To obtain accurate results on the condition and functioning of the heart in electrocardiography, the use of additional leads is often practiced. As a rule, this additional measure allows for timely diagnosis of the development of myocardial infarction and other pathologies. Symptoms of this problem are not always noticed during routine diagnostics using standard parameters, which is explained by the varying strength of the manifestation of changes. The most popular is the Sky ECG, less used are the orthogonal lead and Arrighi.
A person who specializes in this area knows exactly how the axes of the leads along the Sky are connected and the probable possibilities of diagnosing them. This knowledge helps not to repeat standard techniques.
Basic rules for electrode placement
To record an ECG, you need to install electrodes on special points on the body. This is the only way to correctly record the electrical impulses produced by the heart. It is the correct location of the terminal that ensures a clear recording of the cardiogram. Be sure to lubricate the ECG electrode with alcohol.
If the patient has a lot of body hair, then you need to treat the skin with a soap solution or shave the hair. For better electrical conductivity, you need to lubricate each electrode with gel. If you don’t have the gel at hand, you can take an isotonic solution or gauze pads. But if the study is long, then gauze pads cannot be used.
If stationary ECG devices are used, they must be grounded.
Electrodes are either single-use or reusable. The choice of electrodes depends on the preferences of the healthcare professional performing the ECG.
ecg how to do it correctly
How is the procedure performed?
Understanding the technique and knowing how to perform it helps you not to worry in the doctor's office and go through the procedure with minimal stress.
The procedure is absolutely painless and does not impose any restrictions on the patient in preparation or the period after the study—the essence of the method is the special placement of the electrodes. ECG across the Sky - location of electrodes and procedure:
- placing the patient on the couch;
- applying a paste of water and soap to the places where the electrodes are attached (an oilcloth is first placed under the patient’s body);
- connecting an active yellow electrode, which is held on a plate in the lower corner of the left scapula or in position V7 (the latter gives more accurate results and facilitates the examination of patients confined to bed);
- connecting a passive red electrode using a suction cup - intercostal space on the right;
- connecting the red electrode using a bulb suction cup (apex of the heart);
- switching a toggle switch for sequential connection of all axes (points between electrodes) in order to identify pathologies.
The axes that are formed when switching the toggle switch on the equipment reflect different indicators and help to evaluate the condition of the heart and myocardium, which are not noticeable during the classical procedure.
There are three positions in total - they are labeled A, D, I. The most informative of them is position D - it includes the axis between the red and yellow electrodes and most accurately demonstrates the condition of the posterior side of the heart and the presence of pathological abnormalities in the posterior wall of the left ventricle. The remaining two axes show changes in the anterolateral wall. Taken together, a study along all three axes helps to find foci of ischemia, signs of myocardial infarction and other changes.
Taking an ECG across the Sky with stress (several squats) or medication (drugs that stimulate reversible spasm of the coronary vessels) tests helps complete the picture. These methods make it possible to detect foci of hidden ischemia (these are areas that are not fully supplied with blood).
How to install electrodes on limbs?
For better memorization, you can use the traffic light rule. Place red on the right hand, yellow on the left hand, green on the left leg and black on the right leg. It is the last electrode that is grounding.
All placement is performed on the proximal part of the limbs. But, be sure to lubricate the place where the terminals are applied with gel. If there is no gel, you can take an isotonic solution or a gauze pad. If one of the limbs is missing, you need to install clamps on the stump. For better contact, you need to secure the terminals with rubber bands.
correct application of electrodes
Decoding the results
The interpretation is performed by a functional diagnostics doctor. The subject of his consideration is a tape with a cardiogram on which the teeth are depicted. The specialist evaluates the intervals, height and makes a diagnosis about the condition of the heart muscle.
As indicated, lead D is the most informative of the three considered. The presence of ischemic changes is indicated by three main indicators on the cardiogram:
- increased voltage in the QRS complex;
- non-compliance with the norm of the ratio of the amplitudes of the Q and R waves;
- expansion of the Q wave (also fixed in the second switching).
It is impossible to independently determine the condition of the heart using a cardiogram. Wait for a consultation with a specialist from the NEARMEDIC clinic or with your attending physician if you are undergoing examination and treatment in another clinic.
The information value of the method becomes higher when used in addition to recording electrocardiography in 12 leads and other techniques (according to Arrighi, in orthogonal leads). In addition to the ECG, data on the condition of the heart are provided by electrocardiography, color circulation and ultrasound with Dopplerography. In difficult cases, several techniques are used.
Contraindications
Carrying out an ECG
may be difficult in the following cases:
- the patient is overweight;
- there are injuries in the sternum area;
- Excessive hair growth in the area being examined.
Electrocardiogram
with a load is not carried out in the presence of the following pathological conditions:
- chronic cardiac dysfunction;
- acute coronary circulatory disorder (ischemia hearts
);
- myocardial infarction during the acute stage;
- viral and other infectious diseases in the acute phase;
- persistent arterial hypertension with deterioration;
- increased risk of aortic dissection or rupture.
Electrocardiography (ECG)
Electrocardiography is a technique for recording and studying the electric fields generated during the work of the heart. Electrocardiography is a relatively inexpensive but valuable method of electrophysiological instrumental diagnostics in cardiology.
The direct result of electrocardiography is the production of an electrocardiogram (ECG) - a graphical representation of the potential difference resulting from the work of the heart and conducted to the surface of the body. The ECG reflects the averaging of all vectors of action potentials that arise at a certain moment in the heart’s activity.
In the Olmedica and Affordable Health clinics you can do an ECG 7 days a week (Read more)
ECG interpretation is done by professionals with many years of experience.
Story
In the 19th century, it became clear that the heart produces a certain amount of electricity during its work. The first electrocardiograms were recorded by Gabriel Lippmann using a mercury electrometer. Lippmann's curves were monophasic, only vaguely resembling modern ECGs.
The experiments were continued by Willem Einthoven, who designed a device (string galvanometer) that made it possible to record a true ECG. He also came up with the modern designation for ECG waves and described some disturbances in the functioning of the heart. In 1924 he was awarded the Nobel Prize in Medicine.
The first domestic book on electrocardiography was published under the authorship of the Russian physiologist A. Samoilov in 1909 (Electrocardiogram. Yenna, Fischer Publishing House).
Application
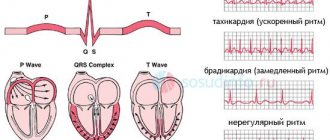
- Determination of the frequency and regularity of heart contractions (for example, extrasystoles (extraordinary contractions), or loss of individual contractions - arrhythmias).
- Indicates acute or chronic myocardial damage (myocardial infarction, myocardial ischemia).
- Can be used to identify metabolic disorders of potassium, calcium, magnesium and other electrolytes.
- Detection of intracardiac conduction disorders (various blockades).
- Screening method for coronary heart disease, including stress tests.
- Gives an idea of the physical condition of the heart (left ventricular hypertrophy).
- May provide information about non-cardiac diseases such as pulmonary embolism.
- In a certain percentage of cases it may be completely uninformative.
- Allows you to remotely diagnose acute cardiac pathology (myocardial infarction, myocardial ischemia) using a cardiophone.
Device
As a rule, the electrocardiogram is recorded on thermal paper. Fully electronic devices allow you to save ECG in a computer. The paper speed is usually 25 mm/s. In some cases, the paper speed is set to 12.5 mm/s, 50 mm/s or 100 mm/s. At the beginning of each recording, a reference millivolt is recorded. Typically its amplitude is 10 mm/mV.
Electrodes
To measure the potential difference, electrodes are placed on different parts of the body.
Filters
The signal filters used in modern electrocardiographs make it possible to obtain a higher quality electrocardiogram, while introducing some distortion into the shape of the received signal. Low-pass filters of 0.5–1 Hz can reduce the effect of a floating contour, while introducing distortion into the shape of the ST segment. A 50–60 Hz notch filter eliminates network noise. A high-pass (35 Hz) anti-tremor filter suppresses artifacts associated with muscle activity.
Normal ECG
Correspondence of ECG sections with the corresponding phase of the heart
Usually, 5 waves can be distinguished on an ECG: P, Q, R, S, T. Sometimes you can see a subtle U wave. The P wave reflects the work of the atria, the QRS complex - ventricular systole, and the ST segment and T wave - the process of myocardial repolarization.
Leads
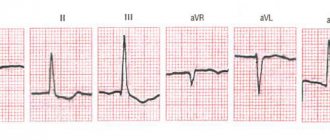
Each of the measured potential differences is called a lead. Leads I, II and III are superimposed on the limbs: I - right hand - left hand, II - right hand - left leg, III - left hand - left leg. No readings are recorded from the electrode on the right leg; it is used only to ground the patient.
Enhanced leads from the limbs are also recorded: aVR, aVL, aVF - unipolar leads, they are measured relative to the average potential of all three electrodes. Note that among the six signals I, II, III, aVR, aVL, aVF, only two are linearly independent, i.e., the signal in each of these leads can be found knowing the signals only in any two leads.
With a unipolar lead, the recording electrode determines the potential difference between a specific point in the electric field (to which it is connected) and a hypothetical electric zero. Unipolar chest leads are designated by the letter V.
Electrode installation diagram
- V1-V6 Leads Location of the recording electrode
- V1 In the 4th intercostal space at the right edge of the sternum
- V2 In the 4th intercostal space at the left edge of the sternum
- V3 Midway between V2 and V4
- V4 In the 5th intercostal space along the midclavicular line
- V5 At the intersection of the horizontal level of the 4th lead and the anterior axillary line
- V6 At the intersection of the horizontal level of the 4th lead and the midaxillary line
- V7 At the intersection of the horizontal level of the 4th lead and the posterior axillary line
- V8 At the intersection of the horizontal level of the 4th lead and the midscapular line
- V9 At the intersection of the horizontal level of the 4th lead and the paravertebral line
Basically, 6 chest leads are recorded: from V1 to V6. Leads V7-V8-V9 are rarely used in clinical practice; they are needed only for more accurate and detailed studies.
To search and register pathological phenomena of “silent” areas of the myocardium, additional leads are used (not included in the standard set):
Additional Wilson leads, the location of the electrodes and, accordingly, the numbering, by analogy with Wilson's chest leads, continue into the left axillary region and the posterior surface of the left half of the chest. Specific to the posterior wall of the left ventricle.
Abdominal leads were proposed in 1954 by J.Lamber. Specific for the anteroseptal part of the left ventricle, the lower and inferolateral walls of the left ventricle. Currently practically not used
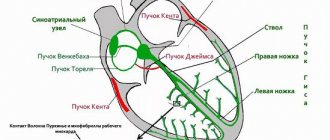
Leads according to Nebo - Gurevich. Proposed in 1938 by the German scientist W. Nebh. The three electrodes form an approximately equilateral triangle, the sides of which correspond to three areas - the posterior wall of the heart, the anterior wall and the adjacent septum.
A correct understanding of the normal and pathological vectors of depolarization and repolarization of myocardial cells allows us to obtain a large amount of important clinical information. The right ventricle has a small mass, leaving only minor changes on the ECG, which leads to difficulties in diagnosing its pathology, compared to the left ventricle.
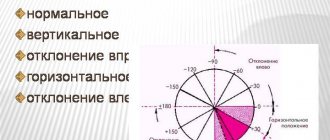
Electrical axis of the heart (EOS)
The electrical axis of the heart is the projection of the resulting vector of excitation of the ventricles in the frontal plane (projection onto axis I of the standard electrocardiographic lead). Usually it is directed down and to the left (normal values: 30°...70°), but it can also go beyond these limits in tall people and people with increased body weight (vertical EOS with an angle of 70°...90°, or horizontal - with an angle of 0 °…30°). Deviation from the norm can mean either the presence of any pathologies (arrhythmias, blockades, thromboembolism) or an atypical location of the heart (extremely rare). The normal electrical axis is called a normogram. Its deviations from the norm to the left or to the right are, respectively, a leftogram or a rightogram.
ECG prices
Research results
The resulting cardiogram
transferred to a cardiologist for functional diagnostics to
decipher
the information. The results are sent to the attending physician, who recommends additional research or selects effective treatment tactics.
ECG parameters are considered normal:
:
- Heart rate (number of contractions within 1 minute) - 60–80 beats/min.
- Type of heart rhythm (where the nerve impulse that causes the contraction occurs) hearts
) - sinus. In case of disturbances, the rhythm can be ventricular, atrial, or atrioventricular.
- The electrical axis of the heart (the direction characterizing the propagation of impulses) is 30–70 degrees. During pregnancy, EOS up to 90 degrees is considered normal.
Application
- Determination of frequency (see also pulse) and regularity of heart contractions (for example, extrasystoles (extraordinary contractions), or loss of individual contractions - arrhythmias).
- Indicates acute or chronic myocardial damage (myocardial infarction, myocardial ischemia).
- Can be used to identify metabolic disorders of potassium, calcium, magnesium and other electrolytes.
- Detection of intracardiac conduction disorders (various blockades).
- Screening method for coronary heart disease, including stress tests.
- Gives an idea of the physical condition of the heart (left ventricular hypertrophy).
- May provide information about non-cardiac diseases such as pulmonary embolism.
- Allows you to remotely diagnose acute cardiac pathology (myocardial ischemia) using a cardiophone.
- Can be used in studies of cognitive processes, alone or in combination with other methods
Preparing for the study
No special preparation is required. If there is thick hair in the chest area, it is recommended to remove hair. The day before, you can stick to your usual drinking and eating regimen. To obtain reliable results, it is not recommended to undergo diagnostics immediately after eating food, coffee, energy drinks, alcohol, or after intense physical activity. ECG accuracy
may be affected by the time of the study, extraneous electromagnetic background, location of the branch electrodes, elevated temperature in the patient, stress and other factors.
How the study is performed
Electrocardiogram
carried out using a stationary or portable electrocardiograph.
The patient is in a supine position. To increase the electrical activity of the skin, the area of the sternum and limbs is wiped with a damp sponge. Branch electrodes are installed in the heart
, on the ankles, and on the wrists. Then the diagnostician turns on the device and begins reading information about electrical potentials.
Graphs of cardiac muscle activity are displayed on the screen in the form of an oscillation graph and recorded on a special tape. The standard duration of ECG recording does not exceed 15 minutes. The results obtained are assessed by general practitioners, cardiologists, and general practitioners. The description (decoding) of the electrocardiogram is performed by cardiologists and functional diagnostics doctors.
Indications
The study is carried out in the following cases:
- the patient has detected abnormalities in work hearts
or there is a high risk of developing pathologies;
- there is shortness of breath;
- constant pain in the sternum or in the heart area;
- presence of changes in arrhythmias;
- in the presence of dizziness, headaches;
- study of the effectiveness of the installed cardiac stimulator;
- the presence of a heart murmur ;
- for chronic diseases of the cardiovascular system, when the patient develops alarming symptoms;
- when planning surgical intervention;
- performance evaluation hearts
during pregnancy;
- undergoing medical examination after 45 years;
- passing medical examinations;
- fainting, sudden weakness;
- for various pathologies of the endocrine system, nervous system, as well as internal organs, in cases of high probability that the heart is affected by these processes;
- in the presence of cardiovascular pathology on the father's or mother's side.
ECG
It is recommended to do this if cholesterol increases and in other cases when blood counts differ from the norm. Patients over 40 years of age should have their heart function monitored annually. Elderly people, pregnant and nursing mothers, as well as young patients can undergo the study.
Questions and answers
What is an orthostatic test with an ECG?
The Doctor Nearby clinic network uses modern methods for diagnosing cardiac activity. The difference between this type of cardiography is that during the study the patient is in an upright position. The oblique test can be passive or active. The test is carried out after a regular cardiogram
, which allows one to assess the autonomic reactivity of the cardiovascular system and monitor rhythm and conduction disturbances.
How is a drug test performed during an ECG?
The Doctor Nearby network of clinics performs electrocardiography using pharmacological drugs. ECG
is recorded against the background of administering medications to the patient that directly affect the functioning of the heart and coronary circulation.
The method is a modification of the usual procedure. During this diagnosis, blood pressure is monitored and the patient's condition is monitored. Blood pressure readings are monitored before the drug is administered, after the drug is administered, and after the drug is stopped. The method of recording an electrocardiogram
is classic.
This diagnostic method is used to detect coronary artery disease and rare heart diseases.