Quit smoking, alcohol, no drugs, no anti-inflammatory drugs without a doctor’s prescription, less fatty and fried foods in the diet. Get adequate sleep and at least minimal physical activity.
This is quite enough. Not a high price to pay for health, and possibly life.
Types of violations
There are several types of disorders:
| Variety | Peculiarities |
| Jet lag syndrome | Appears when fast moving across 2 or more time zones. According to the observations of somnologists, a person’s transfer to an earlier time is worse tolerated than a few hours ahead. |
| Distress related to changes in work schedule | A forced change in daily routine leads to disruption of the circadian rhythm. |
| Sleep phase delay syndrome | With this disorder, patients regularly fall asleep and wake up at late hours, and a steady shift in sleep phase is observed. |
| Phase advance sleep | This is the name of the condition when the biological clock is “in a hurry.” A person goes to bed early and gets up early, but he cannot change his wakefulness on his own. |
| Non-circadian sleep-wake cycle mode | Characterized by a daily change in the cycle by 1-2 hours, it is observed in blind people. |
Peripheral clocks in vascular muscle cells
The smooth muscle cells of blood vessels - myocytes - also have their own peripheral clock. Takishige Kunieda studied the circadian system in aging vascular myocytes. He found that in these cells, the loss of circadian rhythmicity is associated with telomere shortening. The introduction of telomerase prevented problems with the expression of clock genes. These studies suggest that telomerase regulation may be one of the therapeutic options for age-related circadian rhythm disorders [11].
Causes of Circadian Rhythm Disorder
A shift in the rhythm of the biological clock in relation to the light-dark cycle is provoked by internal and external factors. The latter include:
- moving across several time zones (air travel from West to East);
- permanent work with irregular work schedule;
- lack of a routine when a person falls asleep and wakes up at different times;
- long bed rest;
- total visual impairment;
- taking medications.
Sleep disorders are often observed in hospitalized patients with frequent periods of wakefulness at night.
Pathological causes of failure of the circadian system:
- brain damage after injury, stroke;
- Alzheimer's disease, Parkinson's disease;
- encephalitis, meningitis;
- mutation of the circadian clock gene CRY 1;
- age-related changes.
Hereditary predisposition plays a major role when a person’s individual “genetic clock” is “fast” or “lagging behind.”
Peripheral clock in endothelial cells
Several groups of scientists have demonstrated the role of clock genes in the function of the endothelium, the tissue lining the inside of blood vessels and the heart. They found that in mice with a mutation in the Per 2 clock gene, blood vessels do not relax in response to the influence of the main relaxing neurotransmitter, acetylcholine. In addition to this very unpleasant dysfunction, a very high concentration of substances that stimulate vascular compression is detected in the blood of mice, which is fraught with the occurrence of arterial hypertension [9].
But the health problems for the unfortunate mice did not end there. Researcher Chao Wang showed that if endothelial cells have a mutation of the Per 2 gene, then blood vessels quickly age, are poorly restored after damage, and the life expectancy of rodents themselves is greatly reduced [10].
How are circadian disorders treated?
Our center’s somnologists have extensive experience in correcting circadian rhythms, including managing non-standard cases of the disease. The list of therapeutic measures in most cases is individual.
Basic therapy includes:
- Phototherapy with sunlight. This is not always associated with exposure to the sun; fluorescent lamps are also used to correct the circadian system. When you need to stay awake, experts recommend being in bright light. Before falling asleep, carefully darken the room, curtain the windows with thick curtains, and put on glasses with dark lenses before going to bed.
- Regularly performing a set of simple physical exercises helps set your internal biological clock.
- The synchronization of biorhythms with the daily period is affected by food intake. Therefore, it is important to establish a proper diet. Most of the diet is recommended to be consumed in the morning and afternoon. In the evening, the serving size is reduced.
- If, after changes in behavior, symptoms of circadian rhythm disorder persist, the somnologist prescribes drug therapy. The effective dosage, frequency and duration of use of the drug is determined by the doctor, taking into account concomitant diseases.
During the elimination of circadian disorders, patients at the South Clinic are under the close supervision of a competent specialist who promptly assesses changes and, if necessary, adjusts prescriptions.
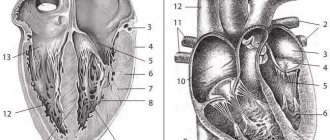
Types of arrhythmias
Most people by arrhythmia mean erratic contractions of the heart muscle (“the heart beats as it wants”). However, this is not quite true. The doctor uses this term for any disturbance of cardiac activity (decreased or increased heart rate), so the types of arrhythmias can be presented as follows:
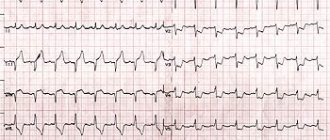
- Sinus arrhythmia, which may be associated with cycles of respiratory activity (increased rhythm during inhalation and slower rate during exhalation) or occur independently of breathing, but indicate some kind of cardiovascular pathology (coronary artery disease in old age) or be a consequence of autonomic dysfunction, for example, in teenagers. This type of arrhythmia is harmless and does not require special treatment measures. The ECG shows a difference between cardiac cycles (> 0.05 s).
- Sinus tachycardia is diagnosed if the heart rate exceeds 90 beats/min, of course, for no apparent reason (running, exercise, excitement). Typically, with such tachycardia, the heart rate does not exceed 160 beats per minute under calm conditions, and only during intense exercise can it reach up to 200 beats. It is caused by many factors associated with pathological processes in the body, therefore the treatment of such tachycardia is aimed at the underlying disease.
- Sinus bradycardia is characterized by a regular but slow sinus rhythm (less than 60 beats/min), associated with a decrease in the automaticity of the sinus node and resulting from excessive physical exertion (in professional athletes), pathological changes (not necessarily cardiovascular, for example, peptic ulcer). ), taking certain medications (digitalis, antiarrhythmic and antihypertensive drugs). Therapy is also aimed at eliminating the cause that caused bradycardia, that is, the underlying disease.
- Extrasystoles that occur with premature excitation and contraction of one part of the heart or all of them at once, therefore, depending on where and in what place the impulse was formed that disrupted the normal sequence of heart contractions, extrasystoles are divided into atrial, ventricular and those coming from the atrioventricular node. Extrasystolic arrhythmia is dangerous if it is group, early and frequent, since it poses a threat to hemodynamics, and as a result can “develop” into ventricular tachycardia or ventricular fibrillation, which will have serious consequences. During myocardial infarction, extrasystolic arrhythmia is recorded in 100% of cases.
- Paroxysmal supraventricular (supraventricular) tachycardia, which develops suddenly and also suddenly stops, is characterized by a regular, strict rhythm, although the contraction frequency can reach 250 beats/min. Such tachycardias include: atrial tachycardia, AV nodal tachycardia and tachycardia with WPW syndrome.
- Arrhythmias associated with conduction disturbances (blockades) are usually well recorded on the ECG, are a companion and symptom of various pathologies and are treated by influencing the underlying disease. Blockades that quite often produce (sinoauricular and atrioventricular) bradycardia (40 beats per minute and below) are considered life-threatening and require the installation of a pacemaker that compensates for cardiac activity.
- Atrial fibrillation, in terms of frequency of occurrence, follows immediately after extrasystole and holds 2nd place in prevalence. It is characterized by the formation of excitation and contraction only in certain areas (fibers) of the atrium, when these processes are absent as a whole. Such chaotic and disorderly excitation of individual fibers prevents the passage of impulses into the atrioventricular node, as well as into the ventricles, to which single impulses nevertheless reach, causing excitation there that responds with random contractions.
Based on heart rate, there are 3 forms of atrial fibrillation:
- Heart rate less than 60 beats/min – bradysystolic;
- 60-100 beats/min – normosystolic;
- Heart rate exceeds 100 beats/min – tachysystolic.
On an ECG with AF, the P wave is not recorded because there is no excitation of the atria, and only atrial f waves are detected (frequency 350-700 per minute), which are characterized by irregularity, differences in shape and amplitude, which gives the electrocardiogram a unique appearance.
The cause of MA may be:
- Organic damage to the heart muscle;
- Age-related changes (coronary heart disease, often in combination with arterial hypertension);
- In young people: rheumatism, valve defects (mitral valve stenosis, aortic valve disease);
- Thyroid dysfunction;
- Congenital pathology (heart defects);
- Acute and chronic heart failure;
- Myocardial infarction;
- Acute cor pulmonale;
- Myocarditis, pericarditis;
- Cardiomyopathy.
The incidence of atrial flutter (AF) is 20-30 times lower than AF. It is also characterized by contractions of individual fibers, but a lower frequency of atrial waves (280-300 per minute). On the ECG, atrial waves have a greater amplitude than in AF.
It is interesting that on one ECG you can see the transition of flicker to flutter and vice versa.
The causes of atrial flutter are similar to the causes of fibrillation.
Symptoms of flickering and fluttering are often absent altogether, but sometimes there are some clinical manifestations caused by erratic activity of the heart or symptoms of the underlying disease. In general, such a pathology does not give a clear clinical picture.
Forecast
It is impossible to say with certainty how the condition of a person suffering due to circadian index disorders will change. The complexity of treatment and the time required for recovery depend on the diagnosis. The stage of the disease also influences the duration of therapy. If it is detected at an early stage of development and does not have time to cause significant complications, a complete cure is possible.
Sometimes QI disorders occur due to chronic pathologies. Their symptoms can be relieved, significantly improving the patient’s quality of life. However, systematic taking of prescribed medications may be required. In some cases, sudden cardiac arrest is possible. A sign of irreversible disorders is the circadian index below 110%. In this case, the drugs prolong life, but do not guarantee a complete cure or stabilization of the patient’s condition. Only the attending physician can give the exact timing, based on the test data. There are factors that worsen the outcome with decreased or increased CI:
- presence of hereditary diseases;
- concomitant pathologies, in particular endocrine and neurological;
- age over 50 years;
- the need for surgery if the person is weakened and may not tolerate surgery;
- lack of results from taking prescribed medications.
Prospects for further research
With its growing reputation as an effective marker of recovery status and a likely marker of illness and injury, future research should be directed toward elucidating the true potential of HRV. This means that future research should explore:
- relationship between HRV and diseases
- relationship between HRV and trauma
- strength and power training based on HRV
- acute and chronic effects of HRV monitoring on performance
- reliability of HRV for children
- How accurately does HRV reflect recovery status in various athletic populations (endurance, strength/power, group sports athletes) and various other populations (men, women, geriatric and pediatric).
Key points
- HRV reflects the variability of the time between heart beats.
- Low HRV levels are associated with many types of diseases.
- HRV correlates with recovery state.
- HRV at rest did not demonstrate the ability to reliably reflect overexertion.
- Athletes with high HRV perform better in endurance tests.
- In athletes with high levels of stress, strength increases to a lesser extent.
- With HRV-based training, performance gains were higher than with a pre-planned program.
- HRV is useful for predicting diseases (for example, upper respiratory tract and pulmonary infections).
- It is possible that HRV predicts injury risk, but this property has not been confirmed in human studies.
- HRV increases by improving the time-pressure relationship in the heart.
- Technologies such as Polar, the ithleteTM app and the Omega Wave System can reliably read HRV.
- HRV can be assessed by ultrashort recording (one minute) and in standing, sitting and supine positions.
Original:
https://www.scienceforsport.com/