What is the apical impulse and where is it located?
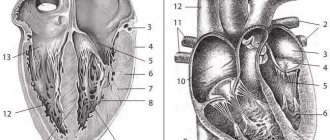
The heart is a muscle whose general function is to constantly pump blood through the body's circulatory system. It is located at the back of the sternum. Its apex is located above the diaphragm. When the heart beats, the muscles touch the chest wall, which can be felt by placing your hand on the left side of the chest.
The human heart is shaped like a pear. The apical or apical pulse is a heartbeat that is heard at the cardiac apex in the region of the left ventricle. This is one of the chambers of the heart that takes blood from the lungs, moves it to the aortic valve, then to the aortic arch, and the blood then flows through the rest of the body. It's a continuous cycle.
Heart rate is determined by the beat heard at the apex of the heart for one full minute. There are several reasons why this pulse is preferable to counting a detectable heartbeat from the wrist or neck. Some people experience irregular heartbeats that are not always transmitted to the arteries of the extremities.
Therefore, the pulse counted at the wrist may differ from the apical pulse.
The heart rate of young children and infants is estimated from the apical pulse because it is difficult to count the beat rate on the arms or legs of infants.
The apical impulse is normally a rhythmically pulsating protrusion of the intercostal space in the area of the cardiac apex onto the chest wall. It is created by tremors generated during systole. During diastole, the heart returns to its normal position. If the beat of the apex of the heart falls on the rib, then the push is invisible to the doctor.
The apical impulse can also be defined as a systolic protrusion of the space between the ribs. The point of the apical, apical pulsation can be found on the left side of the chest, just below the breast nipple. This position roughly corresponds to the lower pointed end of the heart.
Electrocardiogram
When the heart is excited, a potential difference arises between the excited (negative potential on the surface) and unexcited (positive potential on the surface) areas of the myocardium. Such a potential difference can be recorded using an electrocardiograph (a device for recording the biocurrents of the heart). The human body is a good conductor of current, therefore the biopotentials that arise in the heart can be registered on the surface of the human body. The biopotentials of the heart recorded using an electrocardiograph are called an electrocardiogram.
Rice. 7.6. Normal electrocardiogram in standard lead II
To record cardiac biocurrents, standard taps are used, in which the recording electrodes are located:
Lead I: right arm and left arm;
Lead II: right arm and left leg
Lead III: left arm and left leg.
A normal electrocardiogram (ECG) consists of waves, segments between them and intervals (Fig. 7.6).
The height of the teeth characterizes the characteristics of excitation, the duration - the speed of impulses in the heart. The ECG has 3 upward (positive) waves - P, R, T and two negative, downward waves - Q and S waves.
The P wave characterizes excitation in the atria, its amplitude is 0.2 mV (1/8 R), duration is 0.11 s.
PQ interval - reflects the time from the beginning of atrial depolarization to the beginning of ventricular depolarization and characterizes the speed of excitation in the atria, AV node, His bundle and its branches, its duration is 0.1-0.21 s.
Q wave - characterizes excitation of the interventricular septum, amplitude - ¼ R.
The R wave is the period of excitation coverage of both ventricles; is the main vector of the QRS complex, the amplitude in lead II is 1.6 mV.
The S wave is the period of completion of ventricular depolarization, amplitude is ¼ R.
The maximum duration of the ventricular QRS complex is 0.07-0.09 s.
Wave T (trophic) - the process of repolarization in the ventricles; duration - 0.16-1.24 s, amplitude - ½R.
The QT interval reflects the rate of depolarization (QRS) and repolarization (ST) of the ventricles; it is called electrical ventricular systolic, duration - 0.35-0.44 s.
The interval between the T wave and the subsequent P wave is the electrical diastole of the heart.
The RR interval (duration of the cardiac cycle) allows you to determine the heart rate (60 / RR in s). It is significant that with an increase in heart rate (tachycardia), the diastolic (TP) decreases significantly more than the systolic (QRST).
The electrical axis of the heart is the projection of the average resulting QRS vector onto the frontal plane. Normally, the position of the electrical axis of the heart approximately corresponds to the position of its anatomical axis.
The position of the electrical axis is expressed by the value of the angle alpha (a) formed by the electrical axis of the heart and the positive half of the axis and lead. Options for the position of the electrical axis of the heart: 1) normal, angle a is +30 ... + 69 °, 2) vertical, angle a is +70 ... + 90 °; 3) horizontal, the angle a varies from 0 to 29 °. The position of the electrical axis of the heart depends on both cardiac and post-cardiac factors. In people with a hypersthenic constitution, the electrical axis of the heart has a horizontal position or even a levogram appears. In tall, thin people, the electrical axis of the heart is normally located more vertically, sometimes to the right angle. Deviation of the axis to the right may indicate hypertrophy of the right ventricle, and to the left - left.
There are several methods for determining the electrical axis of the heart. The simplest of them, with sufficient reliability, is the following. Normally, in lead II, the value of the R wave is equal to the sum of the values of the R waves in leads I and III. If the amplitude of the R wave is large in lead I, then they speak of a livogram, if in lead III - a rightogram.
Properties normal and abnormal
The apex beat can be heard with your fingers or with a stethoscope. Both options are effective.
When listening to the pulse, you should pay attention to the speed of the heartbeat:
- A slow beat is normal for a person who is in good physical shape. But a slowdown may occur under the influence of certain medications.
- An increased pace in adults indicates that the person has high blood pressure or cardiac problems. It is also typical for people involved in physical exercise and young children.
Before palpation, the pulsation is examined by a doctor under direct and then lateral lighting. The angle of rotation during inspection changes to 90°.
The apical impulse provides a broad picture of cardiac activity to the physician and helps to establish the correct diagnosis.
| Character of the blow | ||
| Fine | Abnormal | |
| Short early (systolic) impulse, felt over an area of 2-3 cm² | Property of momentum | Possible violations |
| Hyperdynamic impulse (very short impulse of large amplitude) | Thyrotoxicosis, anemia, sepsis, vitamin deficiency, ventricular septal defect | |
| Pulsating impulse | Hypertension, aortic stenosis, | |
| Hypodynamic impulse (weak or absent apical impulse) | Myocardial infarction | |
All conclusions about the quality of the apical impulse are based in most cases on subjective analysis and many years of experience of doctors.
Positive and negative
The apical impulse is normally positive, as a rule. In rare cases it may be negative.
Under the influence of the formed pericardial adhesions, a symptom of a negative apical impulse is detected. This occurs when during systole the chest does not protrude at the site of the apical impulse, but is pulled inward.
In the zone of the V intercostal space at the moment of ventricular contraction, a vacuum is formed. As a result, the intercostal space is retracted and a negative apical impulse occurs.
With a positive push, a pulsating protrusion of the space between the ribs occurs.
In what cases is it not determined (not palpated)?
Some physical conditions interfere with the transmission of impulse from the apex to the chest wall:
- obesity;
- pericardial effusion;
- accumulation of fluid in the pleura;
- subcutaneous emphysema.
It is impossible to locate the apical impact site if there is spinal deformity, chest wall deformity, or tracheal deviation.
Why might it be displaced?
The apex beat is normally determined by a limited rhythmic beat. For some people, the impulse may have a diffuse pulsation, be stronger or weaker. The displacement of the apical impulse is influenced by changes in the heart or organs surrounding it.
| Pulse point | Reasons for displacement |
| Shift left | Mitral or aortic valve insufficiency, myocardial damage. Right-sided pleurisy, pneumothorax, hydrothorax, tricuspid valve insufficiency. |
| Offset right | Left-sided pneumothorax, hemothorax, left-sided exudative pleurisy, dextrocardia. |
| Deviation left and down | Aortic valve insufficiency (dilatation of the left ventricle). |
| Mixing towards the center | Displacement of the heart to the right due to left-sided hydrothorax, pneumothorax, pneumosclerosis. |
| Shift up and left | Occurs in conditions when the level of the diaphragm increases (flatulence, obesity, acidosis). |
Do not confuse thrust displacement with displacement. If the patient lies on the left side, then the apical pulsation shifts to the left by 3-4 cm. When lying on the right side, the displacement occurs to the right by 1.5 cm. In pregnant women with increased weight, the pulse moves to the left. For people with nicotine addiction - to the right.
A stable change in the location of the pulse, displacement, occurs due to internal disorders.
Width and area
The area of the apical impulse is determined by the width between II and IV and the fingers located at the outer and inner borders of the visible pulsation. The indicator for a healthy person does not exceed 2 cm. If the width is less than 2 cm, such a push is called limited.
An increase in area was noted among athletes and people engaged in heavy physical labor.
What affects the change in the area of the apex beat:
| Increased area | Reduced area |
| Myocarditis | Well developed muscles |
| Heart defects | Narrow intercostal spaces |
| Hypertension | Enhanced nutrition |
| Tumor of the posterior mediastinum | |
| Left ventricular dilatation |
The boundaries of the push are established at the 1st stage of palpation. The doctor gives a qualitative assessment during the 2nd stage of palpating the patient.
Spilled
A diffuse cardiac impulse can be felt in 2 or more intercostal spaces.
An enhanced apical impulse, the area of which is more than 2 cm² (spread), indicates hypertrophy of the right or both ventricles of the heart.
In case of enlargement of the left ventricle, the apical pulse is shifted downwards, has a local point, and is often strengthened.
Limited
A localized pulse is felt in the 5th intercostal space. The location is influenced by gender, human constitution, and the level of the diaphragm. In some women, the impulse is determined in the area of the IV intercostal space; in hypersthenics, it falls on the midclavicular line.
Height
A high apical pulse is determined by the amplitude of finger lifting and manifests itself in the following cases:
- accelerated heartbeat;
- high diaphragm position;
- deep exhalation, during which the cardiac apex moves closer to the chest wall;
- tumor of the posterior mediastinum;
- left ventricular hypertrophy.
Low shock occurs when:
- obesity;
- left-sided exudative pleurisy;
- pericarditis;
- deep breath;
- emphysema.
The apex beat normally has an average height. It is characteristic of normosthenics, people with a normal width of intercostal distances.
The range of oscillations of the intercostal space does not exceed 2-3 mm and depends on several factors:
- thickness of the chest wall;
- dynamics of myocardial contractility;
- hemodynamic type of state of the cardiovascular system.
Force
The strength of the apical impulse can be determined as follows:
- an increased push raises the finger;
- pulsating, of medium strength, easily identified, but the finger does not lift;
- a weak push is hard to find.
The strength of the pulsating impulse, as well as the area, depends on the location of the heart in the chest, but mainly on the contractile power of the left ventricle.
A pulsation of average strength is determined in a person with a moderate diet, standard physical development, and normal hemodynamics.
Intensified shocks occur with increasing speed and strength of contractile work of the left ventricle. It is observed more often in athletes, in people after emotional stress or workload. Pathological causes are associated with left ventricular hypertrophy, tumor of the posterior mediastinum, thyrotoxicosis, and shrinkage of the lung tissue.
Weak tremors can be detected in completely healthy people. These include patients with enhanced nutrition and powerfully developed muscles.
Pathologies affecting the decrease in thrust force:
- subcutaneous emphysema;
- obesity;
- left-sided pneumothorax;
- adhesive pericarditis;
- cardiosclerosis;
- heart defects.
The most alarming cause of decreased strength is a decrease in myocardial contractility.
If the doctor notices the simultaneity of changes in some parameters, then on this basis the following conclusions are drawn:
| Properties | Volume | Violation | Volume | Violation | Volume | Violation |
| Square | Increased | Normal myocardial contractility, muscle hypertrophy | Increased | Dilatation of the left ventricle, decrease in its functions | Reduced | Myocardial damage |
| Height | Increased | Increased | Reduced | |||
| Force | Increased | Reduced | Reduced |
The strength or weakness of the apical impulse is determined during a deep inspiration, and the patient should lie on his back.
Resistance
The presence of resistance is determined by the force of finger pressure that must be applied to “extinguish” the apical impulse. With high blood pressure, narrowing of the aortic mouth, obstacles arise for the flow of blood from the left ventricle to the aorta. This makes the apex impulse unyielding and resistant.
The pulse may be moderate when the tissue is perceived as pliable upon palpation. The impulse is called resistant if the tissue is dense, which occurs with left ventricular hypertrophy. The pulsation can become dome-shaped when the area and force of the push are increased. More often this occurs with aortic defects.
Other types of unwanted vibrations
In the case when the cardiac impulse becomes diffuse and affects other areas, such as the armpit, epigastric region, it becomes widespread. This condition is characteristic of heart disease.
In cardiology, the symptom of “cat purring” is also known. This occurs due to trembling of the chest wall. It is determined by digital or palmar palpation and is caused by low-frequency fluctuations in the blood flow that passes through the narrowed opening of the valve.
The detected sign is compared with the pulse in the carotid artery. If the beats coincide, then a systolic “purr” is detected. If the apical impulse and the blow on the carotid artery do not coincide, then a diastolic “purr” is noted.
Systolic tremors are characteristic of narrowing of the pulmonary artery. Diastolic manifests itself in stenosis of the right atrioventricular orifice, which is a rare defect.
Inspection and palpation of the heart area
05 May at 16:06 25212
Examination of the heart area When examining the heart area, attention should be paid to possible local deformations of the chest in patients with a variety of congenital and acquired heart diseases. In most cases, such deformations are based on pronounced ventricular hypertrophy.
If a disease (for example, a heart defect) developed in childhood, a noticeable protrusion of the chest wall in the area of the heart (heart hump) may occur. Retraction of the sternum is characteristic of congenital connective tissue dysplasia, which is often accompanied by lesions of the cardiovascular system (valve prolapse, abnormal chordae, etc.). When examining the region of the heart, one can also detect increased pulsation in the area of the apex or cardiac impulse, which indicates the presence of pronounced hypertrophy of the LV or RV myocardium. Increased pulsation at the base of the heart may be a sign of an aneurysm or diffuse dilatation of the aorta or pulmonary artery.
Palpation of the heart
Methodical palpation of the heart area often allows one to obtain extremely important information about the condition of the heart and large vessels.
In some cases, this simple method makes it possible to identify signs of left ventricular and right ventricular myocardial hypertrophy, dilatation of the heart cavities, dilation of the great vessels (indirectly) and aortic or left ventricular aneurysm. At the same time, the apex and cardiac impulse and epigastric pulsation are determined.
First, the apical impulse is always palpated, in most cases formed by the apex of the LV, then the cardiac impulse (the zone of absolute dullness of the heart) and the epigastric region, which to a certain extent reflect the state of the RV.
Apex beat
An increase in the apical impulse indicates hypertrophy of the LV myocardium, and its shift to the left and an increase in area (spread out apical impulse) indicate LV dilatation.
With concentric hypertrophy of the LV myocardium (without its dilation), the apex impulse is strengthened and concentrated, with eccentric hypertrophy it is strengthened and diffuse.
Displacements of the mediastinum, including the apical impulse, can also be caused by extracardiac reasons.
Heart beat
Epigastric pulsation
It is best determined at the height of a deep breath, when the heart, located on the diaphragm, moves down slightly. In a healthy person, it is often possible to detect a small transmission pulsation of the abdominal aorta, which decreases at the height of a deep inspiration.
In patients with eccentric hypertrophy of the pancreatic myocardium in the epigastric region, especially at the height of deep inspiration, increased diffuse pulsation is determined. Palpation of the great vessels includes the determination of pulsation and trembling in the region of the heart.
Determination of pulsation in the heart area
The fingertips are used to palpate the second intercostal space on the right (ascending aorta), to the left of the sternum (pulmonary artery trunk) and in the jugular notch (aortic arch). Normally, when palpating the area of the great vessels, it is sometimes possible to detect a weak pulsation only in the jugular notch.
Increased pulsation in the jugular notch may be associated with an increase in pulse pressure in the aorta with aortic insufficiency or hypertension or the presence of an aortic arch aneurysm; after significant physical activity, such an increase in pulsation is noted even in healthy individuals.
The appearance of significant pulsation in the second intercostal space to the left of the sternum usually indicates an expansion of the trunk of the artery, often as a result of pulmonary arterial hypertension.
Determination of tremors in the heart area
In the precordial region, the so-called systolic or diastolic tremor can sometimes be detected, caused by low-frequency shaking of the chest as a result of the transmission of vibrations that occur when blood passes through the narrowed valve openings.
– Diastolic flutter at the apex of the heart occurs when the left AV orifice is narrowed (mitral stenosis), when, during diastolic filling of the LV, blood from the left atrium (LA), encountering an obstruction in the area of the stenotic mitral valve, forms a turbulent flow.
– Systolic vibration in the aorta (in the second intercostal space to the right of the sternum and in the jugular notch) is detected in the case of narrowing of the aortic orifice. Below is a diagram that allows you to correctly interpret some of the changes revealed by palpation of the heart area.
Normal indicators in children and adults by age
Table of apical pulse indicators:
| Age group | Readings are normal |
| Newborns | 80 – 140 beats/min |
| Children from 4 to 9 years old | 75 – 120 beats/min. |
| Children under 15 years old | 50 -90 beats/min |
| Adults | 60 – 100 beats/min. |
The apex beat is normal in an adult if it does not exceed 100 or not lower than 60 beats/min. The ideal heart rate at rest and during physical activity varies from person to person.
Reasons why your heart rate may increase:
- fear or anxiety;
- heat;
- recent physical activity;
- pain;
- hypotension;
- blood loss;
- insufficient oxygen consumption.
Additionally, a heart rate that is consistently higher than normal may be a sign of heart disease, heart failure, or an overactive thyroid gland. The decrease is affected by medications that can affect the heart rate.
Heart sounds
These are sound manifestations of the work of the heart. they can be listened to using a phonendoscope or recorded using a phonocardiograph.
There are 4 heart sounds:
I tone - systolic.
Long, drawn-out, dull. It occurs due to the closure of the leaflet valves, tension in the ventricular muscles and tension in the tendon strands, as well as turbulence in the initial segments of the aorta and pulmonary trunk.
II tone - diastolic.
Short and sonorous. Occurs when the semilunar valves of the aorta and pulmonary trunk close.
The first two tones can be heard using a phonendoscope.
III tone - is formed as a result of vibration of the walls of the ventricles during their rapid filling with blood.
IV tone - is formed as a result of vibrations of the walls of the ventricles caused by the passage of blood during atrial systole.
Step-by-step palpation algorithm
Palpation of the apical pulse is carried out in 2 stages. To do this, landmarks on the body are used.
They include:
- bony point of the sternum;
- intercostal spaces;
- the midclavicular line (an imaginary line running down the body from the middle of the collarbone).
Stage I:
- The doctor stands to the right of the patient. The right hand is placed on the patient's chest. The base of the hand rests on the sternum, and the fingers cover the area from the III to VI ribs.
- The doctor presses the hand to the chest, bending the II, III, IV fingers, looking for the place of vibration of the intercostal space.
If the pulsation is not detected, the patient should lean forward 50°. This is done to bring the heart as close to the chest as possible. Before bending over, you need to exhale.
At the 2nd stage of palpation, the doctor determines the location of the push, type, area, strength, compliance, height.
Palpation technique:
- The doctor turns his hand with his fingers upward at the site of the found pulsation. The phalanges of the fingers should be located along the intercostal space.
- Slowly moving the fingers, slightly plunging them into the intercostal space, the doctor assesses the quality of the pulse.
The apex beat can be seen in only 50% of people. In others, it is hidden by a layer of fat, muscle, distance of the heart from the chest, or is affected by emphysema, which often accompanies older patients. Pulsation is clearly visible in asthenics, normosthenics and people with a thin fat and muscle layer.
Prevalence of cardiac pulsation
The area of protrusion of the cardiac impulse is about 2 cm². If it turns out to be larger, then they speak of a diffuse or widespread shock. With a smaller area it is limited.
Widespread pulsation occurs if the heart's larger surface is adjacent to the chest wall. This is observed:
- with a deep breath;
- pregnancy;
- at, etc.
In the absence of these conditions, a diffuse impulse may be the result of expansion of the heart (all or any of its parts).
A limited cardiac impulse occurs when the heart has a smaller area adjacent to the chest. The reason for this may be:
- emphysema;
- low aperture;
- hydro-, pneumopericardium.
What is a cardiac impulse?
The shaking of the anterior chest wall caused by the contraction of the heart is called a cardiac impulse. It occurs synchronously with ventricular systole.
In the tension phase, the shape and size of the heart changes, which makes it possible for the surface of the ventricles to come into contact with the chest wall. The study of the cardiac impulse is carried out using inspection, palpation, and a sound signal.
What does sound analysis provide?
Diagnostics requires identifying sounds that do not correspond to the norm. Therefore, an experienced doctor must be able to distinguish the “music” of regular heart contractions from pathological ones.
The muscular and valvular apparatus of the heart are in constant hard work. By driving a mass of blood from the chambers into the vessels, they cause vibration of nearby tissues and transmit sound vibrations to the chest from 5 to 800 Hz per second. The human ear can perceive sound in the range from 16 to 20,000 Hz, with the best sensitivity between 1000 and 4000 Hz. This means that a person does not have enough capabilities for an accurate diagnosis.
It takes practice and attention. Heard sounds should be perceived as information
Having received it, the doctor must:
- evaluate the origin in comparison with the norm;
- suggest the causes of violations;
- characterize.
Determination algorithm
The heartbeat is palpated as follows:
- The doctor's hand is placed on the precordial area, the fingers are at the level of the apical impulse, and the palm is at the right edge of the sternum, then palpation is performed. This is how the precordial region is assessed.
- Having assessed the condition at this level, the doctor’s hand moves to the third rib and palpation is also carried out here.
Thus, the doctor, with an existing cardiac impulse, distinguishes between the vibration of the lower part of the sternum, the pulse at the edges of the sternum and the epigastric pulsation.
Percussion technique and data
Percussion allows you to determine the size, configuration, position of the heart and the size of the vascular bundle.
First of all, you should take a position so that you can correctly place the pessimeter finger (press it tightly against the chest and parallel to the border being determined) and so that it is convenient to apply a percussion blow with your finger on the finger.
The heart of children should be percussed quietly, because the child’s chest is relatively thin and with strong impacts, nearby tissues will be involved in the oscillatory movements, which will not make it possible to correctly determine the boundaries of relative and absolute cardiac dullness. When determining absolute dullness of the heart, percussion should be as quiet as possible. It is necessary to percussion from a clear pulmonary sound to cardiac dullness.
Diseases detected by palpation, features of apical impulses in pathologies
The most common disorder that is revealed by palpation is an increase in the volume of the left ventricle, when the pressure in the systemic circulation steadily increases. This is affected by alcohol abuse and physical overload. This is an acquired pathology that is eliminated over time. But it is possible to identify other violations, more serious.
For hypertension
In the early stages, hypertension is not clearly expressed. However, even during this period, symptoms can be identified: headache, heart pain, vascular neurosis. The development of the disease is influenced by left ventricular hypertrophy. On palpation, an enhanced apical impulse is detected.
Other properties of apical pulsation:
- push is positive;
- spilled;
- resistant;
- domed in some cases;
- has a shift to the left and down.
With ventricular hypertrophy
This is a condition in which the muscles of the left ventricle thicken, often associated with uncontrolled hypertension. The process is not permanent, but in some cases can lead to heart failure. When the underlying problem is treated, the thickened ventricle may shrink in size over time.
With hypertrophy, the force of the apical impulse increases, a displacement occurs to the anterior axillary line, and down to the 6–7 intercostal space. The pulsation becomes diffuse, high, and takes on a dome-shaped shape.
For coronary heart disease
Insufficient supply of the heart muscle with oxygen and nutrients leads to myocardial damage. The main factor in the development of the disease is atherosclerosis of the coronary arteries, which reduces the blood supply to the heart muscle.
Upon visual examination of the heart area, the apex beat is not detected.
Upon palpation, the doctor determines:
- positive apical impulse;
- palpation of the pulse is carried out in the 5th intercostal space towards the outer side of the left midclavicular line;
- pulsation diffuse, low, resistant;
- shock area 3 cm².
Listening to the apical impulse is the most effective way to assess cardiac activity. If your pulse is outside the normal range or there is an irregular heartbeat, you should definitely visit a cardiologist.
Author: Belyaeva Anna
Technique for determining the boundaries of relative cardiac dullness
First, the right, then the left and upper boundaries are determined. Determination of the right border of relative dullness begins with determining the border of hepatic dullness along the right midclavicular line from the 3rd intercostal space down. Then the pessimeter finger is turned at a right angle, placed one intercostal space higher parallel to the right border of the heart and percussed towards the right edge of the sternum.
Having detected a shortening of the percussion sound, a mark is made along the outer edge of the finger. The right border is formed by the right atrium.
To define the left border
relative dullness of the heart, the apex impulse must first be found (it coincides with the left border of relative dullness and is formed by the left ventricle). If the apex beat cannot be detected, then percussion of the left border is carried out along the 4th or 5th intercostal space (depending on the age of the patient), starting from the midaxillary line. The pessimeter finger is placed parallel to the expected border and moved towards the heart. The finger strike should be directed from front to back, if possible, and not from left to right, because in the latter case, the posterior border of the heart is determined. Percussion is performed until shortening appears and a mark is also placed along the outer edge of the finger (along the edge facing the clear sound).
When determining the upper limit
relative dullness of the heart, a finger-pessimeter is placed at the left edge of the sternum (lin. parasternalis sin) parallel to the ribs and, starting from the 1st intercostal space, descends down the parasternal line. When a shortening of the percussion sound appears, a mark is made along the upper edge of the finger. It is formed by the cone of the pulmonary artery and the appendage of the left atrium.
Diameter of the heart
measured in centimeters - the distance from the right to the left borders of relative dullness (the sum of two terms).
To determine the configuration of the heart
percussion is carried out in the same way on the right and left and along other intercostal spaces (from the 5th to the 2nd) and the resulting points are connected to each other.
Determination of the boundaries of absolute cardiac dullness
(formed by the right ventricle) is performed according to the same rules, using the quietest percussion in the same order - right, left, and then the upper border.
To determine the right border
For absolute dullness, a finger-pessimeter is placed on the right border of relative dullness of the heart parallel to the right edge of the sternum and moved inward until an absolutely dull sound appears. A mark is made along its outer edge (facing the border of relative dullness).
To define the left border
For absolute dullness, the finger-pessimeter is placed parallel to the left border of relative dullness, slightly outward from it and percussed, moving the finger-pessimeter inward until a dull sound appears. The mark is placed along the outer edge of the finger.
When determining the upper limit
For absolute dullness, a finger-pessimeter is placed on the upper limit of relative dullness of the heart at the edge of the sternum parallel to the ribs and goes down until a dull sound appears. The mark is made along the edge of the finger facing upward.
Determination of the boundaries of the vascular bundle
performed by percussion along the 2nd intercostal space. The pessimeter finger is placed on the right along the midclavicular line parallel to the expected dullness and moved towards the sternum until a dull sound appears. A mark is made along the outer edge of the finger. Then percussion is performed on the left in the same way and a mark is made along the outer edge of the pessimeter finger. The distance between the marks is measured in centimeters.
What methods should a doctor know?
Narrow medical specialization does not exclude the general training of a general practitioner. The standard set of knowledge and skills of a novice doctor necessarily includes:
- personal examination of the patient;
- palpation - palpation of a dense organ, edge to determine consistency and size; pulse, area of the heart - to determine the shock wave, the force of the heart impulse;
- percussion - determining the boundaries of dullness by the nature of the sound obtained by tapping a finger over organs of different densities;
- Auscultation - listening to standard points of the body located above zones that are as close as possible to the movement of fluid inside hollow organs; the occurrence of noise depends on the speed of flow and obstacles.
Let us consider the possible results of using propaedeutics methods in the diagnosis of cardiac pathology.
Shift of the apical impulse to the left and down indicates left ventricular hypertrophy