Human blood is a liquid and mobile connective tissue of the body. Its structure is divided into two components: the liquid part - plasma and formed elements - erythrocyte cells, leukocytes and platelets. Blood performs many important functions in the body, including respiratory, protective, transport and excretory.
In case of serious blood loss, the patient needs a transfusion of donor material. This procedure saved a huge number of lives, but this would have been impossible without knowledge of the characteristics of blood, ignoring which will lead to incompatibility between the donor and the patient.
Classification
At this stage of development of medicine, it is known that there are two significant systems for classifying human blood - by Rh factor and group. Due to ignoring these parameters, the concept of “incompatibility” appeared.
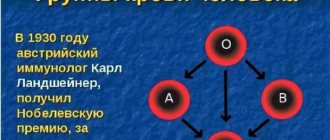
The first successful transfusion was recorded in France in the middle of the 17th century. However, we can say with confidence that this was luck, because doctors of that era had no idea about groups, did not know which blood group could be transfused to everyone, and lamb biomaterial was used as a donor. And only at the beginning of the 20th century, through a huge number of scientific studies, the scientist Karl Landsteiner proposed a classification into 4 groups, which is still used today.
A little history
Attempts at blood transfusion began several centuries ago. In those days, they did not yet know about possible blood incompatibility. Therefore, many transfusions ended unsuccessfully, and one could only hope for a lucky break. And only at the beginning of the last century one of the most important discoveries in hematology was made. In 1900, after numerous studies, an immunologist from Austria, K. Landsteiner, discovered that all people can be divided by blood into three types (A, B, C) and, in this regard, proposed his own transfusion scheme. A little later, his student described the fourth group. In 1940, Landsteiner made another discovery - the Rh factor. Thus, it became possible to avoid incompatibility and save many human lives.
However, there are cases when a transfusion is urgently needed, and there is no time or opportunity to look for a suitable donor, for example, this was the case at the front during the war. Therefore, doctors have always been interested in the question of which blood group is universal.
Blood groups
The system that separates blood according to this indicator is known as the AB0 system. According to it, they distinguish:
- The first group, sometimes called zero. Denoted by 0 (I).
- The second group, designated A (II).
- The third, designated B (III).
- And the fourth, whose designation is AB (IV).
What was the basis for this division? Protein molecules were found on red blood cells that turned out to be individual for each person. These include those that have a significant effect on the blood and its formation. These protein molecules are called antigens, or agglutinogens, and are designated A and B. Plasma may contain agglutinins, designated by the symbols α and β. The combination of these proteins determines the blood type.
Read also: Common causes of low white blood cells and platelets, symptoms and diagnosis
People with the first group do not have agglutinogens, while those with the second group have antigen A. Those in the third group have an antigen called B. The fourth group has both A and B, but lacks agglutinins. It is considered the rarest. People with group I are considered to be common, which, given its versatility, has become the main reason for the availability of a large amount of donor material. It's not hard to get.
Attention! A person is born with a certain blood type, which does not change with age and remains so throughout life.
When transfusion of the wrong type of blood occurs, red blood cells begin to stick together, it coagulates, and small vessels become blocked. High risk of fatal outcome. This process is triggered due to the ingress of antigens of the wrong type.
The process of determining blood identity
An important point in transfusion is to determine the identity of the biological fluid and the presence of infections in it. To do this, a blood sample is taken for a general analysis, the resulting amount is divided into two parts and sent for research. In the laboratory, the first one will be checked for the presence of infections, the amount of hemoglobin, etc. The second one is used to determine the blood type and its Rh factor.
Rhesus affiliation
Rhesus is another antigen found on red blood cells. If it is present, the blood is defined as Rh-positive; if the protein is absent, it is said to be Rh-negative. The majority of the population has a positive Rh factor; according to the latest information, the number of this part of people reaches 85%, the remaining 15% are Rh negative.
The indicator plays a critical role in the development of hemolytic disease of newborns. Pathology is the main cause of the formation of jaundice in the fetus. Due to Rh conflict, the child may begin to disintegrate his red blood cells, since his blood components are perceived as foreign to the woman’s body, resulting in the production of antibodies.
To determine the group and Rh factor, it is necessary to take a sample for analysis on an empty stomach. Despite the fact that food intake does not affect them, as in many other laboratory studies, the material is collected in the morning on an empty stomach.
What blood is most common?
According to statistics, about half of all inhabitants of the planet have blood of the first group, about 40% are carriers of the second, approximately 8% of the population have the third group, and only 2% of people have the fourth. The vast majority (85%) are owners of Rh-positive blood, and only 15% do not have a specific protein on the surface of red cells - the Rh factor. From this we can conclude that the best group is I positive, and this means that such blood can always be found, unlike the fourth negative.
Blood transfusion by group
The blood transfusion scheme allows you to take into account its group in each individual case. Transfusion is called blood transfusion. The procedure is performed when the human body is in critical condition, since, despite the millions of lives saved with its help, it carries a risk to the patient’s health. The branch of medicine that studies the mixing of biological fluids of the body and the problems of their compatibility is called transfusiology.
The person who donates material for transfusion (donation) is called a donor, and the one to whom it is transfused is called a recipient. During blood transfusion, the Rh factor and blood groups are taken into account. The material is transferred taking into account the following features:
Read also: Reasons for ordering a test for hormone concentrations in men
- For people with the first blood group, the same group will be suitable.
- Persons with the second group are allowed to transfuse the first and their own group.
- Third, people with grades I and III are suitable as donors.
- The fourth one can pour in all types of material.
Based on the table with the data, we can conclude which blood group is suitable for everyone: people with blood 0 (I) do not have antigens, due to which the first blood group is considered a universal donor. However, modern medicine does not encourage blood transfusion of this group. This practice is used only in critical situations. People with group IV are considered universal recipients, capable of receiving any biomaterial.
Important! For a successful blood transfusion procedure, it is not enough to know which blood group is suitable for all blood groups. Compliance with the Rh factor becomes a prerequisite; if inappropriate biomaterial is transfused, there is a high risk of Rh conflict.
How to find out your group and Rh factor?
Modern medicine offers a quick and reliable blood test to determine the group and presence of antigen. The procedure is quick and results are ready within 30 minutes. To determine the group, reference blood is added to blood samples and the classification is determined based on the results of the reaction.
If you carefully study your medical record and look at your passport, you can find out your blood type without visiting the clinic. From the first days of birth, blood is taken from the child for tests, this information is stored in the card. When you first go to the hospital at an older age, the data is duplicated in your passport.
So, having considered all types of blood and their compatibility, we can conclude that the first group 0 (I) is universal for transfusion, and only the owner of group AB (IV) can become an ideal recipient. Doctors (in order not to take risks) usually carry out transfusions of the same blood and only in rare cases, in non-standard and critical situations, are guided by the rules of compatibility with the obligatory consideration of Rh factors.
Indications for transfusion and risks
Blood transfusion is a test for the body, and for this reason, indications are needed to perform it. These include the following pathologies and abnormal conditions of the body:
- Diseases based on a lack of red blood cells (anemia), as a result of which the body is unable to independently form a sufficient number of these elements.
- Hematological diseases of malignant type.
- Significant blood loss resulting from injuries or accidents.
- Severe intoxication, the correction of which is impossible by other means.
- Complex operations that involve tissue damage and bleeding.
The introduction of donor material into the body increases the load on many systems, enhances metabolic processes, which provokes the development of pathologies. Therefore, a number of contraindications to the procedure are taken into account:
- myocardial infarction,
- suffered thrombosis,
- heart muscle defects,
- disorders of the kidneys and liver,
- acute form of cardiopulmonary failure,
- disorders in cerebral circulation, etc.
Compatibility tests when planning pregnancy
It should be noted that the Rh factor does not affect the course of the first pregnancy, but it must be determined in order to protect the woman and give her a chance to give birth to a second and subsequent children.
Therefore, future parents need to find out the compatibility of their Rhesus in advance. To check blood compatibility, both spouses must undergo tests at the planning stage.
Women who are Rh negative and planning a pregnancy with a Rh positive man should have a blood test done to check for antibodies. You can donate blood for antibodies even if you are already pregnant. In the latter case, this should be done as early as possible in order to prevent miscarriage and fetal diseases.
The concept of universality
During red blood cell transfusion, universal donors are people with blood type 1 and Rh negative. Patients with the fourth type and a positive presence of antigen D are universal recipients.
Such statements are only suitable if a person needs to receive a reaction of antigens A and B during a blood cell transfusion. Often such patients are sensitive to foreign positive Rh cells. If a person has the NN system - the Bombay phenotype, then such a rule does not apply to him. Such people can receive blood from NN donors. This is due to the fact that their erythrocytes have antibodies specifically against N.
Universal donors cannot be those who have antigens A, B or any other atypical elements. Their reactions are usually not taken into account often. The reason is that during transfusion, sometimes a very small amount of plasma is transported, in which foreign particles are directly located.
Heredity
When a new life is born, it depends only on the parents what blood type the baby will receive. An important role is played by the compatibility of parents during conception and pregnancy. The fact is that the genes of the mother and father are equally involved in the creation of a new person. The blood type in itself does not matter, and when different groups are combined, the child will receive either the blood of the mother or the father, or, through the process of mutation, a different type. But with different Rh factors, an immune reaction occurs. If the child has the antigen, but the mother does not, a Rh conflict occurs. Agglutinins are produced and proteins are destroyed. When positive and negative red blood cells meet again, a reaction of gluing and destruction of hematopoietic cells occurs. For the first pregnancy there is practically no danger, but during the second the mother’s blood contains such an amount of antibodies that it leads to hemolytic disease. To avoid unwanted reactions, therapy with anti-Rhesus globulin is carried out.
In what cases is blood transfusion required?
Transfusion is done due to severe blood loss. If the patient loses about 30% of blood within a few hours, then this procedure should be performed. It is also done urgently if a person is in shock after surgical treatment.
Transfusions are often prescribed to patients who have been diagnosed with anemia, serious blood diseases, inflammatory processes in the body and purulent-septic diseases, strong and severe intoxications of the body.
The procedure is prescribed to people with the following diseases:
- leukopenia – a sharp decrease in the level of leukocytes,
- hypoproteinemia – low level of protein in the blood,
- sepsis - infection of the blood by microbes,
- violation of ESR.
For transfusion, blood with all its components, drugs and blood substitutes are mixed. Medicines are added to the donor’s normal blood to increase the therapeutic effect, while reducing the risk of complications after the procedure.
Red blood cells are often injected into the patient's body. To do this, the red blood cells are first separated from the frozen plasma. After this, a liquid with a high concentration of red cells is poured into the recipient’s body. This method is used for anemia, acute blood loss, with the development of malignant tumors, after tissue and organ transplantation.
Read also: Indications for a blood test for bilirubin, norms and deviations
A mass of leukocytes is infused for agranulocytosis, when the level of these cells rapidly decreases, and for the treatment of severe complications of diseases of an infectious nature. After the procedure, the level of white cells in the blood increases, which has a beneficial effect on the course of recovery.
When to use fresh frozen plasma:
- severe blood loss,
- DIC syndrome,
- hemorrhages - blood leaks through damaged vessel walls,
- overdose of coagulants,
- diseases of an infectious nature.
Patients with blood diseases especially need transfusions. Some patients have to do this procedure once a week, or even more often.
Transfusions are also given to people after chemotherapy. If the tumor has affected the bone marrow, after therapy not only malignant cells stop growing, but also healthy ones.
Women often need transfusions after a difficult birth during which they lost a lot of blood. Sometimes doctors do not recommend using a man's blood for this. Women's is considered safer, and for a young mother this is especially important.
Chief Physician of the O.K. Blood Center Gavrilova DZM Olga Andreevna Mayorova - about how the capital’s blood service is organized, which blood components are most in demand and how a novice donor can organize the process with maximum comfort for themselves and benefit for the city.
Is there enough donor blood in Moscow now?
Fortunately, there is no shortage of blood and its components in the city. Difficulties can only arise with the selection of blood for patients with rare phenotypes and antibodies - but we are also solving this problem to the best of our ability by creating special reserves. The selection of blood components for recipients is carried out according to at least ten, and more often according to twenty to thirty different indicators. This is a rather complex and time-consuming process; sometimes it is difficult to choose the right material.
Perhaps for such complex patients it is possible to find a donor among relatives?
In fact, there are strict contraindications against the use of related donor blood. In some cases, patients may experience immunological reactions, especially with hematological diseases. We always try to find a non-relative donor for such patients. But we are happy to invite relatives, if they are ready for this, to make a reciprocal donation: someone helped you, and you help others. This is nothing more than a form of conscious gratitude.
Indeed, in Moscow there are several very difficult patients, whose names we know from memory: they need special, rare blood. As a rule, for them we keep a special supply of donor blood with a special mark: this saves us from the need in an acute moment to search for donors in the database and call them, asking them to urgently donate blood components.
What type of blood is usually missing?
There is an increased need for Rh negative blood components in the city: the number of Rh negative donors is decreasing from year to year. Why is this happening? Migration factors may have an influence: it is known that negative Rhesus is extremely rare among representatives of Asian peoples. We also note that recently even young donors are beginning to experience health problems earlier, and among our donors citizens over 40 years of age predominate. So, finding a healthy donor is becoming increasingly difficult.
In what seasons is donated blood most needed?
As a rule, the risk of a shortage of blood and its components in Moscow occurs during the New Year holidays, as well as in the summer. The reason here is not at all that the number of acute injuries is becoming more frequent: donors are simply leaving the city. We have learned to cope with the New Year holidays: we create blood reserves in advance. In addition, we continue to work on holidays: for the whole country the New Year holidays last 10 days, but for us it lasts no more than 5 days. With the summer holidays, the situation is more complicated: they are longer, and the volume of donor activity decreases significantly. In small towns it is quite possible to stock up on blood and its components in advance, but on the scale of Moscow, with its enormous needs, this is almost impossible. In addition, some blood components have a short shelf life - for example, platelets cannot be frozen and are stored for no longer than 5 days. It is impossible to make a full stock.
Which blood components can be preserved for a longer period – and in what way?
Each blood component has its own storage mode. Platelets , as I already said, are very vulnerable and difficult to freeze. They are stored at a temperature of 20-25 degrees, subject to continuous stirring - for this purpose special devices, thrombomixers with a thermostat are used. Fortunately, our service is well equipped with these devices. Red blood cells are stored at a temperature of +4 degrees - that is, under the conditions of a conventional pharmaceutical refrigerator. Shelf life - from 35 to 52 days, on average 42 days. They are frozen effectively: our center and several blood transfusion departments have the necessary supply of cryopreserved red blood cells. As for leukocytes , the donation of these elements is not our prerogative. This is an extremely labor-intensive process, which in Moscow is carried out by only one organization - the National Medical Research Center for Pediatric Hematology, Oncology and Immunology named after. D. Rogacheva. The lifespan of leukocytes is only a few hours, they are used mainly for severe forms of fungal sepsis, moreover, the donation process requires serious preparation, and, as a rule, they are donated only by career donors.
In our service, the most difficult component of blood to obtain is plasma . It freezes well, and its frozen shelf life is 3 years, however, unlike red blood cells and platelets, it cannot be immediately issued to city hospitals. To use plasma, the donor must be re-examined 6 months after donation. This is called quarantine: until we are sure that the donor is healthy, we do not have the right to transfer plasma to medical organizations.
What happens to the collected plasma if the donor for some reason does not show up for additional examination after quarantine?
In such a situation, there is a way to secure the plasma - for this you need to carry out a certain chemical treatment. As a result, we obtain pathogen-inactivated plasma, which can be used for medicinal purposes. However, this process is associated, firstly, with significant financial costs, and secondly, with some losses in plasma properties. It is best if the donor still finds the opportunity to come for the examination. But the components of donor blood, red blood cells and platelets, are sent to the medical network immediately after testing: the tests performed are enough to be sure of the quality of the blood.
What blood components are most in demand now?
In recent years, a general trend has been observed in world medicine: the consumption of red blood cells is increasing, and the consumption of plasma is falling. This is due to new trends in transfusiology, new aspects and technologies for the treatment of hematological and oncological diseases. Thus, now we often have to replace blood cells rather than plasma. There is even an excess of plasma in the city - but, fortunately, the decrease in consumption is offset by a long shelf life. Blood plasma is too valuable a material to be written off: the accumulated surplus will be used to produce medicines.
Can we say that the Moscow blood transfusion station is technically equipped enough to carry out all the tasks assigned to it?
Undoubtedly. Our station is equipped to the highest standard - and what's more, modernization has never stopped for us. We can say that we received the most modern equipment somewhat ahead of the curve, when the request for new methods of donation was at the formation stage. Today we have everything we need to supply the medical network with blood and its components.
We talked about blood components - is whole blood now donated for transfusions?
Currently, whole blood is transfused to patients only in special cases. Although this is not prohibited by law, medicine is already well aware of the risks of developing post-transfusion complications when transfusion of whole blood. Therefore, 99.9% of collected whole blood must be processed and separated into components - this is how we obtain red blood cells.
Are there any differences when donating various blood components? Does the donor feel them?
For each component, different sampling algorithms are provided. Donors are most familiar with whole blood donation: many experienced it for the first time centrally, in universities and enterprises. This is the simplest type of donation; it does not require any special devices and can be carried out on-site. Nowadays, blood is donated for red blood cells using this method. But donors donate plasma and platelets using apheresis technologies, only in a hospital setting - either in our blood center or in one of the departments. The process of donating plasma and platelets is much longer: a donor donates whole blood in 10 minutes, plasma in 40 minutes, and platelets in up to an hour and a half.
Who decides which blood components a donor will donate?
The decision is made by the transfusiologist during the reception and examination of the donor. However, every donor has the right to express their wishes and concerns. For example, for some it is very difficult to remain in the same position for an hour and a half - this means that it will be difficult for him to donate platelets. As a rule, experienced personnel donors are inclined towards a certain type of donation: our specialists do not interfere with this. But for the first time, only whole blood is donated. We must see how the donor will cope with blood loss, then find out the donor's infection status, and only then will he be given the opportunity to choose.
The donor's infection status is determined during the donation process - why not in advance?
Previously, it was indeed a common practice to take a blood test from a donor 1-2 days before donation. The danger is that a day or two before donating blood, the donor may be a carrier of an infection: the viral agent is in his blood, but markers of infectious diseases will not show this. Thus, we risk sending potentially contaminated blood to the city. With current practice, we are guaranteed to collect only healthy blood and its components from donors. Yes, some blood will be discarded based on infection tests, but usually this is no more than 1 percent of all cases.
That is, no more than 1 percent of donor blood is rejected?
The presence of infection is not the only reason why blood may be discarded. Other reasons are a lack of protein in the blood, a violation of tightness, deviations in certain biochemical parameters. In total, up to 5% of all donated blood is rejected. In all countries of the world, this figure is approximately the same: science does not yet know a way to significantly reduce the percentage of donor blood that is rejected.
Fortunately, we are often able to detect whether a donor has an infection at the registration stage: then he simply will not be allowed to donate, and the blood will not have to be discarded.
Have medical contraindications for donation changed in recent years? Are there new grounds for medical withdrawal?
All contraindications for donation are regulated by Order of the Ministry of Health of the Russian Federation No. 364 “On approval of the procedure for medical examination of a blood donor and its components.” This order has been around for many years, but it does not need to be changed: our field of activity is quite conservative, and the provisions of the order are formulated quite universally.
Yes, now in global practice there is a tendency to soften contraindications for blood donation. This is quite reasonable: every year it becomes more and more difficult to find absolutely healthy donors. The most severe contraindications still remain severe somatic diseases, a history of cancer, as well as hepatitis, HIV, and syphilis. But neurological diseases, for example, are no longer considered such a strict contraindication: it all depends on the manifestations and severity of the disease. This also applies to other features of the donor’s body. Previously, a strict contraindication was, for example, the presence of piercings or tattoos; We are currently looking for an opportunity to examine the donor and, if no dangerous signs are identified, he will be allowed to donate.
What to do if controversial issues arise during the examination of a potential donor by a transfusiologist?
If during the examination a contradiction is revealed between the information that the donor gives about himself and the opinion of the transfusiologist, the decision on donation will be postponed for a short time, and the potential donor will be given a referral for additional examinations. For example, if a transfusiologist sees a postoperative scar on a donor, he should refer him for a consultation with a surgeon. The surgeon will give his opinion, which will help the transfusiologist make the final decision. Even though this is a rather complex scheme, sometimes completely harmless conditions can pose a threat both to the donor himself and to all blood recipients.
How do donors usually feel when they are refused a donation?
As a rule, our employees are ready to explain to the donor in detail and with reason why such a decision was made in relation to him. Most often, donors agree with our decision. In addition, each such precedent becomes a reason for a detailed self-examination - as a result, a serious illness can be identified.
What happens if the donor test done at your center turns out to be really alarming? Do you inform the donor that you have found something serious in his tests?
Yes, of course, and we report such news only personally – but we definitely report it. That’s why it’s so important that all our donors leave their current contact information in the form!
If a donor's analysis raises concerns, we invite him to our center privately and have a personal, private conversation. The only exception is when we receive a positive HIV test. In this situation, we are obliged to send a blood sample to the MHC AIDS for verification - and, accordingly, the MHC staff will communicate with the donor. There are often cases when we get false positive results. For example, it happens that a female donor has a false positive reaction to syphilis, and this is associated with early pregnancy.
What to do if your tests are positive? Will a person be able to become a donor again after undergoing treatment?
There is a clear algorithm for restoration of donation - if we are not talking about absolute contraindications. Most often, this is a matter of repeating the test after a certain period - and after that you can donate blood again.
Is it true that when donating blood for the first time, a donor cannot receive payment for it?
Yes, that's absolutely right. The first donation – if the person has never been registered as a donor anywhere before – is always free. Further, the donor can follow one of two paths provided by the Moscow healthcare system. The first way is paid donation, regulated by orders and law. To become a paid donor, you need to undergo a fairly extensive examination. As a rule, paid donors are carriers of a rare phenotype or donors with negative Rhesus. Usually the blood of these donors is extremely important, we even personally ask them to come and donate blood from time to time.
The second type of donation is using measures of social support for the population. This process is regulated by Resolution No. 51 of the Moscow Government: starting from the second donation, a donor with any blood type, even the most common, can take advantage of all support measures, receive them in the department where he donated blood - on the day of donation or through a savings system.
Is it true that you feed donors before and after donation?
Before donation, we give each donor sweet tea and cookies. This procedure is not enshrined in law, but it has a long history and is of great importance: its main task is not to feed, but to relax and reassure the donor. After a glass of sweet tea, donating blood is much easier to tolerate. After donation, the donor is indeed supposed to replenish the body’s resources, but we do not feed, we only provide compensation for food. This is much more convenient, since, firstly, each donor has his own tastes and his own diet, and secondly, the given set of food products would be quite cumbersome.
Is it true that sometimes the blood service can refuse to donate to a visiting donor not for medical reasons, but simply because you have such blood in excess?
Cases of such a refusal are quite rare, but, indeed, sometimes it happens that in a given particular department a certain blood group is available in excess. I would advise donors to carefully follow the “traffic light” on the website of our center and the blood service of the FMBA of Russia. Green color means there is a lot of such blood in this department. Yellow – may end soon. Red – this kind of blood is really needed. You can choose a department where your blood will be accepted with open arms.
Is it true that sometimes a donor has to wait in a long line before he can donate blood?
Yes, this happens: our center is also open on weekends, and many Muscovites can only donate blood on weekends. But in fact, only those donors who came to donate on a first-come, first-served basis will have to wait a long time. Those who use the pre-registration system wait much less.
If you are going to donate blood, how much time should you budget for the entire process?
Be prepared for the fact that, taking into account all the formalities, the blood donation process will take at least four hours. Firstly, the donor needs time to fill out a detailed questionnaire, select a measure of social support, undergo an examination, and prepare for donation. Secondly, even if you have always tolerated donation easily, it is worth allowing a little time for unforeseen reactions, mild illness, etc. Donors who donate platelets and plasma are given a medical certificate that will allow them not to come to work on the day of donation.
We know that for many citizens it is important to receive the title of an honorary donor of Moscow, as well as an honorary donor of Russia. Does presentation for an award always take place in a formal atmosphere?
According to the established procedure, the title of honorary donor is actually awarded in a solemn atmosphere. However, here everything depends on the wishes of the donor himself. We are often asked that all formalities be resolved as quickly as possible so that we can receive the certificate in hand and not waste time on the ceremony. There are others - those who require official recognition. For such donors, we will definitely organize a ceremony to award the title. It seems to me that, regardless of the chosen style, the honor of the donor is not diminished in any way: it’s not about who presented you with the award and badge and in what room. It's about how many lives you end up saving.
Contraindications
This is a complex and risky procedure. In case of failure, a number of violations of vital processes in the body will occur. Therefore, doctors always take this issue seriously. They examine diseases and information about transfusions that have already been given to the patient.
The procedure is contraindicated in patients with defects and other serious heart diseases. For disorders of blood flow in the vessels of the brain and protein metabolism in the body, for allergies.
Often, even in the presence of contraindications and serious diseases that require a transfusion, doctors perform this procedure. But at the same time, they prescribe drugs to the patient to prevent diseases that may appear after it.
Therefore, to the question of which blood group is most in demand in modern donation, the answer is ambiguous. Since only the native group is transfused to the recipient, and there are more people with I (0) Rh+, and transfusions are given to them more often, it is in demand. And there are much fewer people with IV (AV) Rh+ or -, but if a person with such a group needs a transfusion, finding a donor will be problematic.