Description of the analysis
Determination of mchc occurs through calculations based on basic data, such as hematocrit, obtained from a complete blood count. This index serves as a highly sensitive test for disruption of hemoglobin generation processes. The main advantage is that it is independent of the average volume of red blood cells.
Essentially mchc reflects the density of filling red blood cells with hemoglobin and is a very stable indicator. Therefore, mchc is often used as an indicator of errors in the operation of laboratory equipment. But do not confuse MCHC with MCV, as these are different indicators.
Preparing for analysis
Direct analyzes for mchc are not done; general analysis data (CCA) are used for calculations. To carry it out, blood is taken from a vein, the amount is up to 3 ml. If certain indicators are present, it is possible to take capillary blood; such an analysis is prescribed for children under 3 years of age, patients with pathologies of the blood coagulation system.
No special preparation is required for a general blood test. Blood sampling is performed in the morning, on an empty stomach, or at any convenient time of the day. The main condition is not to eat for at least 8 hours before the test. You can drink water, but not coffee, tea or sweet drinks.
To increase the reliability of the data obtained, it is recommended to avoid stress, excessive physical and psycho-emotional stress 1-2 days before blood collection. You should avoid drinking alcohol.
How to prepare for the test
To obtain the most reliable data, it is recommended to carry out a number of preparatory activities. They will help not to “blur” the overall picture and accurately diagnose any deviation from the norm. Before taking blood, you must refrain from eating at least 4 hours before the procedure. It is also recommended to exclude heavy physical activity, emotional disorders and stress the day before. When taking any medications, you should talk in advance with your doctor, who can evaluate their composition and understand whether taking them can affect the analysis. If medications affect the results, you will need to limit their use a few days before the test. You also need to stop drinking alcoholic beverages and drugs. To achieve reliability, it is better not to smoke before analysis.
The best option is to visit the laboratory in the morning, on an empty stomach. In the morning you are allowed to drink only a glass of clean water. Strong tea, coffee and any other snack are not allowed. If it is necessary to donate blood several times to monitor therapy or more detailed diagnostics, then it is best to do this at the same time and in a similar condition. It is also worth contacting an identical clinic or laboratory. By adhering to these rules, the influence of third-party factors on the results obtained will be reduced to almost zero.
MCHC blood test explanation
A normal mchc value is considered to be between 310 and 380 g/l. Such values are considered the norm for adults of both sexes. In newborns, children, and adolescents, the normal limits are shifted downward. For children under 1 year of age, the average amount of hemoglobin in a red blood cell is considered to be 290-370 g/l.
After the completion of puberty, the normal concentration of iron-containing proteins stabilizes and remains throughout life within certain limits (in the absence of pathologies that can affect this indicator).
It is important to consider that finding the mchc index in the range of normal values does not always mean the absence of pathologies. There are anemia and other diseases that do not manifest themselves as a change in the mchc level in a blood test.
What does it mean if monocytes are elevated?
In a normal state, the number of monocytes in the blood is as follows (per 1 liter of blood):
- for adults: from 0.04 to 0.08*109 cell units;
- for children: from 0.05 to 1.1 * 109 cell units.
If we talk about the norm in relative terms, then the number of monocytes should be 1% -10% of the total mass of leukocytes. Moreover, for children the optimal range is from 2% to 7%, and for adults – from 1% to 8%. If the concentration is greater than the specified values, this indicates increased monocytes in the blood. This disorder is called monocytosis.
MCHC in blood test is increased
A high mchc index occurs when the concentration of iron-containing proteins in red blood cells increases. Such conditions are usually observed in various genetic pathologies. The most common:
- Hereditary spherocytosis. This is a disease in which the formation of the erythrocyte cytoskeleton is disrupted. As a result, the surface area of the cell membrane decreases, its plasticity is disrupted, and the concentration of hemoglobin in the cell increases significantly. You can find out about the analysis of hemoglobin levels here. Spherocytosis often occurs in hidden, benign forms and is detected only during screening diagnostics.
- Sickle cell anemia. One of the most common congenital diseases of red blood cells. As a result of disturbances in the process of hemoglobin production, red blood cells acquire a changed shape, and the mchc index increases. In such patients, hemoglobin has a different structure from the norm and carries oxygen less efficiently. If pathological genes are passed on from one of the parents, the disease occurs in a latent or mild form and provides immunity from malaria. When receiving defective genes from the mother and father, sickle cell anemia is severe and can cause serious pathologies and death.
- Hemoglobinosis C. A severe hereditary pathology that develops when both parents receive defective genes that direct the synthesis of erythrocyte proteins. Manifests itself in the form of hemolytic jaundice, chronic anemia, the most common complication is cholelithiasis. Defective hemoglobin is produced by the body in significant quantities because it carries oxygen worse than normal protein. As a result, a sharp increase in mchc index values is observed.
An increase in the mchc index does not always serve as a signal for the development of pathological processes. This figure may increase as the body recovers after severe blood loss. For residents of high mountains, an increase in hemoglobin concentration is a normal option as it serves to compensate for the low oxygen content in the air.
Therefore, professional climbers may experience a significant increase in the mchc index, which, in the absence of other pathological symptoms, should be assessed as normal.
MEDICAL CENTER
Interpretation of study results contains information for the attending physician and is not a diagnosis.
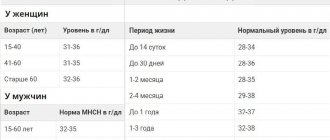
The information in this section should not be used for self-diagnosis or self-treatment. The doctor makes an accurate diagnosis using both the results of this examination and the necessary information from other sources: medical history, results of other examinations, etc. Hemoglobin (Hb, hemoglobin) Units of measurement in the medical center STUDIO DOCTOR: g/dl. Alternative units: g/l. Conversion factor: g/l x 0.1 ==> g/dl. Reference values
| Age, gender | Hemoglobin level, g/dl | |
| Children | ||
| 1 day - 14 days | 13,4 — 19,8 | |
| 14 days - 4.3 weeks | 10,7 — 17,1 | |
| 4.3 weeks - 8.6 weeks | 9,4 — 13,0 | |
| 8.6 weeks - 4 months | 10,3 — 14,1 | |
| 4 months – 6 months | 11,1 — 14,1 | |
| 6 months – 9 months | 11,4 — 14,0 | |
| 9 months - 12 months | 11,3 — 14,1 | |
| 12 months - 5 years | 11,0 — 14,0 | |
| 5 years - 10 years | 11,5 — 14,5 | |
| 10 years - 12 years | 12,0 — 15,0 | |
| 12 years - 15 years | Women | 11,5 — 15,0 |
| Men | 12,0 — 16,0 | |
| 15 years - 18 years | Women | 11,7 — 15,3 |
| Men | 11,7 — 16,6 | |
| 18 years - 45 years | Women | 11,7 — 15,5 |
| Men | 13,2 — 17,3 | |
| 45 years - 65 years | Women | 11,7 — 16,0 |
| Men | 13,1 — 17,2 | |
| > 65 years old | Women | 11,7 — 16,1 |
| Men | 12,6 — 17,4 | |
Increased hemoglobin levels:
- dehydration (with severe diarrhea, vomiting, increased sweating, diabetes, burn disease, peritonitis);
- physiological erythrocytosis (in residents of high mountains, pilots, athletes);
- symptomatic erythrocytosis (with insufficiency of the respiratory and cardiovascular systems, polycystic kidney disease);
- erythremia.
Decreased hemoglobin:
- anemia of various etiologies;
- overhydration.
Hematocrit (Ht, hematocrit)
Units of measurement in the medical center STUDIO DOCTOR: %.
Reference values
| Age, gender | Hematocrit indicator, % | |
| Children | ||
| 1 day - 14 days | 41,0 — 65,0 | |
| 14 days - 4.3 weeks | 33,0 — 55,0 | |
| 4.3 weeks - 8.6 weeks | 28,0 — 42,0 | |
| 8.6 weeks - 4 months | 32,0 — 44,0 | |
| 4 months – 9 months | 32,0 — 40,0 | |
| 9 months - 12 months | 33,0 — 41,0 | |
| 12 months - 3 years | 32,0 — 40,0 | |
| 3 years - 6 years | 32,0 — 42,0 | |
| 6 years - 9 years | 33,0 — 41,0 | |
| 9 years - 12 years | 34,0 — 43,0 | |
| 12 years - 15 years | Women | 34,0 — 44,0 |
| Men | 35,0 — 45,0 | |
| 15 years - 18 years | Women | 34,0 — 44,0 |
| Men | 37,0 — 48,0 | |
| 18 years - 45 years | Women | 35,0 — 45,0 |
| Men | 39,0 — 49,0 | |
| 45 years - 65 years | Women | 35,0 — 47,0 |
| Men | 39,0 — 50,0 | |
| 65 years - 120 years | Women | 35,0 — 47,0 |
| Men | 37,0 — 51,0 | |
Increased hematocrit:
- dehydration (with severe diarrhea, vomiting, increased sweating, diabetes, burn disease, peritonitis);
- physiological erythrocytosis (in residents of high mountains, pilots, athletes);
- symptomatic erythrocytosis (with insufficiency of the respiratory and cardiovascular systems, polycystic kidney disease);
- erythremia.
Decreased hematocrit:
- anemia of various etiologies;
- overhydration.
Red blood cells
Units of measurement at the STUDIO DOCTOR medical center: million/µl (106/µl). Alternative units: 1012 cells/L.
Conversion factors: 1012 cells/l = 106 cells/μl = million/μl.
Reference values
| Age, gender | Red blood cells, million/µl (x106/µl) | |
| Children | ||
| 1 day - 14 days | 3,90 — 5,90 | |
| 14 days - 4.3 weeks | 3,30 — 5,30 | |
| 4.3 weeks - 4 months | 3,50 — 5,10 | |
| 4 months – 6 months | 3,90 — 5,50 | |
| 6 months – 9 months | 4,00 — 5,30 | |
| 9 months - 12 months | 4,10 — 5,30 | |
| 12 months - 3 years | 3,80 — 4,80 | |
| 3 years - 6 years | 3,70 — 4,90 | |
| 6 years - 9 years | 3,80 — 4,90 | |
| 9 years - 12 years | 3,90 — 5,10 | |
| 12 years - 15 years | Women | 3,80 — 5,00 |
| Men | 4,10 — 5,20 | |
| 15 years - 18 years | Women | 3,90 — 5,10 |
| Men | 4,20 — 5,60 | |
| 18 years - 45 years | Women | 3,80 — 5,10 |
| Men | 4,30 — 5,70 | |
| 45 years - 65 years | Women | 3,80 — 5,30 |
| Men | 4,20 — 5,60 | |
| 65 years - 120 years | Women | 3,80 — 5,20 |
| Men | 3,80 — 5,80 | |
Increased red blood cell concentration:
- dehydration (with severe diarrhea, vomiting, increased sweating, diabetes, burn disease, peritonitis);
- physiological erythrocytosis (in residents of high mountains, pilots, athletes);
- symptomatic erythrocytosis (with insufficiency of the respiratory and cardiovascular systems, polycystic kidney disease);
- erythremia.
Decreased red blood cell concentration:
- anemia of various etiologies;
- overhydration.
MCV (mean erythrocyte volume) Determination method: calculated value. Units of measurement at the STUDIO DOCTOR medical center: fl (femtoliter). Reference values
| Age, gender | Mean erythrocyte volume, MCV, fl | |
| Children | ||
| 1 day - 14 days | 88,0 — 140,0 | |
| 14 days - 4.3 weeks | 91,0 — 112,0 | |
| 4.3 weeks - 8.6 weeks | 84,0 — 106,0 | |
| 8.6 weeks - 4 months | 76,0 — 97,0 | |
| 4 months – 6 months | 68,0 — 85,0 | |
| 6 months – 9 months | 70,0 — 85,0 | |
| 9 months - 12 months | 71,0 — 84,0 | |
| 12 months - 5 years | 73,0 — 85,0 | |
| 5 years - 10 years | 75,0 — 87,0 | |
| 10 years - 12 years | 76,0 — 90,0 | |
| 12 years - 15 years | Women | 73,0 — 95,0 |
| Men | 77,0 — 94,0 | |
| 15 years - 18 years | Women | 78,0 — 98,0 |
| Men | 79,0 — 95,0 | |
| 18 years - 45 years | Women | 81,0 — 100,0 |
| Men | 80,0 — 99,0 | |
| 45 years - 65 years | Women | 81,0 — 101,0 |
| Men | 81,0 — 101,0 | |
| 65 years - 120 years | Women | 81,0 — 102,0 |
| Men | 83,0 — 103,0 | |
Increasing MCV values:
- B12 deficiency and folate deficiency anemia;
- aplastic anemia;
- liver diseases;
- hypothyroidism;
- autoimmune anemia;
- smoking and drinking alcohol.
Reducing MCV values:
- Iron-deficiency anemia;
- anemia of chronic diseases;
- thalassemia;
- some types of hemoglobinopathies.
It should be taken into account that the MCV value is not specific; the indicator should be used to diagnose anemia only in combination with other indicators of a general blood test and biochemical blood test.
RDW (Red cell Distribution Width, distribution of red blood cells by size)
Method of determination: calculated value Units of measurement in the medical center STUDIO DOCTOR: %
Reference values
< 6 months — 14.9 – 18.7
> 6 months — 11.6 – 14.8
Increasing RDW values:
- anemia with heterogeneity of red blood cell size, including those associated with nutrition; myelodysplastic, megaloblastic and sideroblastic types; anemia accompanying myelophthisis; homozygous thalassemia and some homozygous hemoglobinopathies;
- a significant increase in the number of reticulocytes (for example, due to successful treatment of anemia);
- condition after red blood cell transfusion;
- interferences – cold agglutinins, chronic lymphocytic leukemia (high number of leukocytes), hyperglycemia.
There are also a number of anemias that are not characterized by an increase in RDW:
- anemia of chronic diseases;
- anemia due to acute blood loss;
- aplastic anemia
- some genetically determined diseases (thalassemia, congenital spherocytosis, presence of hemoglobin E).
It should be taken into account that the value of the RDW indicator is not specific; the indicator should be used to diagnose anemia only in combination with other indicators of a general blood test and biochemical blood test.
MCH (average amount of hemoglobin in 1 red blood cell)
Determination method: calculated value.
Units of measurement and conversion factors: pg (picograms).
Reference values
| Age, gender | Average hemoglobin content in 1 red blood cell, MCH, pg | |
| Children | ||
| 1 day - 14 days | 30,0 — 37,0 | |
| 14 days - 4.3 weeks | 29,0 — 36,0 | |
| 4.3 weeks - 8.6 weeks | 27,0 — 34,0 | |
| 8.6 weeks - 4 months | 25,0 — 32,0 | |
| 4 months – 6 months | 24,0 — 30,0 | |
| 6 months – 9 months | 25,0 — 30,0 | |
| 9 months - 12 months | 24,0 — 30,0 | |
| 12 months - 3 years | 22,0 — 30,0 | |
| 3 years - 6 years | 25,0 — 31,0 | |
| 6 years - 9 years | 25,0 — 31,0 | |
| 9 years - 15 years | 26,0- 32,0 | |
| 15 - 18 years old | Women | 26,0 — 34,0 |
| Men | 27,0 — 32,0 | |
| 18 – 45 years old | Women | 27,0 — 34,0 |
| Men | 27,0 — 34,0 | |
| 45 – 65 years | Women | 27,0 — 34,0 |
| Men | 27,0 — 35,0 | |
| 65 years - 120 years | Women | 27,0 — 35,0 |
| Men | 27,0 — 34,0 | |
Increasing MCH values:
- B12 deficiency and folate deficiency anemia;
- aplastic anemia;
- liver diseases;
- hypothyroidism;
- autoimmune anemia;
- smoking and drinking alcohol.
MCH Downgrade:
- Iron-deficiency anemia;
- anemia of chronic diseases;
- some types of hemoglobinopathies.
It should be taken into account that the MCH value is not specific; the indicator should be used to diagnose anemia only in combination with other indicators of a general blood test and biochemical blood test. MCHC (mean erythrocyte hemoglobin concentration) Determination method: calculated value
Units of measurement at the STUDIO DOCTOR medical center: g/dl. Alternative units: g/l. Conversion factor: g/l x 0.1 ==> g/dl.
Reference values
| Age, gender | Average hemoglobin concentration in erythrocytes, MSHC, g/dl | |
| Children | ||
| 1 day - 14 days | 28,0 — 35,0 | |
| 14 days - 4.3 weeks | 28,0 — 36,0 | |
| 4.3 weeks - 8.6 weeks | 28,0 — 35,0 | |
| 8.6 weeks - 4 months | 29,0 — 37,0 | |
| 4 months – 12 months | 32,0 — 37,0 | |
| 12 months - 3 years | 32,0 — 38,0 | |
| 3 years - 12 years | 32,0 — 37,0 | |
| 12 years - 15 years | Women | 32,0 — 36,0 |
| Men | 32,0 — 37,0 | |
| 15 years - 18 years | Women | 32,0 — 36,0 |
| Men | 32,0 — 36,0 | |
| 18 years - 45 years | Women | 32,0 — 36,0 |
| Men | 32,0 — 37,0 | |
| 45 years - 65 years | Women | 31,0 — 36,0 |
| Men | 32,0 — 36,0 | |
| 65 years - 120 years | Women | 32,0 — 36,0 |
| Men | 31,0 — 36,0 | |
Increased MSHC values: hereditary microspherocytic anemia. Decrease in MCHC values:
- Iron-deficiency anemia;
- anemia of chronic diseases;
- some types of hemoglobinopathies.
It should be taken into account that the MCHC value is not specific; the indicator should be used to diagnose anemia only in combination with other indicators of a general blood test and biochemical blood test.
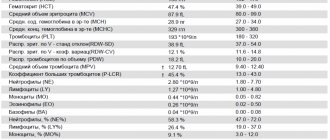
Platelets Determination method: conductometry using the hydrodynamic focusing method.
Determination method: conductometry using the hydrodynamic focusing method. Units of measurement at the STUDIO DOCTOR medical center: thousand/μL (103 cells/μL). Alternate units: 109 cells/L. Conversion factors: 109 cells/l = 103 cells/µl = thousand/µl. Reference values:
| Age | Platelet concentration, thousand/µl (103 cells/µl) | |
| Children | boys | girls |
| 1 day - 14 days | 218 — 419 | 144 — 449 |
| 14 days - 4.3 weeks | 248 — 586 | 279 — 571 |
| 4.3 weeks - 8.6 weeks | 229 — 562 | 331 — 597 |
| 8.6 weeks - 6 months | 244 — 529 | 247 — 580 |
| 6 months - 2 years | 206 — 445 | 214 — 459 |
| 2 years - 6 years | 202 — 403 | 189 — 394 |
| Age | Platelet concentration, thousand/µl (103 cells/µl) | |
| 6 years - 120 years | 150 — 400 | |
Increased platelet concentration:
- physical stress;
- inflammatory diseases, acute and chronic;
- hemolytic anemia;
- anemia due to acute or chronic blood loss;
- conditions after surgical interventions;
- condition after splenectomy;
- oncological diseases, including hemoblastosis.
Decreased platelet concentration:
- pregnancy;
- B12 deficiency and folate deficiency anemia;
- aplastic anemia;
- viral and bacterial infections;
- taking medications that inhibit platelet production;
- congenital thrombocytopenia;
- splenomegaly;
- autoimmune diseases;
- conditions after massive blood transfusions.
Leukocytes Determination method: conductometry using the hydrodynamic focusing method. Units of measurement at the STUDIO DOCTOR medical center: thousand/μL (103 cells/μL). Alternate units: 109 cells/L. Conversion factors: 109 cells/l = 103 cells/µl = thousand/µl. Reference values:
| Age | Leukocyte concentration, thousand/µl (103 cells/µl) |
| 1 day – 12 months | 6,0 – 17,5 |
| 12 months – 2 years | 6,0 – 17,0 |
| 2 years – 4 years | 5,5 – 15,5 |
| 4 years – 6 years | 5,0 – 14,5 |
| 6 years – 10 years | 4,50 – 13,5 |
| 10 years – 16 years | 4,50 – 13,0 |
| 16 years – 120 years | 4,50 – 11,0 |
Increased leukocyte concentration:
- physiological leukocytosis (emotional and physical stress, exposure to sunlight, cold, food intake, pregnancy, menstruation);
- inflammatory processes;
- viral and bacterial infections;
- conditions after undergoing surgical interventions;
- intoxication;
- burns and injuries;
- heart attacks of internal organs;
- malignant neoplasms;
- hemoblastoses.
Decreased leukocyte concentration:
- viral and some chronic infections;
- taking medications (antibiotics, cytostatics, non-steroidal anti-inflammatory drugs, thyreostatics, etc.);
- autoimmune diseases;
- exposure to ionizing radiation;
- wasting and cachexia;
- anemia;
- splenomegaly;
- hemoblastoses.
MCHC reduced
Deciphering the mchc blood test when the index decreases is required much more often. In this case, the concentration of iron-containing protein in red blood cells decreases, often so significantly that with direct microscopy, red blood cells become much less saturated in color.
This phenomenon is called blood hypochromia, and anemia that is accompanied by a decrease in this index is called hypochromic. There are many reasons for a decrease in mchc in a blood test, the most common are:
- Iron-deficiency anemia. Occurs when there is a lack of foods enriched with iron in the diet, or a violation of its absorption in the intestines. It is often found among vegetarians, since large amounts of iron are found in easily digestible form in meat and other animal products.
- Thalassemia. A hereditary disease associated with the transmission to a child of inheritance of defective genes responsible for coding the protein chains of hemoglobin.
- Anemia, which serves as a symptom of the development of pathologies of the liver, bone marrow, kidneys and other organs.
Another specific condition for which decreased mchc levels are a marker is lead poisoning. This toxic metal is dangerous in any concentration; it is widely used in various industries, so the likelihood of poisoning with it is quite high. Acute forms of poisoning are extremely rare; in chronic forms, this toxic metal gradually accumulates in the bones, nerve tissues, and bone marrow.
The hematopoietic function is inhibited, pathologies of the nervous system develop, and the kidneys and liver suffer. There are practically no specific symptoms for such poisonings, so if a patient has a decrease in mchc, the possibility of intoxication with this metal must be taken into account. Our medical center employs the best specialists who can explain each of the tests, and we also have the best prices for services in the city of Minsk.
What are monocytes in the blood
Monocytes are a type of leukocyte - white blood cells. These are large formations with large nuclei. They are involved in protecting the body from inflammatory processes. Monocytes can penetrate the walls of blood vessels, leaving the blood and rushing to the site of inflammation. They destroy bacteria, viruses, as well as dead cells of their own body. It turns out that monocytes perform an important sanitary function.
This is especially important during infectious diseases. For example, if a person is sick with the flu, at this moment many cells of the oropharynx and nasal cavity are destroyed. Then monocytes will arrive in large numbers to the appropriate areas and digest the dead parts of the cells. In this case, the tissues will recover faster, which will contribute to overall recovery.