Author Marina Lebedeva
10/17/2002 16:31 (Updated: 07/06/2021 16:46)
Health
The development of the fetus is influenced by a huge number of factors. A low hemoglobin level in an expectant mother is one of them. According to statistics, approximately half of pregnant women face this problem. In the article we will talk about what the hemoglobin standards are during pregnancy and what to do if hemoglobin is low.
Hemoglobin is an indicator that requires special monitoring during pregnancy
Waiting for a child means nine months of not only joy, but also, unfortunately, a double burden on the body. To maintain the normal functioning of all internal systems and provide nutrition to the fetus, a larger number of different elements are required, including hemoglobin - a complex iron-containing protein, an integral participant in the process of oxygen transfer through the circulatory system. This is due, first of all, to an increase in the volume of circulating blood. Until birth, the circulatory system of the unborn baby is connected to the circulatory system of the mother. In a woman’s body, an additional circle of blood circulation is formed.
In the second trimester, the rate of red blood cell formation decreases, and the iron accumulated by the body comes to an end, while the fetus develops more and more intensively. The need for hemoglobin increases up to one and a half times compared to the “non-pregnant” state.
In the third trimester, the body prepares for childbirth and possible blood loss during it, while the already formed fetus requires more and more hemoglobin. As a result, the expenditure of iron-containing protein reaches a maximum, and its content in the body reaches a minimum (from 100 grams per liter).
During nine months of pregnancy, 800–1200 mg of iron is consumed more than in normal conditions. Of this, about 500 mg goes to the needs of the fetus. By the end of the third trimester, the expectant mother needs about 6 mg of iron per day, while the usual requirement is approximately 4.6 mg per day.
Throughout pregnancy, a low hemoglobin content is usually recorded (the norms are given below), which does not always indicate a protein deficiency. However, with a prolonged decrease in the level below 105 grams per liter, a woman may develop iron deficiency state (IDS), and then iron deficiency anemia (IDA).
What affects iron deficiency during pregnancy?
The following factors can aggravate the risk of developing VSD:
- a short interval between pregnancies - the body will not have time to replenish the lack of iron in the blood depot;
- toxicoses . Frequent vomiting reduces the intake of not only iron, but also other elements;
- multiple pregnancy . Iron consumption increases in this case proportionally;
- Dysbacteriosis impairs microelement absorption.
It is very important to monitor the level of hemoglobin in the body throughout pregnancy and promptly take corrective measures if necessary.
Anemia and pregnancy
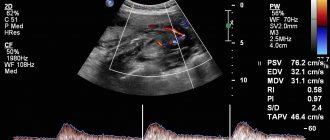
Ultrasound machine HS40
Top seller in high class.
21.5″ high-definition monitor, advanced cardio package (Strain+, Stress Echo), expert capabilities for 3D ultrasound in obstetrics and gynecology practice (STIC, Crystal Vue, 5D Follicle), high-density sensors.
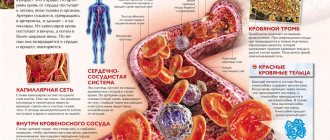
Anemia is characterized by a decrease in the level of hemoglobin in the blood, a decrease in the number of erythrocytes (red blood cells), the appearance of their pathological forms, as well as changes in the vitamin balance, a decrease in the amount of microelements and enzymes in the body. Anemia is one of the most common complications of pregnancy. The leading sign of anemia in pregnant women is a decrease in hemoglobin level to less than 110 g/l. Anemia in pregnant women in 90% of cases is iron deficiency. This anemia is characterized by a violation of hemoglobin synthesis due to iron deficiency developing as a result of various physiological and pathological processes. According to WHO, the incidence of iron deficiency anemia in pregnant women ranges from 21 to 80%. The presence of iron deficiency anemia leads to a disruption in the quality of life of patients, reduces their performance, and causes functional disorders in many organs and systems. Iron deficiency in pregnant women increases the risk of complications during childbirth, and in the absence of timely and adequate treatment, iron deficiency may also occur in the fetus.
The human body contains about 4 g of iron, which is one of the elements vital for the body. It is part of hemoglobin and a number of other vital substances that affect the function of various organs and systems in the human body. 75% of the iron in the human body is found in hemoglobin. Iron is most fully absorbed from animal products (meat), and much worse from plant foods. The release of iron from foods is reduced when they are cooked, frozen, or stored for a long time.
Iron is excreted from a woman’s body in the amount of 2-3 mg per day through the intestines, bile, urine, through the exfoliating epithelium of the skin, during lactation and menstruation.
In non-pregnant women, the iron requirement is 1.5 mg per day. During pregnancy, the need for iron steadily increases in the first trimester by 1 mg per day, in the second trimester - by 2 mg per day, in the third trimester - by 3-5 mg per day. To produce additional iron, 300 - 540 mg of this element is used. Of these, 250 - 300 mg of iron is spent on the needs of the fetus, 50 - 100 mg on the construction of the placenta, 50 mg of iron is deposited in the myometrium. Iron loss is most pronounced in 16-20 weeks of pregnancy, which coincides with the period when the process of hematopoiesis begins in the fetus and the increase in blood mass in the pregnant woman. In the third stage of labor (with physiological blood loss), 200 to 700 mg of iron is lost. Later, during lactation, another 200 mg. Thus, about 800 - 950 mg of iron is consumed from the maternal depot during pregnancy and the postpartum period. The body is able to restore iron reserves within 4-5 years. If a woman plans a pregnancy before this period, she will inevitably develop anemia. Iron deficiency cannot but occur in multiparous women.
Of interest are some indicators (presented in the table) of peripheral blood depending on the duration of pregnancy.
Table.
Some peripheral blood parameters in different trimesters of pregnancy.
| Indicators | 1st trimester | 2nd trimester | 3rd trimester |
| Hemoglobin, g/l | 131 (112-165) | 126 (110-144) | 112 (110-140) |
| Hematocrit, % | 33 | 36 | 34 |
| Red blood cells, 1012/l | 10,2 | 10,5 | 10,4 |
| ESR mm/hour | 24 | 45 | 52 |
Prevention of anemia, first of all, should be carried out among pregnant women who are at high risk of developing it.
Factors contributing to the development of iron deficiency anemia
- Reduced iron intake from food (vegetarian diet, anorexia).
- Chronic diseases of internal organs (rheumatism, heart defects, pyelonephritis, hepatitis). In liver diseases, the processes of iron accumulation in the body and its transportation are disrupted. Particular attention should be paid to diseases of the gastrointestinal tract. Gastrointestinal bleeding due to gastric and duodenal ulcers, hemorrhoids, as well as intestinal diverticulosis, ulcerative colitis, and helminthic infestation lead to anemia in patients.
- The presence of diseases manifested by chronic nosebleeds (thrombocytopathies, thrombocytopenic purpura).
- Gynecological diseases accompanied by heavy menstruation or uterine bleeding, endometriosis, uterine fibroids.
- Complicated obstetric history: multiparous women; history of spontaneous miscarriages; bleeding in previous births contribute to the depletion of iron stores in the body.
- Complicated course of this pregnancy: multiple pregnancy; early toxicosis; young age of the pregnant woman (under 17 years); primigravidas over 30 years of age; arterial hypotension; exacerbation of chronic infectious diseases during pregnancy; gestosis; placenta previa; premature placental abruption.
Pregnancy is contraindicated in the following forms of diseases of the blood and hematopoietic system: chronic iron deficiency anemia of III-IY degree; hemolytic anemia; bone marrow hypo- and aplasia; leukemia; Werlhof's disease with frequent exacerbations. If pregnancy occurs due to these diseases, it is advisable to terminate the pregnancy before 12 weeks.
The development of anemia during pregnancy is facilitated by: metabolic changes occurring in the patient’s body during pregnancy; decrease in the concentration of a number of vitamins and microelements - cobalt, manganese, zinc, nickel; changes in hormonal balance during pregnancy, in particular, an increase in the amount of estradiol, which causes inhibition of erythropoiesis; deficiency in the body of a pregnant woman of vitamin B12, folic acid and protein; lack of oxygen, which disrupts redox processes in a woman’s body; immunological changes in the body of a pregnant woman, occurring due to constant antigenic stimulation of the maternal body from the tissues of the developing fetus; consumption of iron from the depot of the mother’s body, necessary for the proper development of the fetus.
During pregnancy, so-called physiological or “false” anemia may also occur. The occurrence of this form is due to an uneven increase in individual blood components. The fact is that during pregnancy, as a compensatory reaction, there is an increase of 30 - 50% in the volume of the mother's blood, but mainly due to plasma (the liquid part of the blood). Accordingly, the ratio of the volume of blood cells (including red blood cells containing hemoglobin) and the liquid part of the blood (plasma) shifts towards the latter. This form of anemia does not require treatment.
Pathological forms of anemia during pregnancy
- Essential (cryptogenic) malignant anemia of Birmer-Ehrlich (synonyms: megaloblastic anemia, pernicious anemia, Addison-Birmer anemia). This anemia is rare during pregnancy. This form of anemia is associated with a deficiency of vitamin B12 or folic acid. The development of anemia associated with vitamin B12 deficiency is facilitated by past infections, insufficient intake of this vitamin from food, diseases of the stomach and duodenum, the use of medications (acyclovir, anticonvulsants, nitrofurans, oral contraceptives) and Crohn's disease.
- Hypochromic anemia, which is a concomitant disease during pregnancy. Anemia can be a consequence or concomitant pathology of infectious diseases (sepsis) and parasitic infestations (helminthiasis, malaria) during pregnancy. Hypochromic anemia during pregnancy can occur as a result of liver disease, stomach disease, and nutritional dystrophies.
- Megaloblastic anemia associated with folic acid deficiency accounts for 1% of all anemias in pregnant women and most often develops in the third trimester of pregnancy, before childbirth and in the early postpartum period. Folic acid plays an important role in many physiological processes, participates in the synthesis of a number of amino acids, and plays a key role in cell division processes. Tissues with a high rate of cell division (bone marrow, intestinal mucosa) are characterized by an increased need for folic acid. Folic acid deficiency in the body occurs due to: insufficient content in the diet; increased need for folic acid (pregnancy, prematurity, hemolysis, cancer); impaired absorption and increased excretion from the body (some skin diseases, liver diseases). The daily requirement of a pregnant woman's body for folic acid increases to 400 mcg, and by the time of delivery - up to 800 mcg; the need for folic acid during lactation is 300 mcg. Hidden folic acid deficiency is observed in up to 1/3 of the total number of pregnant women. Folic acid deficiency adversely affects the course of pregnancy and fetal development. The full formation of the fetal nervous system is impossible if there is a deficiency of folic acid in the woman’s body. With such a deficiency, the formation of neural tube defects (anencephaly, encephalocele, spina bifida) is possible. Another important fact confirming the role of folic acid during pregnancy is the close relationship between the level of folic acid in the mother's body and the birth weight of the child. Several weeks before birth, the fetus uses the mother's folic acid to increase its own weight and replenish its folate reserves. As a result, in women with folic acid deficiency, the likelihood of having a child with malnutrition and a reduced supply of folic acid increases significantly. The main sources of folic acid in food are: raw green vegetables and fruits (especially oranges), beef liver.
- Hypo- or aplastic anemia, in which there is a sharp suppression of bone marrow hematopoiesis. The causes of this form of anemia are most often: ionizing radiation; taking medications (chloramphenicol, aminazine, butadione, cytostatics); entry into the body of chemicals (benzene, arsenic) that have a myelotoxic effect; chronic infectious diseases (viral hepatitis, pyelonephritis); autoimmune processes. The diagnosis is made based on the results of a bone marrow puncture, which reveals the complete disappearance of bone marrow elements and their replacement with adipose tissue and hemorrhages. The mortality rate for a pregnant woman with this form of anemia reaches 45%. Therefore, it is advisable to terminate pregnancy up to 12 weeks followed by splenectomy. If hypoplastic anemia is diagnosed in late pregnancy, surgical delivery by cesarean section combined with splenectomy is recommended.
- Hemolytic anemia is a large group of diseases, the main distinguishing feature of which is a shortening of the life of red blood cells due to their hemolysis. There are two main groups: hereditary and acquired.
- Microspherocytic hemolytic anemia is hereditary. It develops due to a defect in the structure of the erythrocyte membrane, which leads to the penetration of excess sodium into the cell and the accumulation of water. The red blood cells become spherical and are destroyed in the spleen.
- Autoimmune hemolytic anemia, in which the formation of antibodies to one’s own red blood cells occurs. There are symptomatic and idiopathic autoimmune hemolytic anemia. The symptomatic form includes anemia, which develops against the background of hemoblastoses, systemic lupus erythematosus, ulcerative colitis, chronic hepatitis, and malignant ones. The idiopathic form includes those cases of anemia when it is impossible to establish the underlying disease. Rarely occurs during pregnancy. The prognosis for the mother is favorable. Delivery is through the natural birth canal.
Symptoms of anemic syndrome
Anemic syndrome is manifested by a complex of nonspecific symptoms and is caused by insufficient oxygen supply to tissues. The main clinical manifestations of this pathology are general weakness, increased fatigue, dizziness, tinnitus, floaters before the eyes, tachycardia, shortness of breath during exercise, fainting, insomnia, headache and decreased performance.
The consequences of iron deficiency are: dry skin, formation of cracks on it; violation of the integrity of the epidermis; the appearance of ulcerations and cracks in the corners of the mouth with inflammation of surrounding tissues; changes in the nails (fragility, layering, transverse striations, nails become flat, take on a concave spoon-shaped shape); hair damage (hair splits, ends split). Due to iron deficiency, patients experience a burning sensation of the tongue; perversion of taste (desire to eat chalk, toothpaste, ashes, clay, sand, raw cereals); unhealthy addiction to certain odors (acetone, gasoline, kerosene, naphthalene); difficulty swallowing dry and solid foods; the appearance of a feeling of heaviness and abdominal pain, as with gastritis; urinary incontinence when coughing and laughing, nocturnal enuresis; muscle weakness; pale skin; arterial hypotension; low-grade fever. In severe forms of iron deficiency anemia, anemic myocardial dystrophy develops.
Complications of pregnancy with iron deficiency anemia
Due to the fact that during pregnancy, oxygen consumption increases by 15-33%, pregnant women with iron deficiency anemia are characterized by severe tissue hypoxia with the subsequent development of secondary metabolic disorders, which may be accompanied by the development of dystrophic changes in the myocardium and a violation of its contractility. Iron deficiency anemia is characterized by disturbances in protein metabolism with the occurrence of protein deficiency in the body, which leads to the development of edema in a pregnant woman. With iron deficiency anemia, degenerative processes develop in the uterus and placenta, which lead to disruption of its function and the formation of placental insufficiency. In this case, the developing fetus does not receive sufficient quantities of the nutrients and oxygen it needs, resulting in delayed fetal development. The main complications of pregnancy with iron deficiency anemia are: threat of miscarriage (20-42%); gestosis (40%); arterial hypotension (40%); premature placental abruption (25-35%); fetal growth retardation (25%); premature birth (11-42%). Childbirth is often complicated by bleeding. In the postpartum period, various inflammatory complications may occur (12%).
In addition to assessing standard indicators of a clinical blood test (hemoglobin, red blood cells, hematocrit, ESR), the diagnosis of iron deficiency anemia is based on the assessment of a number of other indicators, such as: color index, average hemoglobin content in a red blood cell, morphological picture of red blood cells, iron level in the blood serum. total iron-binding capacity of blood serum, and some others.
Diet for pregnant women with iron deficiency anemia
In addition to drug treatment, pregnant women with iron deficiency anemia are prescribed a special diet. 2.5 mg of iron per day is absorbed from food, while 15-20 times more from medications. The greatest amount of iron is found in meat products. The iron they contain is absorbed by the human body by 25-30%. The absorption of iron from other products of animal origin (eggs, fish) is 10-15%, from plant products - only 3-5%.
The largest amount of iron (in mg per 100 g of product) is found in pork liver (19.0 mg), cocoa (12.5 mg), egg yolk (7.2 mg), heart (6.2 mg), veal liver ( 5.4 mg), stale bread (4.7 mg), apricots (4.9 mg), almonds (4.4 mg), turkey meat (3.8 mg), spinach (3.1 mg) and veal ( 2.9 mg). A pregnant woman with iron deficiency anemia should adhere to a balanced diet. Protein products are recommended: beef, bovine liver, tongue, liver and heart, poultry, eggs and cow's milk. Fats are found in: cheese, cottage cheese, sour cream, cream. Carbohydrates should be replenished with: wholemeal rye bread, vegetables (tomatoes, carrots, radishes, beets, pumpkin and cabbage), fruits (apricots, pomegranates, lemons, cherries), dried fruits (dried apricots, raisins, prunes), nuts, berries ( currants, rose hips, raspberries, strawberries, gooseberries), cereals (oatmeal, buckwheat, rice) and legumes (beans, peas, corn). Fresh herbs and honey must be included in your diet.
Prevention and treatment of iron deficiency anemia, use of iron medications
A necessary condition for the treatment of iron deficiency anemia is the use of iron medications, which are prescribed only by the attending physician. To prevent the development of iron deficiency anemia during pregnancy, the same drugs are used as to treat this complication. Prevention of the development of iron deficiency anemia in pregnant women at risk for the occurrence of this pathology consists of prescribing small doses of iron supplements (1-2 tablets per day) for 4 - 6 months, starting from 14 - 16 weeks of pregnancy, in courses of 2-3 weeks, with breaks for 14 - 21 days, a total of 3 - 5 courses per pregnancy. At the same time, it is necessary to change the diet in favor of increasing the consumption of foods containing large amounts of easily digestible iron. According to WHO recommendations, all women during the second and third trimesters of pregnancy and in the first 6 months of lactation should take iron supplements. Treatment with iron supplements should be long-term. The hemoglobin content increases only at the end of the third week of therapy for iron deficiency anemia. Normalization of red blood counts occurs after 5 to 8 weeks of treatment.
It is most preferable to take iron supplements orally rather than by injection, since in the latter case various side effects may occur more often. In addition to iron, medications for the treatment of iron deficiency anemia contain various components that enhance iron absorption (cysteine, ascorbic acid, succinic acid, folic acid, fructose). For better tolerability, iron supplements should be taken with meals. It must be taken into account that under the influence of certain substances contained in food (phosphoric acid, phytin, tannin, calcium salts), as well as with the simultaneous use of a number of medications (tetracycline antibiotics, almagel), the absorption of iron in the body decreases.
It is preferable for pregnant women to prescribe iron supplements in combination with ascorbic acid, which is actively involved in the processes of iron metabolism in the body. The content of ascorbic acid should be 2-5 times higher than the amount of iron in the preparation. Currently, a number of effective drugs are used to treat anemia in pregnant women. The question of prescribing a specific drug, as well as its single dose, frequency of use and duration of treatment is decided only by the attending physician on an individual basis. The physician should also monitor the effectiveness of the treatment, which is best assessed by the level of transferrin and ferritin in the serum, and not by the level of hemoglobin and red blood cells.
Treatment with iron supplements should not be stopped after normalization of hemoglobin levels and red blood cell counts in the body. Normalizing hemoglobin levels in the body does not mean restoring iron reserves in it. For this purpose, WHO experts recommend that after 2-3 months of treatment and elimination of the hematological picture of anemia, do not stop therapy, but only halve the dose of the drug that was used to treat iron deficiency anemia. This course of treatment continues for 3 months. Even after completely restoring iron reserves in the body, it is advisable to take small doses of iron-containing drugs for six months.
Ultrasound machine HS40
Top seller in high class.
21.5″ high-definition monitor, advanced cardio package (Strain+, Stress Echo), expert capabilities for 3D ultrasound in obstetrics and gynecology practice (STIC, Crystal Vue, 5D Follicle), high-density sensors.
Normal hemoglobin levels at different stages of pregnancy
If in women of childbearing age the hemoglobin content in the blood is considered normal at the level of 120 grams per liter, then during pregnancy the norms change. Moreover, the hemoglobin content in the blood of a pregnant woman depends on the trimester:
- I trimester - 110 grams per liter;
- II trimester - 110 grams per liter;
- III trimester -105 grams per liter (lower limits of normal are given).
Increased iron requirements in early pregnancy are usually covered by reserves from the blood depot. That is why iron deficiency conditions are rarely diagnosed in the first trimester. By the second trimester, as we have already mentioned, if a woman does not take iron supplements and does not change her diet, depot reserves are depleted, which often leads to the development of anemia. The opposite situation is also possible, although with much less probability - an increase in the level of hemoglobin in the blood.
Elevated hemoglobin levels are a cause for concern
Hemoglobin levels are considered elevated when levels are above 150 grams per liter. The reasons for the increase may be
- hormonal changes,
- dehydration,
- heart failure,
- respiratory disorders,
- folic acid deficiency, etc.
An increased level of hemoglobin leads to an increase in blood viscosity and can cause a slowdown in blood circulation in the mother and child, and therefore lead to tissue nutritional disorders. The most dangerous consequences of high hemoglobin include thrombosis.
As measures designed to normalize hemoglobin levels, pregnant women are recommended to first review their diet (eat less meat, switch to vegetables, from which iron is absorbed to a lesser extent), adjust the schedule for taking vitamins and drink more.
Why is a low hemoglobin level dangerous for the expectant mother and baby?
Anemia diagnosed in an expectant mother can be mild (hemoglobin level in the range of 110–91 grams per liter), moderate – 90–81 grams per liter, and severe when the hemoglobin level falls below 80 grams per liter.
Stably reduced hemoglobin during pregnancy also poses a threat to the woman and child. The expectant mother may develop placental insufficiency. As a result, the fetus will experience a lack of oxygen (fetal hypoxia), which will lead to developmental delays.
In some cases, there is a risk of miscarriage or premature birth. During the postpartum period, women with low hemoglobin levels have an increased risk of infectious complications and low milk production. That is why the level of hemoglobin in the blood during pregnancy must be regularly assessed by donating blood for a general analysis. The latter is usually prescribed once every trimester. If the doctor notes deviations from the norm, then tests may be prescribed several times per trimester. In cases of severe anemia, a woman may be tested up to twice a month.
Symptoms
An asymptomatic course is typical for low hemoglobin during pregnancy. Basically, symptoms make themselves felt immediately after the level of iron in the blood begins to fall. Common symptoms include:
- pale skin
- dizziness
- fatigue
- low performance
- weakness in the body
- shortness of breath even with minimal physical activity
- fainting
- brittle nails
- increase in heart rate
- severe hair loss on the scalp
- sores and cracks in the corners of the mouth
- desire to eat unusual or unintended foods
- desire to smell something that is unpleasant for ordinary people
A pregnant woman may have 1-2 symptoms listed in this list, but in such cases there is no need to immediately diagnose yourself with anemia. A couple of symptoms may also indicate completely different conditions, including toxicosis of the first trimester and its consequences. Therefore, it is important to consult a doctor so that he can prescribe tests and conduct the necessary studies to make a clear diagnosis.
Consequences of low hemoglobin levels
- gestosis
The pregnant woman develops edema, her blood pressure rises, and protein is found in the urine when the appropriate analysis is performed. The liver cannot function normally, less protein is produced than the body needs, and water metabolism is significantly disrupted. If the course of gestosis is severe, the pregnant woman’s brain will lack oxygen, followed by headaches. Sometimes preeclampsia is diagnosed, and in the absence of therapeutic measures taken, eclampsia. In the latter case, the pregnancy is terminated for medical reasons.
- embryonic development delay
If there is not enough oxygen in the mother’s body, then the child also lacks it. Its development becomes slow, and first of all, a very important organ, the brain, suffers.
- risk of premature birth
Low hemoglobin during pregnancy can lead to early placental abruption. If medical assistance is not quickly provided, the fetus may die, and there is also a risk of death of the mother. If the third degree of anemia is observed, then in 12 cases out of 100 the child is born dead.
- risk of infectious diseases after childbirth
- bleeding during childbirth or weakness of labor
- lactation disorders
Among the long-term consequences, as scientists from the United States write, is senile dementia. The study, which was conducted over eleven years, showed that with low hemoglobin levels, the risk of dementia in the elderly increases by 41%. The reason is that oxygen starvation leads to the death of neurons.
Changes in coagulogram and clinical blood test parameters
Changes in the coagulogram of a pregnant woman are a natural physiological process associated with the appearance of the uteroplacental circulation. It is due to the fact that the pregnant woman’s body prepares for an increase in blood volume during pregnancy and for possible blood loss during childbirth.
During normal pregnancy, the activity of the blood coagulation system increases. This means that already in the 3rd month of pregnancy, fibrinogen increases, which reaches its maximum values on the eve of childbirth. Therefore, gynecologists reasonably recommend monitoring this indicator during pregnancy (once per trimester, if there are deviations in these indicators, more often, once a week).
Simultaneously with the increase in fibrinogen, the activity of the internal blood coagulation mechanism also increases, while the analysis shows a shortening of the activated partial thromboplastin time (aPTT). Other parts of the blood coagulation system, such as the coagulation blocker antithrombin III, also change during pregnancy. But as pregnancy progresses, there is a gradual decrease in the activity of this indicator.
But lupus anticoagulant should not be produced normally in a pregnant woman.
Pregnancy also affects the results of a general blood test. Indicators such as hemoglobin and hematocrit may decrease in the second half of pregnancy, and leukocytes, on the contrary, may increase.