ESR or erythrocyte sedimentation rate indicates an imbalance of blood proteins, which can result from cell destruction as a result of many pathological conditions. In case of cancer, a change in ESR is not at all necessary, but in some clinical situations, an acceleration or deceleration of the rate of fall of red blood cells may occur.
- ESR: what is it?
- ESR norm
- ESR indicators in oncology
- Table of ESR indicators for oncology in men and women
- ESR analysis
- Preparation for analysis
- How to get tested
ESR: what is it?
ESR and ROE - erythrocyte sedimentation reaction are the same, but the latter abbreviation is considered outdated. ESR shows the intensity of red blood cell aggregation followed by their sedimentation to the bottom.
The clumping of red blood cells is enhanced in the presence of the protein fibrinogen, which is involved in the formation of blood clots and is normally practically absent in plasma. A decrease in the largest fraction of proteins - albumin and an increase in numerous protein fractions of globulins - gamma, beta and alpha changes the ESR towards an increase.
The sedimentation rate will certainly change if the erythrocyte has an abnormal shape and non-standard size, which is typical for anemia of various etiologies, including those caused by complications of chemotherapy.
Any pathological process - infection, inflammation, tumor, especially a malignant blood disease, affects the ratio of blood proteins and, of course, can shift the indicator in one direction or another.
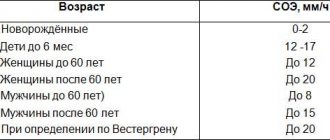
ESR norm
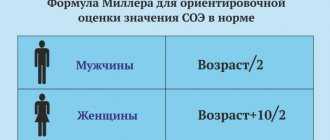
Normal interval rates of subsidence rates have been determined for all age groups of children; for adults there is only a gender norm without taking into account age, but it is known that over the years of life the rate slightly accelerates. In women, normal values are higher than in men: from 2 to 15 mm per hour versus an interval of 1 to 10 mm.
The higher value of female ESR is explained by the lower density of red blood cells per milliliter of blood, which allows them to fall faster, similar to the higher speed of a car on an open highway and the inevitable decline in heavy traffic.
During pregnancy, or rather from the second half, ESR increases, reaching 50-60 mm per hour. After childbirth, the balance of protein fractions and sex hormones, which are proteins, as well as plasma volume gradually return to normal and the rate of fall of blood cells stabilizes.
The erythrocyte sedimentation rate responds to food intake, so blood tests are taken on an empty stomach. The rate of red blood cell sediment formation is sensitive to some medications and physical activity, even to the duration of the summer heat period, so normal values are given with a spread, where the maximum value is several times higher than the minimum value.
Every twentieth healthy adult has his own ESR standard, deviating from the generally accepted standard.
If any abnormalities from the norm appear in the blood test of a cancer patient, and not just changes in ESR, you need to consult with an oncologist; an examination may be required. Our Clinic specialists are ready to help and find the root cause.
Book a consultation 24 hours a day
+7+7+78
An increase in erythrocyte sedimentation rate (ESR) in women under 50 years of age is observed when the value is more than 15 mm/h, in women over 50 years of age - more than 30 mm/h; in men under 50 years old - more than 10 mm/h, over 50 years old - more than 20 mm/h.
Mechanism of occurrence
ESR depends on the intensity of the formation of erythrocyte agents, which is associated with the properties of the plasma and the charge of the erythrocyte membrane. The most important property of blood plasma that affects this indicator is its viscosity. It increases as the protein spectrum shifts towards coarsely dispersed proteins. This occurs primarily with an increase in the amount of fibrinogen, the main stabilizer of red blood cell suspension. An increase in other globulins in the plasma (γ-globulins, α2-globulins) also leads to a drop in the electrical charge of erythrocytes and promotes their aggregation. ESR also depends on the number, size, volume of red blood cells, and the concentration of hemoglobin in them. The fewer these cells, the faster they settle in the capillary.
On average, men have more red blood cells than women, so the ESR is higher in the latter. It also increases at low temperatures. As for physiological conditions, pregnancy is accompanied by a significant acceleration of ESR (up to 30–40 mm/h). In 1984, L. Wilson and co-authors found that in healthy elderly people this figure can reach 50–60 mm/h.
When the level of bile acids in the blood increases, the ESR slows down. Severe hypofibrinogenemia, for example in severe liver damage, can prevent an increase in ESR even with significant dysproteinemia. Its slowdown is facilitated by an increase in the partial tension of CO2 in the blood, as well as erythrocytosis.
When is accelerated ESR observed?
1. Inflammatory diseases:
- bacterial infections,
- immune inflammation,
- aseptic inflammation,
- viral infections.
2. Blood diseases:
- anemia,
- paraproteinemic hemoblastoses,
- other forms of hemoblastosis.
3. Malignant tumors.
4. Metabolic diseases:
- amyloidosis,
- diseases occurring with impaired fat metabolism.
Inflammatory diseases
An increase in ESR is associated with the development of dysproteinemia, the appearance in the bloodstream of tissue breakdown products, C-reactive protein, immune complexes and other components that change blood viscosity and the potential of the erythrocyte membrane. In bacterial infections, the severity of this process is often determined by the severity of the pathology.
With purulent inflammations and abscesses of various organs, the ESR is significantly accelerated. Sometimes its indications lag behind the clinical development of the disease, which is especially evident in acute inflammatory conditions. At the same time, there is no direct connection between the indicators of ESR, body temperature and leukocytosis. ESR increases relatively more slowly and also decreases to normal compared to the number of leukocytes and the clinical manifestations of the disease.
For example, in acute tonsillitis, the maximum acceleration of ESR is most often observed during the period of decreased body temperature and the reverse development of the inflammatory process in the tonsils. Nevertheless, the majority of such common inflammatory diseases as acute appendicitis, cholecystitis, pyelonephritis, pneumonia are characterized by a degree of ESR acceleration that correlates with the severity of the pathological process, although it occurs later than leukocytosis and fever appear.
In chronic inflammatory conditions, an increase in ESR is more often and more consistently recorded than fever and leukocytosis.
Sometimes chronic indolent infections of the biliary tract, urinary system, oral cavity and other localizations occur latently, and acceleration of ESR is one of the few or even the only symptom that allows one to suspect the presence of a chronic focus of infection. Encapsulation of an inflammatory focus, in which decay products do not enter the blood, is not always accompanied by an increase in ESR, in contrast to the rapid entry of necrosis products into the bloodstream. For active tuberculosis, an acceleration of ESR is typical, usually combined with moderate leukocytosis and lymphopenia.
Most specific bacterial infections are associated with an acceleration of ESR. Difficulties in diagnosis arise with latent infections that are not accompanied by a clear clinical picture. It is necessary to identify a latent infection that affects the teeth, tonsils, paranasal sinuses, bile ducts, kidneys, and female genital organs. In addition to a persistent acceleration of ESR, moderate leukocytosis can be detected, sometimes with a shift in the leukocyte formula to the left. C-reactive protein appears in the blood serum, the amount of sialic acids increases, dysproteinemia is possible, mainly due to a moderate increase in globulins of various fractions. Sometimes functional disorders are detected on the part of the organs involved in the inflammatory process. Immune inflammation covers a large group of various diseases with primary or secondary immunopathological reactions. In some cases, exposure to an infectious agent that initially causes infectious inflammation subsequently triggers a chain of immunological phenomena.
A common cause of increased ESR is rheumatism. The level of this indicator correlates with the activity of the rheumatic process and the severity of the exudative phase of inflammation. A significant acceleration of ESR is typical for all systemic connective tissue diseases and is often consistent with the activity of the disease. With these diseases, cryoglobulins sometimes appear in the blood, which sharply increase blood viscosity and reduce ESR. Immune kidney diseases also lead to an increase in it. This is typical for nephrotic syndrome of various origins due to pronounced dysproteinemia and hypercholesterolemia, often hyperfibrinogenemia.
Significant acceleration of ESR has been described in sarcoidosis. Aseptic inflammation also leads to this. It occurs under the influence of various exogenous physical and chemical factors (irradiation, burns, injuries, exposure to acids and alkalis, etc.). In such cases, infection can quickly set in.
A typical example of aseptic inflammation is the so-called resorption-necrotic syndrome during acute myocardial infarction, in which, in particular, ESR increases 1–2 days after the onset of leukocytosis and fever. Moreover, the acceleration remains until the heart attack is completely healed.
The dynamics of ESR, as well as leukocytosis and fever, have a certain diagnostic and prognostic significance. Sometimes this suggests the addition of various complications.
Viral infections, unlike bacterial ones, are rarely accompanied by a significant increase in ESR. In acute viral infections of the respiratory tract, primarily with influenza, a moderate acceleration of ESR is delayed and is often recorded for the first time against the background of already decreasing body temperature and the reverse development of clinical manifestations of the disease. Viral pneumonia often occurs without acceleration of ESR.
Viral hepatitis is characterized by a moderate acceleration of ESR in the pre-icteric period, a decrease in ESR to normal and even lower as jaundice appears, and an increase again with the disappearance of jaundice with a gradual return to normal during recovery. Long-term persistence of a moderately accelerated ESR indicates the persistence of the virus or the addition of a bacterial infection of the biliary tract.
Infectious mononucleosis is accompanied by normal or slightly accelerated ESR in combination with leukocytosis and the presence of polymorphic cells with a large nucleus in the blood.
The bulk of acute viral infections occur with normal or even reduced ESR in combination with moderate leukopenia and relative or absolute lymphocytosis.
Blood diseases
An increase in ESR in anemia is a typical symptom associated primarily with a decrease in the number of red blood cells, although dysproteinemia that is often present also plays a role. There are calculations and nomograms that determine the proper ESR values depending on the number of red blood cells.
It is believed that if the ESR is increased compared to the calculated value, then this may be associated with other severe pathologies that cause anemia (infectious disease, tumor, collagenosis, kidney pathology, etc.). On the contrary, if the ESR is accelerated to a lesser extent, then some authors attribute this to favorable signs of the regenerative nature of anemia (for example, this situation is sometimes observed during reticulocyte crisis in patients with B12-deficiency anemia).
With microspherocytic anemia, there may not be a significant increase in ESR, since the morphological characteristics of erythrocytes in this condition prevent their agglomeration. To diagnose the type of anemia, it is necessary to take into account the medical history, clinical picture, changes in blood tests, bone marrow, and instrumental data (ultrasound, endoscopic examination of the gastrointestinal tract).
Acceleration of ESR is observed in 85% of patients with multiple myeloma due to hyperviscosity syndrome. This diagnosis is made when more than 10% of plasma cells are found in the bone marrow and the paraprotein is present in the serum and/or urine. In Bence-Jones myeloma, when only light chains are secreted, the ESR may remain within normal limits unless severe anemia is present. The second most common, but very rare paraproteinemic hemoblastosis is Waldenström's macroglobulinemia, for which, unlike multiple myeloma, osteolytic processes are uncharacteristic. But hepatosplenomegaly, lymphadenopathy and pronounced hyperviscosity syndrome are typical. The latter appears:
- bleeding of mucous membranes,
- hemorrhagic retinopathy,
- dilatation of retinal veins,
- Raynaud's syndrome,
- ulceration and gangrene of the distal limbs,
- paraproteinemic coma,
- macroglobulinemic retinopathy.
The criteria for the diagnosis of Waldenström's macroglobulinemia are the presence of a mixed cellular substrate in the bone marrow (plasma cells and lymphocytes), detection of monoclonal macroglobulinemia, fibrosis in the trephine.
Heavy chain diseases (HCDs) are B-cell lymphatic tumors. There are options: BTC-γ, BTC-α, BTC-δ, BTC-μ.
With BTC-γ, the average age of patients is 60 years, but can also occur in children. The clinical picture includes: fever, night sweats, weakness, weight loss, lymphadenopathy, splenomegaly, hepatomegaly, damage to the pharyngeal lymphoid ring, recurrent infections, damage to the thyroid gland, salivary glands, skin, subcutaneous tissue, autoimmune processes (25%) with the clinic rheumatoid arthritis, systemic lupus erythematosus, autoimmune hemolytic anemia, thrombocytopenia, thyroiditis, Sjogren's syndrome and others. The bone marrow is affected in 50% of cases. This nosological form does not have a specific histological picture. In the immunochemical diagnosis of BTC-γ, the secretion of fragments of heavy chains of the PIgG subclasses is determined, serum PIg is present in the urine (overload proteinuria), Bence Jones protein is usually absent.
BTC-α is more common in children and young patients under 30 years of age. There are 2 options: abdominal and pulmonary. In the first case, malabsorption syndrome (chronic diarrhea, steatorrhea, exhaustion, edema, hypocalcemia, hypokalemia, baldness, amenorrhea), fever, and attacks of abdominal pain are noted. The pulmonary form is accompanied by bronchopulmonary lesions and mediastinal lymphadenopathy. In the immunochemical diagnosis of BTC-α, fragments of α-chains are determined in blood serum and urine, in the contents of the duodenum and small intestine, and in saliva. Bence Jones protein is never detected in BTC-α. Benign monoclonal gammopathies have been described, which manifest themselves only as a syndrome of increased ESR and are determined biochemically. Sometimes it is possible for such gammopathy to exist throughout the patient’s life. But in some cases, the clinical picture of myeloma or another malignant process gradually develops, sometimes after decades.
As for other forms of hematological malignancies, an increase in ESR is typical for all acute and chronic leukemias, malignant lymphomas, including Hodgkin lymphoma. For diagnosis, in addition to examining the hemogram, sternal puncture and/or trepanobiopsy are necessary. To determine the various forms of lymphomas, it is necessary to conduct histological, enzyme-linked immunosorbent examination of biopsy material, and genetic studies. To clarify the localization of damage to the lymph nodes and internal organs, ultrasound of the abdominal cavity and CT scan of the chest are used.
Malignant tumors
The increase in ESR in this case is associated not only and not so much with the severity of anemia, but with dysproteinemia, an increase in the amount of fibrinogen and a change in the charge of the erythrocyte membrane. More often, persistent and significantly accelerated ESR is observed in cancer of the bronchus, bones, ovary, hypernephroma, sarcomas, and less often in gastrointestinal tumors. Although with cancer of the stomach, colon, pancreas, and liver, a significant increase in ESR is also sometimes encountered. Its magnitude depends on the histological structure of the tumor, but is largely determined by the size of the tumor and the presence of complications. In some cases, an increase in ESR is at the first stage the only manifestation of malignant growth, ahead of clinical symptoms.
With the development of the tumor, other peripheral blood parameters may also change: anemia is often observed (less commonly secondary erythrocytosis), in some cases neutrophilic leukocytosis, lymphopenia, monocytosis, and hyperthrombocytosis are observed. If a neoplasm is suspected and there are no clear clinical manifestations, a thorough and systematic examination is necessary: sternal puncture (detection of signs of hemoblastosis or anemia as the cause of an increase in ESR), ultrasound of the abdominal organs, CT and X-ray examination of the lungs, bronchoscopy, FGDS, FCS. You should consult an obstetrician-gynecologist and urologist.
Metabolic disorders
Most often, an increase in ESR is observed with tissue dysproteinoses. This process may be associated with some forms of hyperlipidemia and widespread atherosclerosis. The main reasons for an increase in ESR in metabolic diseases are dysproteinemia and hypercholesterolemia.
Amyloidosis leads to its acceleration due to severe dysproteinemia. The most common is secondary amyloidosis, which complicates the course of chronic suppurative lung diseases, tuberculosis, chronic osteomyelitis, ulcerative colitis, Crohn's disease, and systemic connective tissue diseases. Paraproteinemic hemoblastoses can lead to the occurrence of this lesion. Amyloid deposition is possible in all organs and tissues. Most often, parenchymal organs are affected: kidneys, liver, spleen, adrenal glands, less often - the gastrointestinal tract, cardiovascular system, lungs, thyroid gland, etc.
There are 4 stages of renal amyloidosis: latent, proteinuric, nephrotic and azotemic. In the first case, the symptoms of the underlying disease, potentially dangerous in relation to amyloidosis, dominate. Sometimes a slight proteinuria appears and a persistent, significantly increased ESR is recorded, which is often not explained by the activity of the underlying pathology. Already at this stage, an enlarged liver and spleen can be palpated, amyloid deposition in which is most common in secondary amyloidosis.
The advanced stage is manifested by complete nephrotic syndrome (proteinuria more than 3 g per day, hypoproteinemia, hyperlipidemia, edema). Symptoms of chronic renal failure subsequently arise and progress. In some patients, amyloid is deposited primarily in the liver. This is characterized by moderate pain in the right hypochondrium, flatulence, and sometimes jaundice. The liver can be enlarged very significantly and descend into the pelvis. In rare cases, a predominant deposition of amyloid in the adrenal glands is possible with a gradual development of the clinical picture of hypocortisolism up to the full-blown symptoms of chronic adrenal insufficiency: increasing weakness, adynamia, persistent decrease in blood pressure, nausea, vomiting, diarrhea, hyperpigmentation of the mucous membranes of the lips and skin on exposed parts of the body and in the area of folds, loss of sexual function. Any impact (intercurrent infection, trauma, etc.) can trigger an adrenal crisis. At the same time, all the listed symptoms increase. Abdominal pain, uncontrollable vomiting appear, dehydration rapidly progresses, convulsive syndrome, oliguria and acute renal failure occur. As a result, a coma develops and the patient dies. Even more rarely, predominant amyloid deposition is observed in the intestine. Clinically, this is manifested by pain, intestinal atony, and persistent diarrhea. Sometimes bleeding is possible.
A persistent and significant increase in ESR as an early symptom is characteristic of primary (idiopathic) amyloidosis.
The most typical lesions are the skin (itching, petechiae, pigment spots, urticaria, sometimes dense swelling that makes the face amicable), muscle and nervous systems (muscle pain, stiffness, muscle tightening, sometimes their atrophy, paresthesia, less often - polyneuropathic syndrome, epileptiform seizures , psychotic reactions). In contrast to secondary amyloidosis, damage to parenchymal organs is less common in primary amyloidosis. Selective deposition of amyloid in any organ is possible. Various forms of hereditary amyloidosis, caused by genetics, have also been described.
A persistent increase in ESR is typical for senile amyloidosis , which is manifested by a triad of Schwartz symptoms: damage to the heart (progressing heart failure), brain (various types of dementia) and amyloid deposition in the islets of Langerhans of the pancreas with the development of symptoms of diabetes. All forms of amyloidosis are characterized by hypercholesterolemia and hyper-β-lipoproteinemia, which occur in the nephrotic stage of renal amyloidosis. When the latter are affected, occasional small proteinuria is observed at an early stage, then it increases and usually exceeds 3 g per day. Proof of amyloidosis is possible by biopsy of various organs and tissues, followed by histological and histochemical examination of the biopsy.
Diseases that occur with impaired fat metabolism, in particular, widespread atherosclerosis, with hypercholesterolemia, can cause a persistent, often moderate, sometimes significant increase in ESR.
In patients with severe atherosclerosis, weight loss, accelerated ESR, sometimes predominant signs of atherosclerotic damage to the cerebral vessels are found (headache, noise in the head or ears, dizziness, syncope, sleep disorders, memory disorders, changes in the emotional sphere, mental disorders; cerebral disorders may occasionally occur vascular crises), and symptoms of damage to the coronary arteries, aorta, and arteries of the lower extremities can be moderately expressed.
Hypercholesterolemia accompanies a variety of diseases, especially common in some forms of liver cirrhosis and nephrotic syndrome of any nature. The increase in ESR in these cases is associated not only with it, but also with severe dysproteinemia. Hypercholesterolemia is typical of hypothyroidism, in which the ESR may increase. It is also typical for some hereditary forms of hyperlipidemia, which contribute to the development of atherosclerosis, for some lipidosis and glycogenosis, often accompanied by a moderate increase in ESR.
A significant acceleration of ESR occurs with generalized xanthomatosis, in particular with Buerger-Grütz syndrome, or hypercholesterolemic xanthomatosis (a disease of middle-aged people; typical are tuberous xanthomas on the face, limbs and mucous membranes, hepatosplenomegaly, chronic pancreatitis, central nervous system damage) and Harbitz-Müller syndrome, or familial hypercholesterolemia (external xanthomas, xanthomatous changes in blood vessels, which can lead to changes in various organs). This process is also described in Urbach-Wiethe syndrome, or mucocutaneous lipoid proteinosis (hyalinosis of the skin and mucous membranes). Typical are nodular deposits in the skin, oral cavity, and vocal cords (which leads to persistent hoarseness), and dysphagia. Possible damage to the central nervous system with epileptiform seizures and mental infantilism. Disorders of fat and carbohydrate metabolism are detected.
conclusions
To summarize, we can say that in order to get an idea of the possible scope of the “diagnostic search” with an increased ESR as a leading sign, it is necessary to obtain detailed anamnestic information. Examination of a patient with an incomprehensible acceleration of ESR requires attention to the main “hot” spots: the size and consistency of the lymph nodes, careful palpation of the spleen, kidneys, listening to the heart, lungs, etc. The doctor must have laboratory and instrumental data.
ESR indicators in oncology
Erythrocyte sedimentation rate is a nonspecific marker, since it changes with any pathology. ESR is only evidence of trouble and the release of “extra” proteins into the blood during tissue breakdown, insufficient synthesis of albumin due to impaired liver or hemoglobin function, as well as changes in the structure of the blood cell itself during anemia.
For a long time, in the majority of those suffering from a malignant neoplasm, including those at the metastatic stage, the blood picture can be absolutely normal. The exception is blood diseases accompanied by the synthesis of pathological proteins - paraproteins, which occurs in myeloma and some malignant lymphomas.
ESR may increase in the following clinical situations:
- disintegration of a cancer tumor, when its central part is deprived of nutrition, forming an area of necrosis, and the destroyed cells enter the bloodstream;
- the addition of inflammation along the periphery of the cancer node, which often accompanies metastases in the lung or primary lung cancer;
- disturbances in protein synthesis in the liver affected by metastases;
- loss of proteins with frequent removal of ascitic or pleural fluid;
- malabsorption disorders due to a malignant tumor of the gastrointestinal tract or removal of a large volume of the stomach and intestines;
- disturbances in the synthesis of the hormone erythropoietin by the kidneys due to the toxic effects of chemotherapy drugs;
- myocardial damage due to certain cytostatics;
- development of anorexia-cachexia syndrome in the terminal stage of the disease.
A decrease in ESR in a cancer patient is possible:
- when red blood cells are deformed as a result of the use of platinum derivatives;
- with jaundice - a complication of pancreatic cancer;
- dehydration as a result of severe vomiting, especially during hot periods;
- progression of failure due to tumor damage to the liver;
- severe pulmonary heart failure with cancerous pleurisy or advanced lung cancer.
A change in ESR in a cancer patient is not a mandatory characteristic of cancer and does not reflect the course of the malignant process, but always indicates clinical distress. In each case of a change in the analysis, it is necessary to seriously understand; it is not at all necessary that this change is a sign of cancer progression.
C-reactive protein (CRP) test
What it is.
A venous blood test in which the concentration of C-reactive protein in a sample is determined. This test is a more accurate indicator of inflammation than ESR because C-reactive protein appears in the blood only during inflammation.
How it works.
The liver produces C-reactive protein in response to the call of immune cells that have encountered a problem, from a bacterial or viral infection to cancer cells. When it encounters dead or dying cells, the protein binds to them and triggers another defense mechanism - it activates the complement system. This means that normally there is either no CRP in the blood, or very little. And if it appears, it means there is definitely inflammation going on somewhere.
Why is it prescribed?
Although CRP is a more reliable marker of inflammation than ESR, the mere fact of its presence in the blood does not indicate anything about the causes of inflammation, so it is not suitable for diagnosis. As a rule, the analysis is prescribed to clarify the diagnosis or to monitor treatment: for example, if a patient with COVID-19 has a CRP level of more than 10 mg/l, then this, along with other signs, may indicate a moderate course of the disease.
“CRP is a more accurate indicator than ESR,”
says another specialist at a Moscow clinic
- it reflects the severity of bacterial inflammation.
If a patient has high white blood cells and high CRP, this strongly suggests that they have a bacterial infection that needs to be treated with antibiotics.” In pneumonia, CRP will reflect the extent of lung damage. The norm is from 0 to 6. If a person has a common cold, it will be in the range of 10-12. But if CRP, for example, is in the range of 100-300, we are most likely talking about serious pneumonia.
“If a person has pneumonia confirmed on an X-ray or CT scan, CRP will fall as they recover,”
explains another doctor.
“At the same time, there are clinical conditions when a person who has recently suffered coronavirus disease maintains a residual temperature within the range of 37.1-37.2°C. If the CRP is normal, this indicates that the patient has actually recovered. And if CRP is high, the person needs further treatment.”
Table of ESR indicators for oncology in men and women
On the Internet you can find tables of changes in ESR for various types of malignant processes separately for women and men. This information could be trusted if the ESR indicator were included in the mandatory criteria for cancer, as we know, most tumor markers produced by cancer cells do not have this honor.
The erythrocyte sedimentation rate in most cancer patients does not deviate from the norm over the period of cancer development. On the eve of death from the progression of a malignant disease, when the volume of the tumor and its aggression are practically incompatible with life, and the function of the most important body systems is reduced to a minimum, the ESR can demonstrate “full health.” A banal respiratory infection, which occurs in the average Russian six times a year, in a radically treated patient without any signs of a malignant process can increase the rate of red blood cell precipitation to 40-60 mm per hour for a month.
With a very small range of oncohematological diseases, ESR may coincide with the progression of the process, but this is not necessary, nor is a decrease in the indicator considered a victory over the tumor.
The interpretation of test changes is individual, and tables of ESR correspondence to certain cancer diseases can be considered a marketing ploy of the site that does not reflect the objective oncological reality.
Two methods of performing a laboratory blood test for ESR
In Russia, two approaches to conducting this analysis are widespread. They differ in the degree of accuracy, the type of biological material being analyzed and the procedure for collecting it.
1.According to Panchenkov
To perform this test, capillary blood is usually taken from a finger. It is mixed with a special anticoagulant that prevents clotting in a ratio of 1 to 4. Then it is placed in a Panchenkov stand - a glass tube with a stand and a scale with 100 divisions. After an hour, when the blood is divided into plasma and heavier formed elements (erythrocytes, platelets and leukocytes), a measurement is taken.
This method is extremely common in the post-Soviet space.
2.According to Westergren
According to the method, blood is first taken from a vein. Then the analyzed material is mixed with an anticoagulant and placed in a special tube 300 mm high. Moreover, it is filled to ⅔. measurements are taken within an hour. It turns out that the result is assessed on a scale with 200 divisions - its accuracy is higher.
Westergren analysis complies with international standards.
Note! In 5% of the total population of the world, ESR indicators from birth differ from the standard. And this is not accompanied by any pathologies.
How to get tested
You need to take the test calmly, it’s too late to get nervous - everything has already happened in the body and all that’s left is to get the information. It would be more correct to pose the question differently: where to take it. It is advisable for an oncology patient to undergo tests in a specialized institution, where not only analysis on the machine is available, but also monitoring of the results obtained “in manual mode”. With specific treatment, especially after the use of medications, the conventional boundary of normality of indicators may temporarily shift. Often, haste in interpreting the result results in excessive examination and unnecessary treatment.
If you want an optimal and unconditionally professional approach, accuracy and objectivity, come for a consultation at our clinic.
Book a consultation 24 hours a day
+7+7+78
Bibliography
- Lugovskaya S.A., Morozova V.T., Pochtar M.E., Dolgov V.V. /Laboratory hematology// M.: Publishing house. Unimed-press; 2002.
- Pervushin Yu.V., Lugovskaya S.A., Marchenko L.A., Kovalevich N.I. / Hematological studies in clinical laboratory diagnostics//Stavropol; 2006
- Nazarenko G.I., Kishkun A.A. / Clinical assessment of laboratory research results // M., 2000.
- Oganesyan A.A., Garbatsevich M.S., Kostyukovich D.I. and others /ESR: old test, new opportunities // Lab. diagnostics. Eastern Europe; 2012; No. 4.
- Chizhevsky A. L. /Biophysical mechanisms of erythrocyte sedimentation reaction// Novosibirsk: Science, 1986.
What does a low erythrocyte sedimentation rate indicate?
This indicator may be below normal due to:
- Following a strict vegetarian diet;
- Violations of water-salt balance;
- Diseases of the nervous system;
- Fasting;
- Excessive physical activity;
- Taking certain steroid hormones;
- Congenital disorder of the hemoglobin protein structure;
- Pregnancy in the second and third trimesters.
Decreased values are much less common than increased values. Often they do not mean any serious violations. Yet sometimes it is a low erythrocyte sedimentation rate that helps the doctor identify the problem. Or at least understand in which direction to look for it, what studies to prescribe for the patient.
Make an appointment now!
Leave your contact details or call and our manager will contact you to make an instant appointment